At the age of 39, I faced the diagnosis of vulvar cancer, an uncommon cancer usually described as affecting postmenopausal women. Surviving a radical vulvectomy 30 years ago was just the beginning of my journey. This surgery involved removal of my clitoris, vulva, and groin lymph glands due to vulvar cancer, an experience that profoundly altered my life. The subsequent six weeks of pelvic radiation therapy induced menopause at the age of 42. I cannot begin to describe those first two years and discovering the taboos and stigmas associated with the word ‘vulva’.
Coincidentally, I met with a woman who experienced the same diagnosis and journey eight months previously. I remember this meeting so well, she lifted her dress, and I lifted mine and there we realised, we were on the same page. We had both requested our medical professionals to connect us with others battling vulvar cancer, but we had both been advised against doing so because ‘it would be too depressing’. There were no support groups for women navigating the post-operative journey after radical vulvectomy. This was my turning point. Feeling all alone and ostracised by society I placed an advertisement in a women’s magazine seeking others with whom I could talk. I received 38 responses, from women all over Australia, facing the same sense of isolation and embarrassment that I was experiencing.
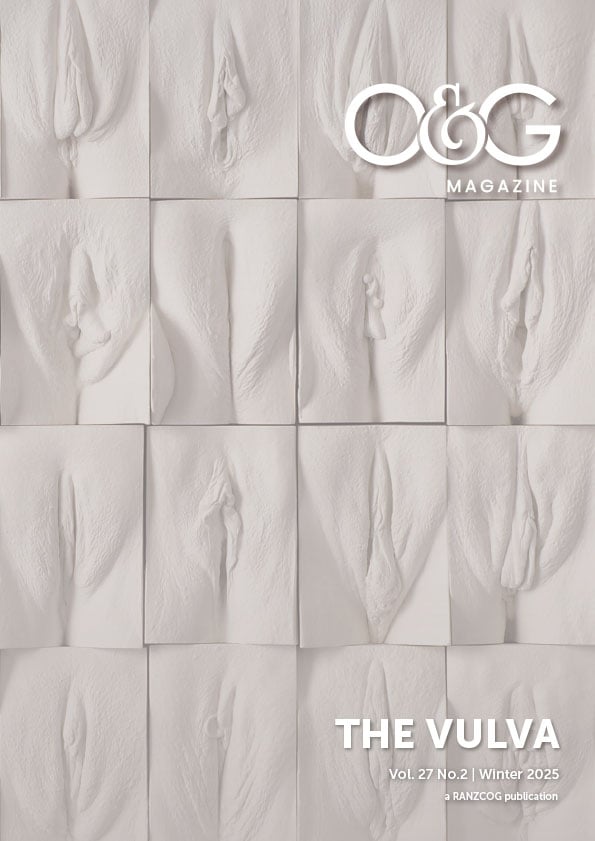
This compelled me to try to understand what made women fearful of speaking out about their symptoms and diagnosis. At the time, most women did not know the difference between ‘vagina’ and ‘vulva’. How could they, when even gynaecological cancer brochures did not include a diagram or picture of a vulva. In 2005, I presented my story to the New South Wales Cancer Council questioning the absence of a diagram of a vulva in their brochures. They took my feedback on board and have since updated their brochure to include a vulva that is appropriately represented. Other states followed suit. Sadly though, even today, reproductive health brochures, aimed at women, often have diagrams of the uterus, cervix and vagina but they do not include a vulva. I have made it my mission to increase awareness of vulvar cancer, among both women as well as health professionals, by destigmatising the use of correct terminology.
- Dare to be Vulva Aware
- Viva la Vulva
I have been told that vulvar cancer is rare and often diagnosed late because of its ‘intimate’ nature.1 Of these, many are young, like I was when I received my diagnosis, and many die of this devastating cancer because of the late diagnosis. And it is not just vulvar cancer. It is also other vulvar conditions like lichen sclerosus, another condition that gets overlooked despite one in 80 women suffering from it. Women themselves feel embarrassed to ask for help for vulvar issues. Medical professionals can also be reluctant to examine the vulva. When they do, they often lack the knowledge and experience to accurately diagnose vulvar conditions. I often hear from women how they were misdiagnosed as having thrush instead of lichen sclerosus or cancer of the vulva.
My entire life, since my diagnosis, has been focused on empowering women to embrace their bodies, especially their vulvas, and have open conversations about vulval symptoms like itching, discharge, skin discolouration, and lumps and bumps, and to seek help early. I want health professionals to take women’s symptoms seriously, to expand their knowledge of vulval diseases and educate women on vulval health. I feel we can only do this if we use accurate terminology, hence my insistence on using the word ‘vulva’. Not vagina, vulva.
- Alone we sit, together we make a mighty roar
When I first started to talk about the vulva, I was told it was an offensive word, and that it would be better to say ‘vagina’. That made no sense to me. The vagina and vulva are two different parts of the body. One is internal, the other is external. We do not call a man’s penis his testicles! How can women talk about their body accurately if they do not know the correct words to use? Hence, I started my ‘Red Knickers’ campaign with the tagline ‘Viva la Vulva’ and advocated for 10 September to be celebrated as International Gynaecological Awareness Day (IGAD). King Edward Memorial Hospital in Western Australia has celebrated IGAD for the past nine years. My advocacy has been recognised with many awards, but awards are superfluous in the absence of action. In 2018, I was selected as Western Australia Senior Australian of the Year. This only spurred me to continue my advocacy.
Despite the challenges, and being a multiple award recipient, I remain steadfast in my mission to ensure that women with vulvar health issues receive the attention and care they deserve and that research into vulvar cancer receives the same funding as breast cancer or ovarian cancers. My journey is a testament to the resilience and determination necessary to effect change in this critical area of women’s health. This is a new world with women demanding old stigmas and taboos be broken. It is time to shine a light on this silent suffering and I will continue to be the voice of women who are afraid to speak out about vulvar issues. To learn more about the author, visit: kathmazzella.com.
References
- AIHW (Australian Institute of Health and Welfare) 2024. Cancer data in Australia [web report] December 2024 release.








Leave a Reply