As health professionals, we are responsible for providing women and their support people with clear, relevant evidence-based and individualised information to guide their discussions about their choices and decisions.
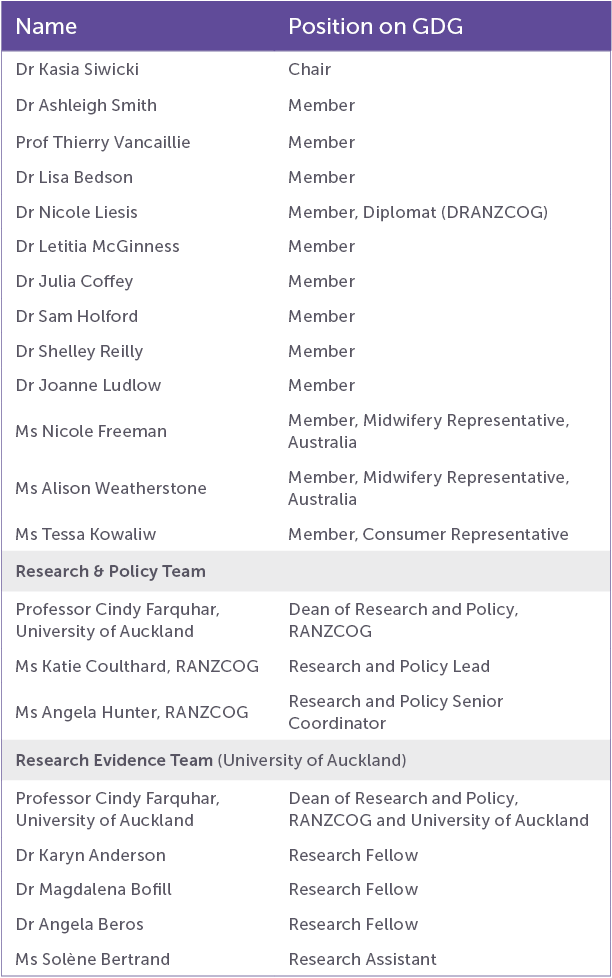
In April, as part of an ongoing review and update of College statements and guidelines, RANZCOG published the Miscarriage, Recurrent Miscarriage and Ectopic Pregnancy Clinical Guideline (C-Gyn 38). This important guideline has been prepared using the same evidence-based approach to developing and updating Clinical Guidance Statements that RANZCOG has adopted since 2020, in a collaborative process overseen by the RANZCOG Women’s Health Committee (WHC) and internally funded by RANZCOG. The work was spearheaded by the outstanding RANZCOG Research and Policy Team (RAPT) alongside the multi-disciplinary Guideline Development Group (GDG), with public consultation and input sought from RANZCOG members, key stakeholders, and consumers to ensure the guideline is reflective of current knowledge, practices, and perspectives.
The scope and clinical questions (formulated by the RAPT and GDG, with review by the WHC) address specific clinical, diagnostic and therapeutic challenges that clinicians encounter commonly in early pregnancy care, and less familiar conditions that are, nonetheless, associated with a significant clinical or personal implications. In line with other updated RANZCOG guidelines, this guideline was developed following accepted international processes according to the National Health and Medical Research Council (NHMRC) and Grading of Recommendations Assessment, Development and Evaluation (GRADE) processes and meets the criteria of the Appraisal of Guidelines for Research & Evaluation (AGREE) II framework.
Because this is a guideline intended for practitioners in Australia and Aotearoa New Zealand, the clinical practice advice it provides has also been shaped by the views of the GDG and stakeholder feedback, with consideration for the varied settings and situations in which the RANZCOG members and the women they care for reside across the two countries.
The application of these guidelines can inform the clinical foundation of a trusting therapeutic relationship and patient-centred care, but the practice of that care also draws on experience, beliefs and empathy with the individual’s situation. The importance of these aspects of care were emphasised repeatedly during discussions within the GDG and in the feedback received during the consultation process.
There is consistent messaging from consumers that clear and empathetic communication, appropriate language, culturally safe practices and an individualised approach are vital in the management of early pregnancy loss, due to the recognised impact of negative health-care interactions on patient experience and recovery.
Specific mental health interventions and comprehensive mental health management were deemed to be outside of scope for this guideline. And it is acknowledged that they may be outside the scope of practice of many members who nonetheless care for women and their support people experiencing pregnancy loss. Being familiar with resources and support networks, local grief counselling and mental health services and liaising with GPs can be part of every practitioner and organisation’s remit.
Resources
The guideline includes a list of resources identified during the guideline development process.
| Source | Name of resource |
|---|---|
| National Blood Authority Australia | Guideline for the prophylactic use of Rh D immunoglobulin in pregnancy care |
| New Zealand Blood Service | Use of Rh D Immunoglobulin (Anti-D Immunoglobulin) During Pregnancy and the Post Partum Period (111G130) |
| Tommy’s National Centre for Maternity Improvement UK | Tommy's Miscarriage Support Tool |
| Pink Elephants Support Network | The Pink Elephants Support Network - Home |
| Red Nose Foundation | Home | Red Nose Australia |
| Miscarriage Australia | Miscarriage Australia - Navigating miscarriage together |
| Sands New Zealand | Sands New Zealand - Pregnancy, Baby and Infant Loss Support, New Zealand |
| Whetūrangitia – online service supporting bereaved parents and whānau in Aotearoa New Zealand | Information for bereaved family and whānau experiencing the death of a baby or child | Whetūrangitia |
Table 1. Excerpt from Miscarriage, Recurrent Miscarriage and Ectopic Pregnancy (C-Gyn 38) p. 74
| National Blood Authority Australia | Guideline for the prophylactic use of Rh D immunoglobulin in pregnancy care |
| New Zealand Blood Service | Use of Rh D Immunoglobulin (Anti-D Immunoglobulin) During Pregnancy and the Post Partum Period (111G130) |
| Tommy’s National Centre for Maternity Improvement UK | Tommy’s Miscarriage Support Tool |
| Pink Elephants Support Network | The Pink Elephants Support Network – Home |
| Red Nose Foundation | Home | Red Nose Australia |
| Miscarriage Australia | Miscarriage Australia – Navigating miscarriage together |
| Sands New Zealand | Sands New Zealand – Pregnancy, Baby and Infant Loss Support, New Zealand |
| Whetūrangitia – online service supporting bereaved parents and whānau in Aotearoa New Zealand | Information for bereaved family and whānau experiencing the death of a baby or child | Whetūrangitia |
How, where and who provides care during the deeply personal and emotional experience of pregnancy loss, and the management of conditions that contribute to it, has evolved. In reviewing the evidence, the GDG has identified areas for future research, aimed at helping to ensure that the evolution of our approach to care continues to meet the needs of our patients.
Further research priorities
- Intrauterine adhesions (IUAs) – incidence following uterine instrumentation, impact and treatment options
- Late miscarriage (pregnancy loss between 13–20 weeks) studies to test the effectiveness, safety, and acceptability of medical and surgical management, and options for pain management
- The role of screening for ANA, sperm DNA fragmentation and B2GP1 antibodies in recurrent miscarriage patients
- Evaluating the best thresholds for diagnosing subclinical hypothyroidism
Recommendations and further research points are excerpted from Miscarriage, Recurrent Miscarriage and Ectopic Pregnancy (C-Gyn 38) pg 73
We all hold out for the gold-standard of early pregnancy care in well-resourced, dedicated early pregnancy units with specially trained multi-disciplinary staff but acknowledge that this is difficult to realise, universally, across all of Australia and New Zealand. There are the grinding practicalities of funding, staffing and training. And the challenges of creating a level playing field for all consumers regardless of rurality, remoteness, orientation, background, beliefs or language.
RANZCOG invests time and effort in producing up to date guidance for its members so that best outcomes can be achieved in the hands of compassionate clinicians working collaboratively with colleagues in providing care for well-informed women and their support people.





Leave a Reply