Case study
An 80-year-old woman presented to the gynaecologist with red, tender urethral caruncles (see Figure 1). Her recent history included a urinary tract infection (UTI) and genital rash, treated with antibiotics and topical steroid treatment along with a recent hip replacement following an osteoporotic fracture. Initiation of topical oestriol therapy led to notable improvement of her symptoms within just three days. She was advised to continue the topical oestrogen therapy, highlighting its potential to address her presenting symptoms effectively. Low oestrogen levels postmenopause can contribute to all the symptoms that this patient experienced.
Urethral caruncles can develop due to the lower elasticity and strength of the urethral tissues leading to discomfort.1 Low oestrogen levels changes the vaginal flora and weakens the bladder muscle which leads to increased postvoid residual volume that can lead to the development of urinary tract infections (UTIs) and/or urinary incontinence.2 Recurrent UTIs can also be a major source of morbidity through its effect on quality of life and the increased incidence of delirium, indication for antibiotics which can have gastrointestinal and microbiome side effects as well as the increase in vaginal thrush, and possibility for complications that can lead to hospitalisation such as pyelonephritis and sepsis.3

Figure 1. Vulva with urethral caruncles. Photo shared with patient permission
Introduction: the overlooked solution
For many postmenopausal women, symptoms associated with genitourinary syndrome of menopause (GSM) – such as vulvo-vaginal dryness, dyspareunia, bleeding, recurrent UTIs and urological urgency, while common, are often underdiagnosed or dismissed as an inevitable part of aging. However, they can significantly impact quality of life. A simple, evidence-based intervention exists: topical oestrogen such as Ovestin cream or pessary, and Vagifem pessary, as seen in Table 1 below.4 Despite proven efficacy and safety, barriers including prescription requirements and societal stigma continue to limit treatment access.
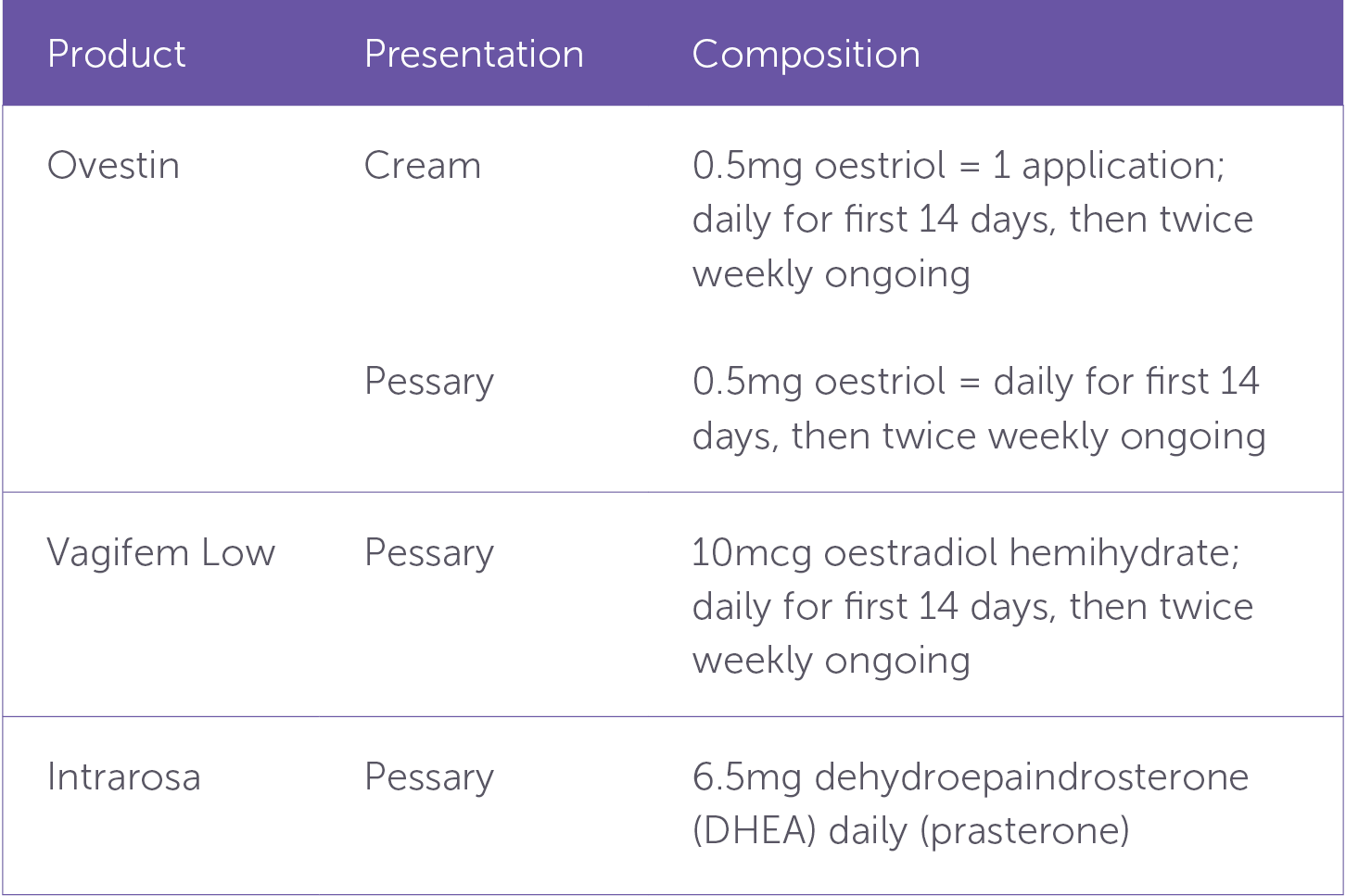
Table 1. Vaginal Therapy options from the Australian Menopause Society4
The importance of oestrogen
Oestrogen plays a crucial role in maintaining the health of vulvovaginal and lower urinary tract tissues. As women approach and reach menopause, oestrogen production from the ovaries decreases and eventually ceases. Some levels of circulating oestrogen remain through the aromatisation of androgens from the ovaries, adrenal glands, and adipose tissue however the levels will never be as high as they previously were before menopause.5
This decline in oestrogen levels leads to thinning of the vaginal epithelium, decreased blood flow, and loss of elasticity. This contributes to symptoms such as dryness, irritation, and dyspareunia. Additionally, the urethra and bladder, which also have oestrogen receptors, become more susceptible to infections and urgency issues due to the increased bacterial colonisation from an increased vaginal pH resulting from decreased oestrogen.5
Topical oestriol directly replenishes local oestrogen levels with minimal systemic absorption, distinguishing it from systemic hormone replacement therapy (HRT), which circulates throughout the body. Topical formulations deliver the hormone directly to the affected tissues leading to a lower risk profile. While the vaginal lining is atrophic, there may be a tiny increase in serum estrogen levels however this quickly subsides.5 Literature reviews that inform clinical guidelines have demonstrated that regular use of topical vaginal oestrogen significantly reduces recurrent UTIs, improves vaginal moisture and elasticity by thickening and maturing the vaginal wall, alleviates dyspareunia, and decreases urgency-related urinary symptoms.5,6,7
The case for accessibility: over-the-counter availability
Currently in Australia, topical oestrogen remains prescription-only, unlike the UK where low-dose vaginal oestrogen (Gina vaginal tablets) and Ovesse (vaginal cream) can be accessed following pharmacist consultation, reflecting a growing recognition of its safety and necessity. This is a similar idea to the distribution of fluconazole which is available with a pharmacist consultation for the treatment of vaginal thrush in many countries including Australia. Like postmenopausal syndrome, vaginal thrush is a common condition with a high safety treatment profile with pharmacist guidance to ensure proper usage. These secondary prevention strategies are also more efficient for how resources are used in the healthcare system, freeing up time and cost for general practitioners and specialists.
Several compelling arguments support improving accessibility. The safety profile of topical oestrogen is well-documented, with negligible systemic absorption and minimal risk compared to systemic HRT. The Australian Menopause Society reports that 27% of women using systemic hormone therapy still experience symptoms of GSM and so it should not be overlooked in these patients.8 While certain groups of women may be less ideal candidates, such as those with histories of gynaecological cancers, this can be screened for by a pharmacist.
However, a systematic review showed that patients who have had breast cancer in the past and used vaginal oestrogen did not have an increased rate of breast cancer recurrence, breast cancer mortality, or overall mortality.9 Moreover, many women avoid healthcare consultation due to embarrassment, lack of awareness, or difficulty accessing healthcare providers. Approximately 50% of postmenopausal women experience symptoms associated with GSM resulting from decreased oestrogen; however less than seven percent are given safe oestrogen therapy.10 Allowing over-the-counter access could significantly increase awareness of available treatments and empower women to take control of their health and quality of life.
A call to action: increasing access to topical oestrogen
Advocating for regulatory changes to allow over the counter access to topical oestrogen in Australia is a step towards addressing the unmet needs of many women. Research suggests only 4.5-7.8% of peri and postmenopausal Australian women are using vaginal oestrogen, despite the substantial proportion who would likely benefit.8 Creating awareness around vulvovaginal and urological health is crucial for women to access and benefit from safe treatments. Enhanced accessibility would represent a significant stride in recognising the unnecessary suffering many women are experiencing and advancing women’s health and wellbeing.
Conclusion
Topical oestrogen is a safe, effective, and underutilised treatment for managing postmenopausal vulvovaginal and urological symptoms. Given its minimal risks and substantial benefits, there is a strong case for making it available over the counter with pharmacist guidance, as seen in the UK. By prioritising accessibility and awareness, we can empower women to take control of their health and improve their quality of life with a simple, evidence-based solution.
References
- Patel, U. J., Moureau, M. K., Neuner, J. M., & Brown, H. W. (2023). Screening and treating urinary incontinence in primary care: A missed opportunity. OBM Geriatrics, 07(04), 1–16.
- Aggarwal, N., & Leslie, S. W. (2025). Recurrent Urinary Tract Infections. In StatPearls. StatPearls Publishing.
- Rodriguez-Mañas, L. (2020). Urinary tract infections in the elderly: A review of disease characteristics and current treatment options. Drugs in Context, 9, 1–8.
- Grainger, S. (2025, March 10). AMS Guide to MHT/HRT doses Australia only. Australasian Menopause Society.
- Peacock, K., Carlson, K., & Ketvertis, K. M. (2023). Menopause. In StatPearls. StatPearls Publishing.
- Hirschberg, A. L., Bitzer, J., Cano, A., Ceausu, I., Chedraui, P., Durmusoglu, F., Erkkola, R., Goulis, D. G., Kiesel, L., Lopes, P., Pines, A., van Trotsenburg, M., Lambrinoudaki, I., & Rees, M. (2021). Topical estrogens and non-hormonal preparations for postmenopausal Vulvovaginal Atrophy: An emas clinical guide. Maturitas, 148, 55–61.
- Valdes, A., & Bajaj, T. (2023). Estrogen Therapy. In StatPearls. StatPearls Publishing.
- Grainger, S. (2024, October 29). Genitourinary syndrome of Menopause. Australasian Menopause Society.
- Beste, M. E., Kaunitz, A. M., McKinney, J. A., & Sanchez-Ramos, L. (2025). Vaginal estrogen use in breast cancer survivors: a systematic review and meta-analysis of recurrence and mortality risks. American journal of obstetrics and gynecology, 232(3), 262–270.e1.
- Davis, S., & Magraith, K. (2023). Advancing Menopause Care in Australia: Barriers and opportunities. Medical Journal of Australia, 218(11), 500–502.






Leave a Reply