Vulval dermatology is a niche but essential subspecialty that sits at the intersection of dermatology, gynaecology, urology and sexual health1. As a dermatologist with a special interest in vulval skin conditions, I have witnessed firsthand the profound effects that vulval dermatological disorders can have on women’s quality of life. For many patients, these conditions not only cause physical discomfort but can also lead to emotional distress, making early diagnosis and proper management vital. This article outlines my journey into vulval dermatology, highlights treatment challenges, and reviews common vulval skin conditions that require expert care.
My journey into vulval dermatology
My journey into vulval dermatology began during my first year of dermatology training, where I had the privilege of working under the mentorship of Associate Professor Amanda Oakley who is a leading expert in the field of vulval dermatology. I was fortunate enough to attend her weekly vulval clinics. The sense of validation women experienced upon finally receiving a diagnosis-and the immense impact on their quality of life once adequately treated-was inspiring. This experience solidified my interest in the field long after completion of my dermatology training.
Vulva as skin of special site
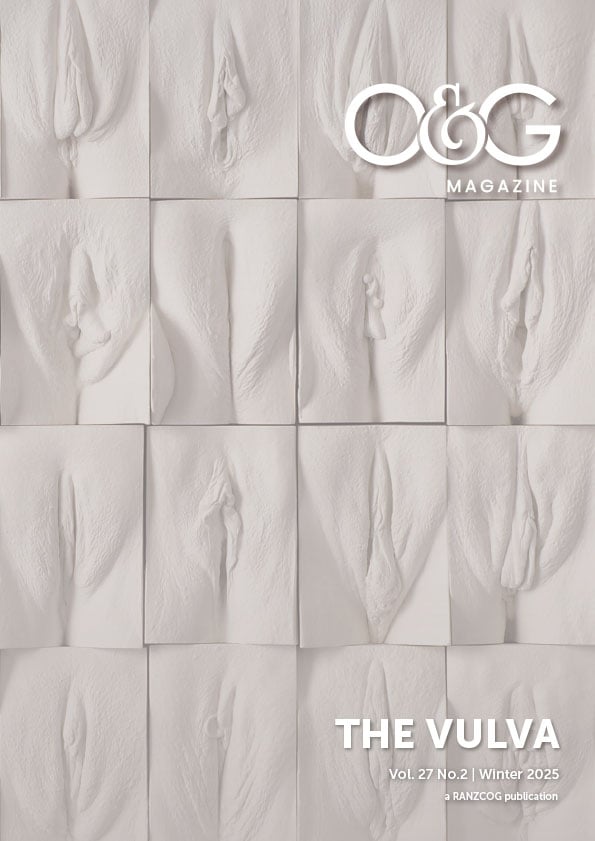
The vulva consists of three distinct types of skin: mucosal, intertriginous, and cutaneous. The mucosal skin — including the inner labia minora and the vestibule — is non-hair bearing and more delicate than other skin types. The labia majora and surrounding areas, on the other hand, have cutaneous skin, which is similar to the skin found on other parts of the body. Additionally, the inguinal regions where the skin touches skin (e.g., the folds between the labia majora) are classified as intertriginous skin which is more susceptible to the effects of occlusion, friction and sweat. When assessing vulval skin conditions, it is crucial to identify which type of skin is involved, as this can greatly influence both the diagnosis and the treatment plan.
The vulva is also unique in that it has a limited way in which rashes can appear – with a cursory look every condition can look similar! For example, psoriasis on the elbow typically presents as a well-demarcated erythematous plaque with silvery scales, but psoriasis on the vulva appears erythematous without the characteristic scales. Despite these diagnostic limitations, some general guidelines can assist clinicians. Erythematous rashes are often seen in conditions like eczema, psoriasis, tinea, or candida. White patches or pallor may suggest lichen sclerosis, lichen simplex, vitiligo, or even malignancy. Ulcers and erosions are typically indicative of lichen planus, autoimmune blistering diseases, or aphthous ulceration. A thorough assessment of other areas of the body, including the scalp, face, flexures, extensors, and nails, can offer valuable clues to help differentiate these conditions.
The importance of vulval skin care
When managing vulval dermatological conditions, skin care plays a critical role. It is essential to take a detailed history to understand what products are being used on the vulva. Over-the-counter products, such as perfumes, soaps, and hygiene wipes, can often exacerbate existing skin conditions and contribute to irritant or allergic contact dermatitis. For example, patients with urinary incontinence may use pads that can irritate the vulval skin, while those with faecal incontinence may rely on wet wipes, which can cause similar issues.
In my practice, I often advise patients to use plain water or non-soap cleansers to cleanse the vulval area, as they are less likely to cause irritation. I also emphasise the importance of not over-washing, as excessive washing can disrupt the skin’s natural barrier and exacerbate inflammation. I recommend loose-fitting underwear made from breathable materials such as cotton or silk to reduce friction and moisture accumulation, both of which can contribute to vulval skin irritation.
When prescribing treatments, I generally prefer ointment formulations for delicate mucosal areas, as they have no water content and do not contain preservatives, making them less likely to irritate. In contrast, creams and lotions can cause a burning or stinging sensation due to their higher water content and added preservatives. However, care must be taken when applying ointments to hair-bearing areas, as they can cause occlusion and folliculitis. Additionally, while topical steroids are often used to treat inflammatory vulval skin conditions, they can lead to side effects such as steroid-induced rosacea, periorificial dermatitis, infections like herpes or candidiasis and if not used properly can result in early and late changes of steroid-induced atrophy.
Common vulval skin conditions
The most common skin conditions referred to a vulval dermatology clinic are lichen sclerosus, eczema and psoriasis2. Other conditions often seen are lichen planus, hidradenitis suppurativa, peri-orificial dermatitis, granular parakeratosis, vitiligo and Zoon’s vulvitis.
Lichen sclerosus
Lichen sclerosus is a chronic inflammatory skin disorder that typically manifests as white, thickened patches on the vulva. This condition is often intensely pruritic, causing severe itching, which can lead to discomfort and pain, particularly during sexual intercourse. The active inflammation in lichen sclerosus may present as erythema, hyperkeratosis, erosions, and fissures. Over time, chronic lichen sclerosus can lead to scarring, labial fusion, and narrowing of the vaginal opening. Lifelong surveillance is necessary to monitor for potential development of vulvar squamous cell carcinoma, as there is an increased risk of malignancy associated with the condition.
Vulval eczema
Vulval eczema encompasses a range of conditions, including atopic dermatitis, irritant contact dermatitis, allergic contact dermatitis, seborrheic dermatitis, and lichen simplex3. Atopic dermatitis is often associated with a personal or family history of asthma, hay fever, or eczema elsewhere on the body. Irritant contact dermatitis occurs when a substance, such as soap or water, repeatedly encounters the vulval skin, causing irritation. Contact allergic dermatitis requires a high degree of suspicion and keeping up to date with the common and emerging contact allergens. If unable to be elicited on history, formal patch testing is necessary to evaluate contact allergic dermatitis. Lichen simplex is a neurogenic type of eczema where there is a perpetual itch scratch cycle that leads to thickened and leathery skin with accentuated skin markings. Underlying causes of the initial pruritus/trigger can be varied.
Vulval psoriasis
Psoriasis on the vulva often presents as erythematous plaques on the labia majora, which may extend into the inguinal, perianal, or gluteal cleft areas. Unlike psoriasis on other parts of the body, vulval psoriasis may not present with the characteristic silvery scale. However, a careful history and examination of other parts of the body (e.g., the scalp, nails, and elbows) can provide important diagnostic clues. Vulval psoriasis that does not respond to intermittent use of mild to moderate potency topical steroids may require systemic treatments, especially if symptomatic. Adjuvant topical treatments commonly used in cutaneous psoriasis-such as tar, calcipotriol, salicylic acid-are typically too irritating for the vulval area and treatments such as phototherapy are not possible.
Granular parakeratosis
Granular parakeratosis is a condition that affects the intertriginous areas of the vulva, often in middle-aged women. It is thought to be triggered by friction, occlusion, and sweating, which alters the skin’s microbiome. This leads to red-brown patches and desquamation of the skin. Although previously uncommon granular parakeratosis has increased in incidence in recent years especially during the Covid pandemic due to widespread use of antiseptic laundry products containing benzalkonium chloride. Treatment typically involves the use of mild to moderate topical steroids to reduce inflammation, along with oral antibiotics to restore the skin’s natural microbiome and keratolytic agents to manage desquamation.
The role of multidisciplinary care and resources
Given the complexity of vulval dermatology, a multidisciplinary approach is often required, particularly for patients with complex or treatment-resistant conditions. In many cases, gynaecologists, sexual health physicians, physiotherapists, sex therapists, and psychologists may be involved in the care of these patients. Vulval clinics, often found in tertiary centres, are invaluable for providing comprehensive care to women with complex vulval dermatological issues. These clinics offer coordinated care that addresses the physical, emotional, and psychological aspects of vulval health.
Several resources are available to both healthcare professionals and patients. The Australian and New Zealand Vulvovaginal Society (ANZVS) is an excellent resource for those involved in the care of women with vulval conditions4. Additionally, websites like caredownthere.com.au and dermnetnz.org provide up-to-date information on vulval dermatology, and they serve as educational tools for both patients and health professionals5,6.
Conclusion
Vulval dermatology is a vital field that significantly impacts the lives of women. As dermatologists, gynaecologists, and other healthcare providers, we can make a profound difference in the lives of women affected by vulval skin conditions. Through early diagnosis, proper treatment, and a multidisciplinary approach, we can help patients regain comfort, confidence, and quality of life.
References
- Brägelmann C, Wölber L, Susok L, Anemüller W, Prüßmann W, Ivanova I, Niebel D. Update vulval dermatology – diagnostics and therapy. J Dtsch Dermatol Ges. 2025 Jan;23(1):65-86.
- Warner S, Oakley A. Vulval dermatoses: A review of referrals to dermatology. Australas J Dermatol. 2024 May;65(3):268-271.
- Pichardo-Geisinger R. Atopic and Contact Dermatitis of the Vulva. Obstet Gynecol Clin North Am. 2017 Sep;44(3):371-378.
- anzvs.org
- caredownthere.com.au
- dermnetnz.org





Leave a Reply