The most common causes1 for any form of vulval discomfort and dyspareunia across all age groups are contact dermatitis, chronic vulvovaginal candidiasis, psoriasis, and lichen sclerosus. However, there are certain conditions that occur more frequently in older women than in younger age groups.
Lichen sclerosus
Vulval and peri-anal lichen sclerosus (LS) is common, impacting around 1 in 300 women. Two thirds of patients are over the age of 50 at presentation. Although association with thyroid disease and vitiligo may be more prevalent than in age-matched controls, LS itself is not thought to have an exclusively autoimmune aetiology.
In addition to the management of symptoms and prevention of scarring, adequate treatment of lichen sclerosus is essential to mitigate the five percent lifetime risk of squamous malignancy2.
Lichen sclerosus typically presents with symptoms such as itch, discomfort, dysuria, and dyspareunia. However, it may also be asymptomatic and identified during routine examination.
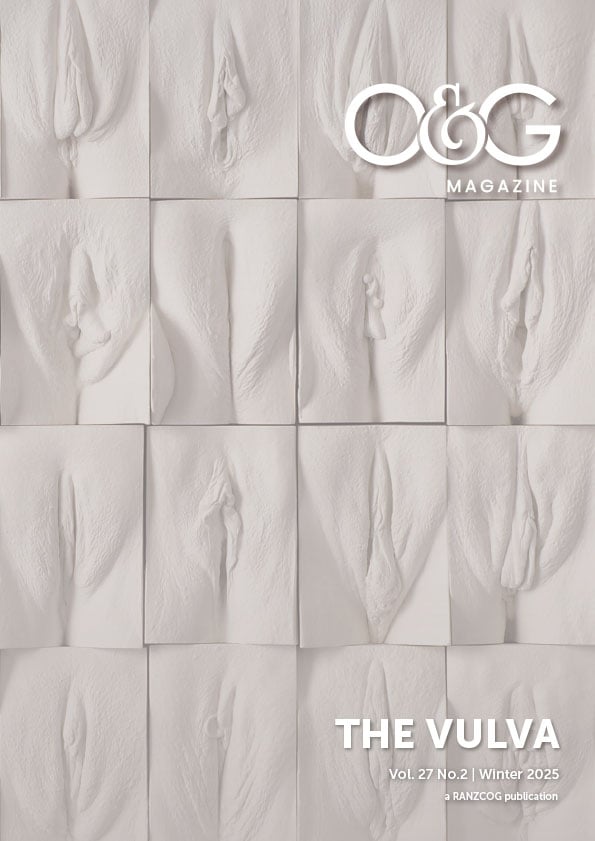
The classic examination findings are of thickened white vulval skin with alteration of vulval architecture. Because there are other skin conditions that may present with white thickened vulval skin (especially lichenified dermatitis or vulval intraepithelial neoplasia (VIN) biopsy is essential to confirm the diagnosis.
Topical corticosteroids (TCS), used continuously to maintain objective control of skin changes are the gold standard3. The potency is titrated against the thickness of initial skin changes. LS is very unlikely to remit, but the careful long-term use of appropriate TCS is very safe and effective.
Oestrogen deficiency
Although all women, if their lifespan allows, will reach menopause, not all women will become symptomatic of menopausal oestrogen deficiency. Despite this observation, topical oestrogen therapy is frequently prescribed as a blanket tool for vulval discomfort without considering alternative diagnoses.
Atrophic vaginitis caused by oestrogen deficiency can cause the same symptoms as many other vulval dermatoses and older women who experience atrophic vaginitis are also more likely to suffer from neuropathic vulval pain4. Additionally, many women experience menopausal symptoms alongside other vulval skin disorders.
There can be a great deal of overlap in examination findings between oestrogen deficiency and other vulvo-vaginal skin disorders. While some shrinkage of vulval structures can be due to menopause, adhesions, fusion, distortion, or significant resorption of structures are always caused by another skin disorder.
The specifics of topical oestrogen therapy will not be discussed here. The essential point however is that symptoms solely due to oestrogen deficiency will be promptly improved after an adequate trial of topical oestrogen. If the symptoms persist, another diagnosis should be considered.
Lichen planus
This is a rare condition, with a varied and sometimes changeable presentation making diagnosis challenging. Genital lichen planus can involve both the vaginal mucosa and vulval skin. Although uncommon, its higher prevalence in older women makes it an important consideration. Common presenting symptoms include pain, dyspareunia, and vaginal discharge. Women who do not practice vaginal penetration may be completely asymptomatic. There is an association between lichen planus and VIN5. Similar to lichen sclerosus, complete suppression of the disease effectively mitigates the risk of progression to squamous cell carcinoma.
The examination findings are highly variable. Skin changes include vaginal erosions, erythema, and adhesions, but thick white skin may be seen on the vulva. More rarely, ecchymoses can cause post-menopausal bleeding. While histopathological diagnosis is specific, it is not always sensitive; thus, clinical diagnosis is often necessary. Biopsy should be done if LS or VIN is suspected.
Lichen planus requires ultra potent corticosteroids to control symptoms and skin changes. One in five patients require oral immunosuppressants as well as topical therapy. This disease is often best managed in conjunction with dermatology or immunology colleagues.
Psoriasis
Psoriasis is common and affects women of all ages. Although psoriasis is neither unique to nor overrepresented amongst women following menopause, its variable presentation6 warrants consideration in any patient presenting with vulval discomfort. Psoriasis is usually intensely itchy and, in the vulva, does not always have the characteristic findings seen on skin elsewhere. A red rash extending into the natal cleft is common as are fissures across the vulval skin. Psoriasis does not cause vaginitis, but can coexist with candidiasis and in oestrogen deficiency, both of which may present similarly. Topical corticosteroids are usually effective for initial improvement and inducing remission. However, as a chronic, relapsing condition, maintenance therapy is usually required with steroid sparing agents and emollients. Optimising skin triggers like urinary incontinence, friction, heat, sweat and coexistent vulval dermatoses is essential to minimise flare-ups.
Neuropathic vulval pain
Vulvo-vaginal pain in the absence of a skin condition has long been a cause of confusion for clinicians. However, an approach which considers the close relations of the vulva and vagina to the bowel, spine and hips makes it easier to understand vulvo-vaginal pain and potentially help our patients. We think that most vulval discomfort in the presence of normal vulval skin is caused by neuromuscular dysfunction.
Lower limb pain referred from the spine is well known, as is bladder dysfunction referred from the spine and/or bowel. It is therefore plausible that vulvo-vaginal pain could similarly be associated with bowel and musculoskeletal diseases or dysfunction. Harris et al clearly established the role of neuromuscular contributions to vulval pain in the absence of a skin problem7. Commonly, the pain will be in a horseshoe shaped ring involving the inferior vulval structures and perineum. This has led to the concept of “pudendal nerve entrapment” as a cause for this type of pain. We think however, that relying on pudendal nerve dysfunction alone to explain vulval neuropathic pain is too narrow a concept and does not always help our patients.
Bowel dysfunction should be improved where possible, and dual-skilled musculoskeletal and pelvic physiotherapy and/or neuromodulating drugs may significantly improve this type of pain. Younger women in this category tend to improve with physiotherapy, while older women may benefit more from neuromodulating drugs. A detailed description of the safe use of such medications as amitriptyline, gabapentin, pregabalin or duloxetine is beyond the scope of this article.
Adjunctive therapies, such as psychology, can also be beneficial, along with encouraging a realistic approach to balancing exercise and rest appropriate to age and pathology.
Vulval discomfort in the post-menopausal state can occur due to several conditions, whether independently or in conjunction with each other. While often well intentioned, prescribing topical oestrogen as a universal remedy for vulval issues in older women can be harmful and should only be used when the treatment of oestrogen deficiency is likely to be of clinical benefit. Familiarity with age-appropriate vulval anatomy and function, as well as an understanding of vulval dermatoses across all ages is essential before then narrowing the focus of assessment to that of the post-menopausal woman.
References
- Bradford J, Presentation: the Aetiology of Vulval Pain. International Society for the Study of Vulvovaginal Disease World Congress, Portugal. 2001.
- Lee A, Bradford J, Fischer G; Long-term Management of Adult Vulvar Lichen Sclerosus: A Prospective Cohort Study of 507 Women. JAMA Dermatology. 2015 Oct; 151(10):1061-7
- Lee A, Bradford J, Fischer G; Long-term Management of Adult Vulvar Lichen Sclerosus: A Prospective Cohort Study of 507 Women. JAMA Dermatology. 2015 Oct; 151(10):1061-7
- Fischer G, Bradford J. The Vulva: A Practical Handbook for Clinicians 2nd Edition. Cambridge University Press 2016
- dermnetnz.org/topics/vulval-intraepithelial-neoplasia [accessed 16/03/2025]
- Shivam K, Bradford J, Fischer G. Vulvar psoriasis in adults and children: a clinical audit of 194 cases and review of the literature. Journal of Lower Genital Tract Disease. 2012 Oct; 16 (4): 364 – 71
- Harris V, Fishcer G, Bradford J. The Aetiology of chronic vulval pain and entry dyspareunia: a retrospective review of 525 cases. Australian and New Zealand Journal of Obstetrics and Gynaecology. 57 (4): 446 – 451






Leave a Reply