Abstract
Haemophilus influenzae is a rare pathogen in obstetric infections. This case report focuses on a 26-year-old female who presented at 14+3 weeks gestation with increasing lower abdominal pain following sudden vaginal fluid. Despite initial planning for expectant management of her second trimester miscarriage, the patient developed signs of sepsis with persistent fevers and worsening abdominal pain. Haemophilus influenzae was identified from both blood cultures and an intraoperative endocervical gel swab, necessitating targeted antibiotic therapy. This case highlights the importance of early recognition and treatment of sepsis in obstetric patients.
Introduction
Haemophilus influenzae is a gram-negative anaerobic bacterium commonly associated with respiratory infections.1,2 However, it is a rare pathogen that has previously been cultured in the female genital tract .1,2 This report presents a unique case of Haemophilus influenzae bacteraemia following a second-trimester miscarriage, which underscores the importance of broad-spectrum antibiotic coverage and multidisciplinary management in obstetric sepsis to prevent morbidity and mortality.3
Case Report
A 26-year-old female (G5P2M1T1) presented to the emergency department with worsening sharp right lower abdominal pain rated 8/10 in severity. This was following clear PV fluid loss, with a known intrauterine pregnancy. At the time of presentation, she was 14+3 weeks gestation. She denied symptoms such as fever, nausea, vomiting, urinary or bowel symptoms, or other systemic signs of illness, with no recent infectious contacts.
Past Medical and Surgical History:
- Alpha thalassemia trait
- Anxiety
- Previous appendicectomy
Obstetric History:
- 2x spontaneous vaginal deliveries
- 1x first-trimester miscarriage
- 1x medically managed termination of pregnancy
Initial Investigations:
- Full Blood Count: Elevated white cell count (WCC) of 18.5 × 10^9/L, otherwise no abnormality.
- C-reactive protein (CRP) of 46, indicating an inflammatory/infectious process.
- Other blood tests including electrolytes, liver, and renal function were within normal reference range.
- Pelvic Ultrasound: Confirmed intrauterine fetal demise at 14+3 weeks, normal liquor volume, posterior placenta, and closed cervix (35mm), normal ovaries and adnexa.
Management Course:
- Given significant pain, the patient was admitted and management options were discussed in accordance with the Queensland Health Stillbirth Guideline.4
- Initially, the patient was opted for expectant management and began to have palpable contractions.
- The patient’s pain was increasing in the right lower quadrant and was no longer able to be controlled with oral analgesia. She was commenced on patient-controlled fentanyl analgesia (PCA) with the assistance of the anaesthetics team.
- Despite the PCA, she had persistent pain and laboratory evidence of infection. Empiric IV antibiotics (gentamicin, ampicillin, and metronidazole) were initiated due to concerns for sepsis.
- Within 30 minutes of starting antibiotics (only gentamicin administered at this time), she developed a fever of 38.2°C.
- Repeat blood tests showed a persistently elevated WCC (17.3 × 10^9/L). Blood cultures were collected at the time of the fever.
- Due to clinical deterioration and ongoing pain, the obstetric team recommended an urgent suction dilation and curettage +/- extraction (D&C) under ultrasound guidance, which was performed without complication.
- Routine intraoperative investigations included an endocervical swab for microscopy/culture/sensitivity (M/C/S).
Postoperative Course:
- Despite surgical intervention, the patient continued to experience fevers and abdominal pain.
- CT abdomen/pelvis revealed no significant findings.
- Antibiotics were escalated to IV piperacillin-tazobactam 4g every six hours per local sepsis protocol.
- Blood cultures returned positive for Haemophilus influenzae (beta-lactam positive) in two sets at 13 and 18 hours. (Figure 1)
- Infectious diseases specialists initially considered the blood culture result to be a contaminant. However, on postoperative day three, the intraoperative endocervical swab also cultured Haemophilus influenzae, confirming an active infection.
- Given beta-lactam resistance, antibiotics were changed to IV ceftriaxone 2g every 12 hours and metronidazole 500mg every 12 hours.
- Following the change of antibiotics, the patient’s pain significantly improved.
- Once afebrile for 24 hours, she was transitioned to oral sulfamethoxazole-trimethoprim 800/600mg every 12 hours for a 14-day course.
- The patient was safely discharged on postoperative day five, afebrile and pain-free, with gynecology and infectious disease follow-up.
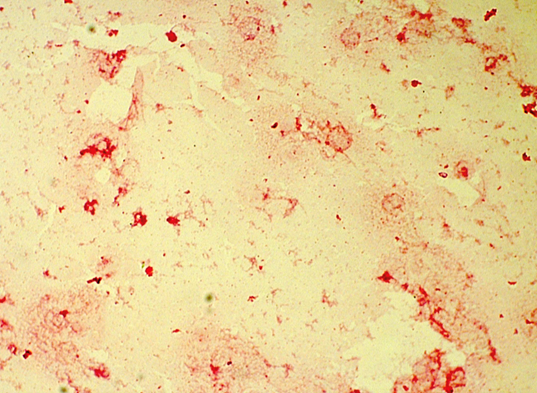
Figure 1. Haemophilus influenza in a blood culture5
Discussion
Haemophilus influenzae, though commonly associated with respiratory tract infections, is an unusual cause of genitourinary infections.1,2 While uncommon, it has been previously cultured with the female genital tract. Reported cases in obstetric patients are rare, but the bacterium has been identified in amniotic fluid, postpartum endometritis, and neonatal sepsis.1,2 The presence of Haemophilus influenzae in both blood cultures and an endocervical swab suggests a significant pathogenic role in this patient’s clinical course.
Key Learning Points:
- Atypical pathogens in obstetric sepsis: While Group B Streptococcus and Escherichia coli are more common, rare organisms like Haemophilus influenzae should be considered, especially in the setting of persistent fevers despite broad-spectrum antibiotics.3
- Early escalation and multidisciplinary input: This case emphasises the importance of involving infectious disease specialists early in cases of unresolving sepsis.
- Consideration of beta-lactam resistance: Empiric antibiotic regimens may require modification based on microbiological findings. In this case, piperacillin-tazobactam was ineffective against beta-lactamase-positive Haemophilus influenzae, necessitating a switch to ceftriaxone.
Conclusion
This case highlights an unusual but significant obstetric infection with Haemophilus influenzae following second-trimester miscarriage. Septic miscarriage is a medical emergency that requires prompt recognition and review. Prompt recognition, targeted antibiotic therapy, and multidisciplinary management were essential in ensuring a favourable outcome.
Timely treatment is critical for prevention of maternal morbidity and mortality. Given the rarity of this pathogen in obstetrics, further research may be beneficial in understanding its role in pregnancy-related infections.
Conflicts of Interest
There are no conflicts of interest for this case report.
Author’s Contributions
Fiegert, C: Drafted the work and revised it critically for important intellectual content. Agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Arnold, S: Provided final approval of the version to be published.
Acknowledgements
Thank you to the patient whose medical history is outlined in the above case report.
References
- Collins S, Ramsay M, Slack MP, Campbell H, Flynn S, Litt D, et al. Risk of invasive Haemophilus influenzae infection during pregnancy and association with adverse fetal outcomes. JAMA. 2014 Mar 19;311(11):1125-32. doi: 10.1001/jama.2014.1878.
- Nair D, Mukundan D, Chawla K, Bhat V, Kotian MS, Bhooshan S. A rare case of Haemophilus influenzae causing postpartum sepsis: case report and literature review. BMC Microbiol. 2023;23:85. doi:10.1186/s12866-023-02885-y.
- Royal College of Obstetricians and Gynaecologists. Bacterial Sepsis in Pregnancy.
- Queensland Health. Perinatal Society of Australia and New Zealand (PSANZ) Clinical Practice Guideline for Perinatal Mortality.
- PathologyOutlines.com. Haemophilus influenzae – Microbiology [Internet].
Abbreviations
CRP – C-Reactive protein
D&C – dilation and curettage
G5P2M1T1; Gravida 5 Parity 2 Miscarriage 1 Termination 1
IV – intravenous
M/C/S – microscopy, culture and sensitivity
PCA – patient-controlled analgesia
PV – per vaginam
WCC – White Cell Count





Leave a Reply