The vulva is an extraordinary, complex, yet often misunderstood part of the human body. Central to identity, pleasure, and health, the vulva remains undervalued in both cultural narratives and medical discussions. As a sexologist, I aim to elevate our understanding of the vulva and encourage open conversations about its anatomy, its role in pleasure, its changes during arousal, and the medical conditions that can affect it.
The current climate: how we talk about the vulva
The word ‘vulva’ is rarely used in everyday conversations, with many incorrectly using ‘vagina’ – which only describes the internal canal) – to describe the entire genital region. This linguistic oversight reflects broader societal discomfort in discussing genitalia, leading to misinformation and shame.
Research shows that inadequate education about vulval anatomy and function often leaves people with misconceptions about their bodies. Many vulva owners feel embarrassed or hesitant to raise questions with their healthcare providers, which can lead to delays in seeking help for medical or sexual concerns (Herbenick et al., 2010).
As healthcare providers, we play a vital role in creating a safe, inclusive environment where patients feel comfortable discussing their vulva without stigma or judgment.
Vulva anatomy: what every patient should know
A thorough understanding of vulval anatomy is essential for recognising normal variations, diagnosing conditions accurately, and facilitating discussion around sexual function. The vulva consists of the following structures:
- Mons pubis: The fatty mound of tissue located above the pubic bone. After puberty, this area is typically covered in pubic hair.
- Labia majora: The outer ‘lips’ of the vulva that protect the internal structures. These folds of skin contain sebaceous (oil) and sweat glands.
- Labia minora: The inner ‘lips’ located between the labia majora. They are typically hairless and rich in nerve endings.
- Clitoris: A highly sensitive organ with internal components, including crura and bulbs, extending along the vaginal canal (O’Connell et al., 2005).
- Vestibule: The area enclosed by the labia minora, containing the urethral opening, vaginal opening, and Bartholin’s glands.
- Bartholin’s glands: Located at the base of the labia minora, these glands secrete mucus to lubricate the vulva during arousal.
- Perineum: The area between the vaginal opening and the anus, also sensitive to touch.
The vulva and pleasure: a sensory powerhouse
The vulva is not just functional — it is designed for pleasure. The clitoris alone contains thousands of nerve endings in its glans, with the internal components extending the scope of sensation throughout the vulva. While the exact number of nerve endings varies, the clitoris is one of the most sensitive structures in the human body (O’Connell et al., 2005).
Pleasure extends beyond the clitoris; The labia, mons pubis, vestibule, and perineum all significantly contribute to sexual arousal and responsiveness. Many vulva owners achieve orgasm through external stimulation, with research showing that fewer than 20% experience orgasm through penetration alone, making our conversations about the importance of understanding and being familiar with the vulva even more important! (Herbenick et al., 2010).
If we are all able to discuss the importance of the vulva when talking with patients, we will be able to empower them to embrace their unique experiences of pleasure and to make this a fun topic in sexual relationships. Knowledge is power, and power leads to autonomy and confidence in setting boundaries and guided erotic experiences.
Let’s explore what happens to the vulva when sexual arousal is experienced? Fun facts that you can share with your patients to help them understand and appreciate their bodies!
The vulva undergoes dynamic changes during sexual arousal, reflecting its adaptability and responsiveness:
- Clitoral engorgement: Increased blood flow causes the clitoris to swell and become more sensitive
- Labial changes: The labia majora and minora swell and darken due to increased vascularisation
- Lubrication: Bartholin’s glands and the vaginal walls produce fluid, enhancing comfort during sexual activity
- Pelvic floor activation: Muscular contractions in the pelvic region can enhance arousal and orgasm
These physical responses occur alongside psychological arousal (remember the biggest sexual organ is the brain), highlighting the importance of addressing both mental and physical aspects of sexual health (Basson, 2001).
Common vulval conditions
While the vulva can be a source of immense pleasure, for many it may also be impacted by various medical conditions that can significantly impact quality of life:
- Vulvodynia: Chronic vulval pain affects 8–10% of vulva owners, presenting as burning, stinging, or irritation without an identifiable cause (Harlow et al., 2008).
- Lichen sclerosus: An autoimmune condition characterised by thinning, whitening, and itching of the vulval skin. Topical corticosteroids remain the first line of treatment (Cooper et al., 2015).
- Post-menopausal atrophy: Oestrogen depletion during menopause often leads to vulvovaginal atrophy, causing dryness, irritation, and discomfort during intercourse (Kingsberg et al., 2017).
- Dermatoses and infections: Conditions such as eczema, psoriasis, and recurrent fungal infections frequently manifest on the vulva.
Combatting stigma
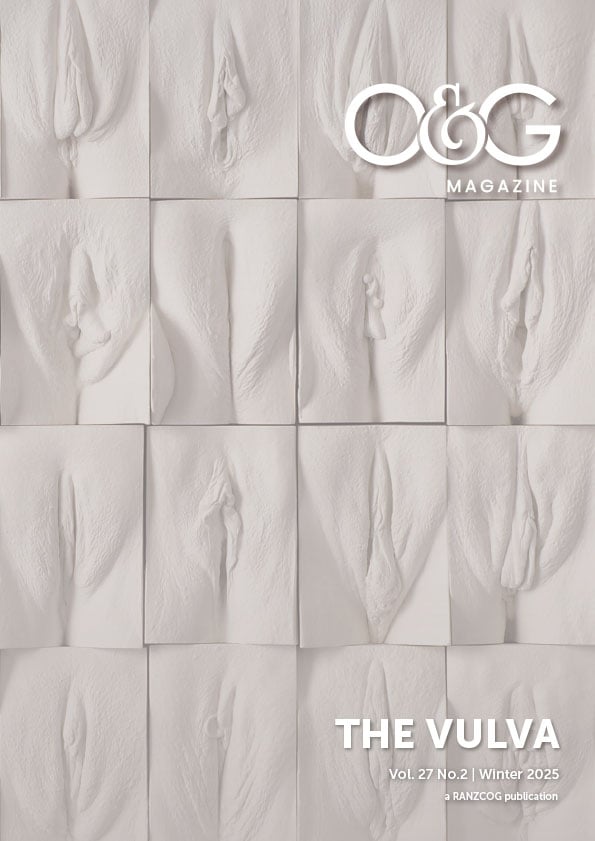
One of the most significant barriers to vulval health is the stigma surrounding its discussion. Many patients are concerned about the ‘normalcy’ of their vulva, often comparing themselves to unrealistic media representations.
Normalising the diversity of vulval anatomy is crucial. Patients should understand that variations in labial size, asymmetry, pigmentation, and texture are completely natural. Initiatives such as The Vulva Gallery, and Comfortable in My Skin website, alongside educational resources, can help foster a sense of pride and acceptance in vulva owners.
Empowering patients
As healthcare providers, you play a critical role in empowering your patients through education and confidence. Here is how:
- Educate patients: Share accurate information about vulval anatomy, function, and pleasure.
- Encourage exploration: Encourage practices such as mirror observation and self-exploration to assist patients in becoming familiar with their vulval anatomy.
- Validate pleasure: Normalise conversations about sexual pleasure as part of holistic health.
- Address concerns: Provide evidence-based treatments for conditions like vulvodynia and dryness.
Conclusion
The vulva is a remarkable part of the human body, deserving of greater attention and care. By normalising discussions around vulval health and pleasure, we can empower patients to better understand and celebrate their bodies.
With accurate education, compassionate care, and a commitment to reducing stigma, we can help vulva owners feel confident, informed, and connected to their bodies and sexual health.
References
- O’Connell, H. E., Hutson, J. M., & Anderson, C. R. (2005). The anatomy of the clitoris. Clinical Anatomy, 18(3), 183–193.
- Herbenick, D., Reece, M., Schick, V., Sanders, S. A., Dodge, B., & Fortenberry, J. D. (2010). Sexual behavior in the United States: Results from a national probability sample of men and women ages 14–94. Journal of Sexual Medicine, 7(s5), 255–265.
- Harlow, B. L., et al. (2008). Prevalence of symptoms consistent with a diagnosis of vulvodynia: Population-based estimates. American Journal of Obstetrics & Gynecology, 198(2), 191.e1–191.e6.
- Cooper, S. M., & Ali, I. (2015). Vulval lichen sclerosus: Epidemiology, aetiology and management. International Journal of STD & AIDS, 26(9), 611–619.
- Kingsberg, S. A., Wysocki, S., Magnus, L., & Krychman, M. L. (2017). Vulvar and vaginal atrophy in postmenopausal women: Findings from the REVIVE survey. Journal of Sexual Medicine, 14(3), 413–424.
- Basson, R. (2001). Female sexual response: A different model. Journal of Sex & Marital Therapy, 27(1), 51–65.





Leave a Reply