Introduction
Endometriosis is a chronic, estrogen-dependent condition, in which endometrium-like tissue grows outside the uterus, and the most common symptoms are severe painful periods, dyspareunia, infertility, pelvic pain and heavy menstrual bleeding.
It affects approximately one in seven women in Australia.1 It is associated with a substantial individual and economic burden, estimated between $7.4 and $9.7 billion annually. 2-3
Identifying endometriosis can be difficult because its symptoms often overlap with other conditions, and menstrual pain is frequently dismissed as normal by both patients and healthcare professionals. This contributes to prolonged periods of discomfort and delays in receiving appropriate care, leaving many individuals to suffer unnecessarily.
Historically, laparoscopy with histopathological confirmation was considered the gold standard for diagnosis, but the landscape has changed somewhat: advances in transvaginal ultrasound (TVUS) and international consensus on systematic imaging have repositioned ultrasound as the preferred first-line diagnostic investigation for most patients.4-5
The Evolution of Imaging Techniques in Recent Years
Until recently, diagnosis of endometriosis was often delayed by a reliance on surgery. Major guideline revisions, such as those from the European Society of Human Reproduction and Embryology (ESHRE) and the International Deep Endometriosis Analysis (IDEA) Group, as well as the Royal Australian and New Zealand College of Obstetrics and Gynaecology (RANZCOG) Australian Living Evidence Guideline: Endometriosis, now recommend imaging – primarily TVUS, as the first-line investigation for people with symptoms suggestive of endometriosis.4-6
MRI is a valuable option, especially as a second-line imaging tool when TVUS is inconclusive or unable to be performed but symptoms persist. MRI is also a valuable tool for preoperative surgical mapping as it provides excellent soft tissue contrast and three-dimensional anatomical detail with a large field of view (including extra pelvic regions) that can be extremely helpful for pre-operative planning of complex cases.
Recent updates to the European Society of Urogenital Radiology (ESUR) guidelines emphasise MRI’s role in evaluating parametrial, ureteric, and bladder involvement, which can be challenging for ultrasound.
Meta-analyses show TVUS and MRI have comparable diagnostic performance for detecting DE in key pelvic sites, especially the rectosigmoid area, though each modality has strengths for different lesion locations.
TVUS is favoured for initial, accessible screening given its lower cost, faster acquisition, ability for dynamic and real-time assessment, and relatively better clinical availability.
Overall, recent years have seen a paradigm shift towards non-invasive imaging diagnosis of endometriosis, with TVUS as the cornerstone management, supplemented by advanced MRI techniques in selected cases. This progression promotes earlier diagnosis, precise disease mapping, and improved patient-centred care while reducing reliance on invasive surgery.
Current Australian Guidelines for endometriosis diagnosis and Medicare changes
Recent advancements in Australian clinical guidelines and Medicare support will further streamline the diagnosis and management of endometriosis.
The RANZCOG Australian Living Evidence Guideline: Endometriosis, released in May 2025, recommends “Patients with symptoms suggestive of endometriosis should be offered a transvaginal pelvic ultrasound as the first-line investigation. A pelvic MRI can be offered if ultrasound is not available, or if deep endometriosis is suspected… surgery is not required as a first-line option to diagnose endometriosis.”5
Complementing these guidelines, the Australian Government has made several key changes to the Medicare Benefits Scheme (MBS) in recent times, which include:
- A new item number specific to complex gynaecological ultrasound being added to the MBS in November 2025
- A new MBS items related to extended gynaecology consultations to support the time needed for in-depths and thorough patient discussion (July 2025)
- The addition of an MBS item specific to gynaecological related MRI imaging (November 2023)
The new MBS item number for specialised ultrasounds targeting endometriosis, and this advanced imaging, will become more accessible, with a higher schedule fee reflecting the complexity and expertise required. These ultrasounds can play a crucial role in timely and accurate diagnosis, as well as treatment planning for patients with this disease.
These Medicare updates align with broader federal initiatives, including establishment and now further expansion of Endometriosis and Pelvic Pain Clinics nationwide.
Together, the evolving diagnostic guidelines and expanded Medicare provisions signal support for a comprehensive, multidisciplinary approach to improving outcomes and quality of life for Australians living with endometriosis.9
Why and How Ultrasound is Useful for Diagnosis?
TVUS is highly accurate for ovarian and deep pelvic disease, offers real-time assessment, is accessible, low-cost, and delivers results relevant both for diagnosis and for detailed surgical mapping.7 MRI is reserved for cases where TVUS is not feasible (e.g., those not comfortable with vaginal examinations), or for suspected extra-pelvic or complex disease.
| Feature | TVUS | MRI |
| Invasiveness | Minimally Invasive | Non-invasive |
| Radiation | None | None |
| Cost | Low | High |
| Accessibility | High | Moderate |
| Best for | Ovarian endometriomas, Pelvic DIE |
Complex, extra-pelvic, inconclusive USG |
| Limitations | Operator-dependent, poot detection of superficial/extrapelvic lesions |
Table 1. Comparison of TVUS with MRI.
| Structure/Parameter | rTVUS | eTVUS (comprehensive) |
| Uterus and ovaries | ✓ | ✓ |
| Organ mobility | ✗ | ✓ |
| Anterior compartment deep endometriosis nodules |
✗ | ✓ |
| Posterior compartment deep endometriosis nodules |
✗ | ✓ |
| Appointment time (min) | ˜20 | 30-45 |
Table 2.
Note: “✓” denotes routinely assessed; “✗” not assessed.
Routine vs. Endometriosis-Focused Ultrasound Protocols
Traditional “routine” pelvic ultrasound – focused on uterus and ovaries, can miss many key endometriosis features. The 2016 IDEA consensus delivered an international, stepwise protocol for detailed evaluation (“eTVUS”), which is now incorporated into both Australian and global best
practice.6-7
The IDEA Four-Step Protocol:
- Assessment of uterus and ovaries, considering features of adenomyosis and ovarian endometriomas
- Evaluation of “soft markers”: Ovarian mobility (immobility may suggest adhesions) and site-specific tenderness (SST)
- Dynamic assessment of the pouch of Douglas: Using the “sliding sign” to detect adhesions/obliteration
- Compartmental search for DIE nodules: Including USLs, posterior vaginal fornix, bladder, rectovaginal septum, and bowel
As is clear from the table above, while a routine TVUS should detect endometriosis, an extended imaging protocol must be undertaken by sonographers in order to detect deep endometriosis sonographically. Efforts are currently underway to upskill the sonography workforce across Australia and New Zealand, however, this is understandably a large task which takes time. A recent study from the University of South Australia revealed that when patients present with symptoms of endometriosis, only 1 in 5 will receive a comprehensive eTVUS due to factors such as scanning time limitations, lack of sonographer education and lack of radiologist education to report the findings.
Furthermore, this study revealed access in bulk-billing clinics and public hospitals was extremely limited with most clinics providing eTVUS being private specialist obstetric and gynaecological imaging centres. It is likely that the new MBS rebates to soon come into effect will help expand access and reduce the financial burden on patients to access eTVUS. Additionally, as more awareness, both publicly and amongst health care professionals occurs, education for imaging professionals will hopefully follow. For clinicians utilising ultrasound for their patients in the work-up of suspected endometriosis, it is important to recognise the difference between rTVUS and eTVUS, and note the limitations of both. It is especially critical to note that a normal ultrasound cannot exclude endometriosis- even a very high quality eTVUS pperformedby an expert.
How Endometriosis Presents and What Can Be Seen on Ultrasound?
Endometriosis manifests in several key forms, each with implications for imaging:
Superficial peritoneal endometriosis:
- Lesions on the peritoneal surface, often undetectable with current imaging, however new evidence is emerging related to the detection of superficial disease with ultrasound
- Ovarian endometriomas: Endometriosis cysts within the ovaries, readily identified as “chocolate cysts” on ultrasound
- Deep endometriosis Ultrasound: Endometriotic lesions that penetrate deep to the peritoneum and those typically affecting the uterosacral ligaments (USLs), pouch of Douglas (POD) rectum etc – are most visible on high-quality TVUS6
| Stage | Description |
| I (Minimal) | Few small superficial lesions, little/ no scar tissue |
| II (Mild) | More lesions, some deeper; mild adhesions possible |
| III (Moderate) | Endometriomas and more deep lesions/adhesions |
| IV (Severe) | Multiple deep implants, large endometriomas, dense adhesions |
Table 3. American Society for Reproductive Medicine (ASRM) staging.
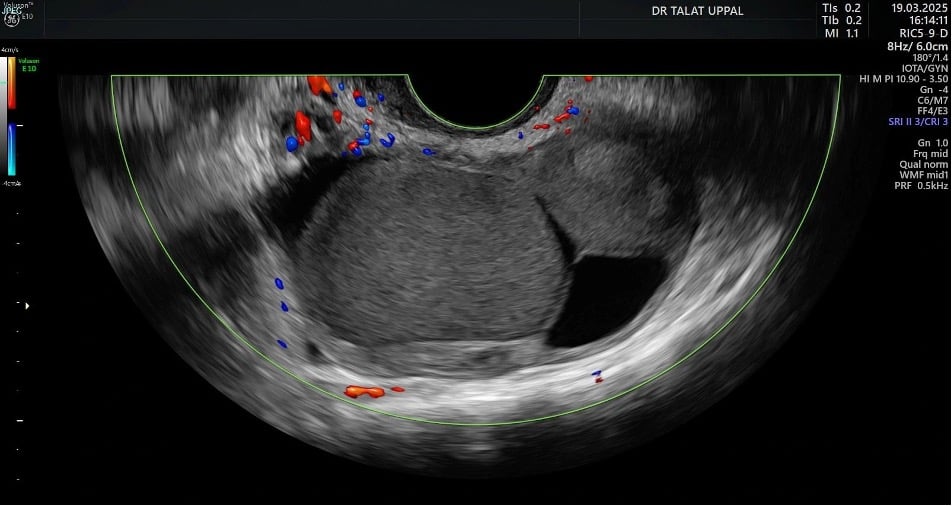
Fig 1.Endometriomas, a type of cyst formed by endometriosis in the ovary, often exhibits a “ground glass” appearance on ultrasound imaging.

Fig 2.Bowel endometriosis
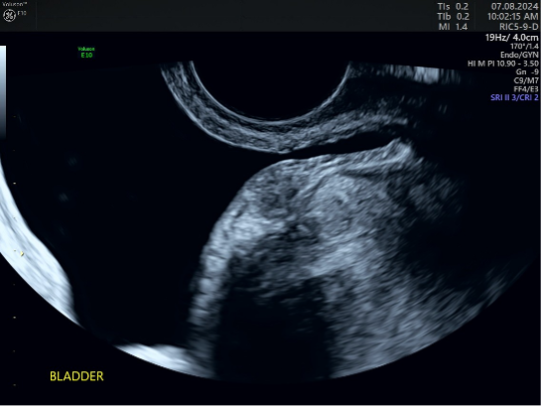
Fig 3.Bladder Endometriosis

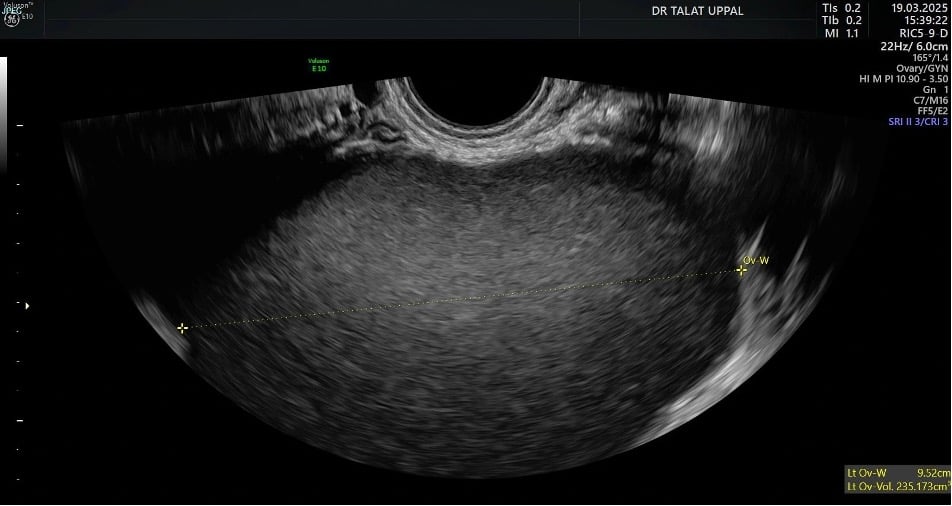
Fig 4.Endometriosis uterosacral ligament
Conclusion
Ultrasound — when used systematically and with current protocols — is now the mainstay of non-invasive diagnosis for ovarian and deep endometriosis in Australia. This, supported by government policy, updated national guidance, and continued research and education in the field hold great potential to reduce diagnostic delays and improve care for people with endometriosis. Improvements in extending ultrasound techniques, which are being integrated into first-line practice for pelvic pain and suspected endometriosis enables timely interventions, optimises surgical planning, reduces diagnostic delays, and empowers patients in their own care.
References
- Gete DG, Mishra GD, et al. Endometriosis poses substantial burden on Australia’s health system. eClinicalMedicine. 2025 Jan 16 [cited 2025 Aug 4]; [Internet]. Available from: University of Queensland News.
- Endometriosis in Australia 2023 [Internet]. Australian Institute of Health and Welfare. [cited 2025 Jun 25].
- Armour M, Sinclair J, Chalmers KJ, Smith CA, Abbott JA. The cost of illness and economic burden of endometriosis and chronic pelvic pain in Australia: a national online survey. PLoS One. 2019;14(10):e0223316.
- ESHRE Guideline Development Group. ESHRE guideline: endometriosis. Hum Reprod Open. 2022;2022(2):hoac009 [published 2022 Mar 4].
- The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG). Australian Living Evidence Guideline: Endometriosis. Melbourne: RANZCOG; 2025 [cited 2025 Aug 4].
- Keckstein J, Ulrich UA, Oppelt P, et al. International Deep Endometriosis Analysis (IDEA) group consensus: systematic sonographic assessment for deep endometriosis. Arch Gynecol Obstet. 2016;294(3):561-571. Addendum: Guerriero S, et al. 2024 Aug 25.
- Leonardi M, Condous G. How to perform an ultrasound to diagnose endometriosis. Australas J Ultrasound Med. 2018;21(2):61-69.
- Deslandes A, Leonardi M. Proposed simplified protocol for initial assessment of endometriosis with transvaginal ultrasound. Ultrasound Obstet Gynecol. 2025;65(2):142-146.
- Item 125 | Medicare Benefits Schedule [Internet]. Health.gov.au. 2025 [cited 2025 Aug 5]. Available from: https://www9.health.gov.au/mbs/fullDisplay.cfm?type=item&q=125&qt=item&criteria=







Leave a Reply