For many women living with pain attributed to endometriosis, their journey is often marked by frustration, repeated hospital visits, and a series of biomedical solutions that provide little lasting relief. While international guidelines, including the recent RANZCOG Australian Living Evidence Guideline: Endometriosis,¹ recommend a multidisciplinary team (MDT) approach, current funding models continue to prioritise biomedical interventions.
Ninah’s story exemplifies the transformative benefits that investing in MDT pain services can offer, not only for women living with persistent pelvic pain (PPP), but for the health system more broadly.
Ninah’s History
We first met in the pelvic pain clinic when Ninah was 24 years old. She shared her history of pelvic pain that had begun around age 15, and which had progressively worsened. Her medical records showed 4-5 Emergency Department (ED) admissions annually from age 20 for abdominal pain, with extensive investigations failing to identify a clear cause. Ninah often felt her severe pain was not believed by healthcare providers in the hospital. She reflected that this lack of belief was one of the most damaging aspects of her experience.
The previous year Ninah had undergone laparoscopy with excision of superficial peritoneal endometriosis and Mirena intrauterine system insertion. Sadly, this surgery not only failed to improve her pain but also saw the affected area expand, radiating into her back. This pain led to another four ED admissions in the year following her procedure. This experience is concordant with a study from the local hospital that found laparoscopic surgery did not reduce ED attendance for women living with PPP.2
Ninah’s Presentation
Ninah described her pelvic pain as a complex mix of stabbing and muscular ache, accompanied by episodes of hot and ripping sensations. Her back pain was an aching sensation, radiating into both legs. She also reported headaches, worsening with stress and tension, and abdominal bloating during pelvic pain flares. The pain had wide-reaching impacts on her life: she had taken seven months off work, experienced disrupted sleep and poor appetite. During pain flare-ups, she was confined to bed with a wheat bag. She was prescribed a range of analgesia, including oral morphine.
Understandably, Ninah described feeling “over it” and reported deep frustration that when she sought medical attention for her pain was told “it was all attributed to endometriosis”, especially when surgery had not helped and “I doubt that it would have grown back that fast”.
A Different Approach
Seeking a different approach, Ninah enrolled in our small-group, MDT-supported pelvic pain self-management program.⁴ For six weeks, Ninah joined five other women living with pelvic pain for half a day a week at the pain clinic, working with an MDT including a pain physician, pain physiotherapist, gynaecologist, pelvic health physiotherapist, psychologist, and dietician.
Together, they gained a comprehensive understanding of contemporary pain science concepts, pelvic anatomy, physiology, and pathology. The program also equipped them with pain management techniques, cognitive behavioural therapy (CBT) concepts, and practical exercises in gentle functional movements and relaxation techniques.
As is standard for all patients attending MDT pain programs, Ninah completed a battery of Patient Reported Outcome Measures (PROMs). Prior to the program she reported a mean pain intensity of 6.8/10 (severe). Her scores also indicated a low confidence in managing activity and a high degree of worry about her pain.
This constellation of low self-efficacy and high worry is a recognised risk factor for poor outcomes in women with pelvic pain, including persistent pain following surgery for endometriosis, greater menstrual pain intensity, increased pain-related disability, elevated distress, and lower quality of life. Notably, an audit of attendees to the gynaecology clinic for pelvic pain revealed that 75% had this presentation.3
Upon graduation from the program Ninah reported a clinically significant reduction in average pain intensity and in the impact of pain on her daily life. She also demonstrated increased confidence to undertake activity despite pain and a marked reduction in her worry about pain. At three, six and twelve months after completing the program she reported having essentially no pain and great confidence to manage her activity should her pain return. Ninah has not attended the ED for pelvic pain in the 6 years since completing the program. Other program participants reported similar successes, with over 80% achieving clinically significant improvement across multiple domains, and no participants reporting any clinically significant deterioration on any measure.4
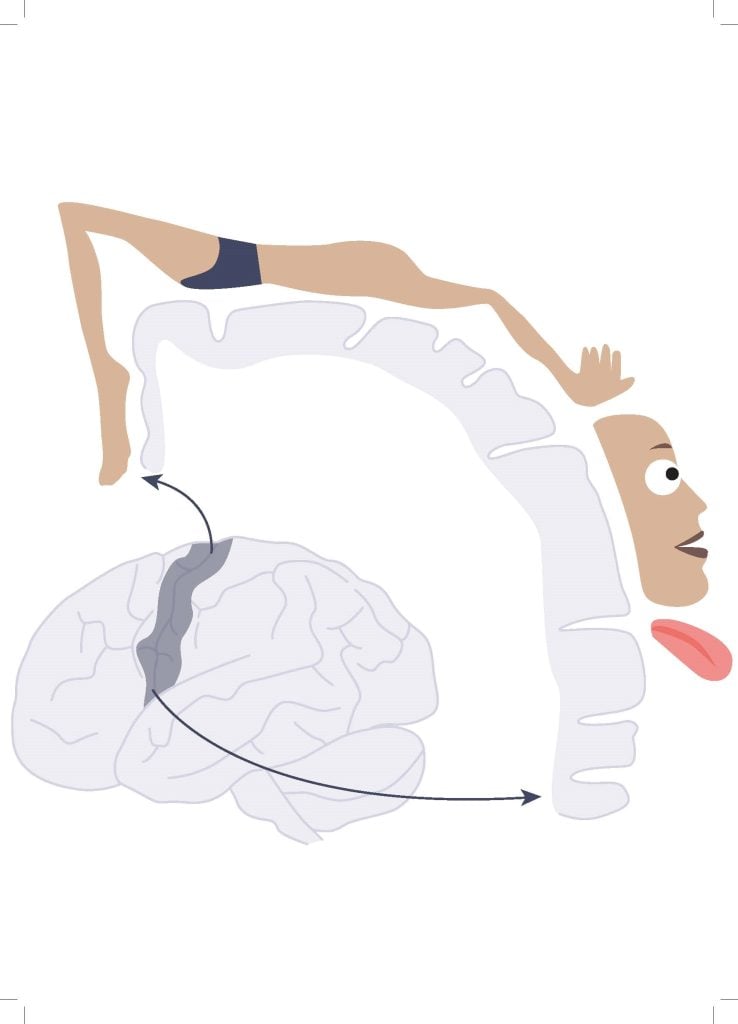
Program participants learn about the nervous system and how to untangle their pain [Picture credit: Pelvic Pain NZ]

Program participants learn about the nervous system and how to untangle their pain [Picture credit: Pelvic Pain NZ]
Ninah’s Story In Her Own Words
It is hard to describe my experience with the program without sounding like a cliché from an infomercial to be honest. In a nutshell, I went from taking incredibly strong opioids nearly every day, coming off the back of having nearly a year off work due to horrible pain, to no longer experiencing the pelvic pain I did when entering the program.
I am now 30, and I have completed postgraduate study, I am working as a teaching assistant at university, and I am still living free from persistent pelvic pain. While I do have a few days of pain, it is truly night and day to what I was experiencing.
Admittedly, I was quite dubious of pain clinics before this program. Clearly coming from a place of assumption rather than experience, I wrongly thought that this program might be superficial lip service and yet another way that the system disregards people with chronic pain. I soon realised I could not have been more wrong.
I think most people dealing with chronic pain, particularly chronic pelvic pain, feel quite rejected, disenfranchised, isolated and essentially not believed quite a lot of the time. This program alleviated all of this for me and my fellow group members. There is an MDT of specialists who you work with, focusing on all aspects of the experience of pain, and each of them really cared about us as individuals and most of all, they believed that what we were experiencing was in fact legitimate.
But what helped me most was understanding how pain actually works—how my brain and nervous system were involved. That knowledge was empowering. It gave me practical tools to “rewire” parts of myself that were misfiring and causing so much distress.
I joined the program hoping to learn how to cope with pain. And I did. But now, I don’t have to cope, because the symptoms I arrived with are gone. I’m blown away and incredibly grateful for that.
A Path Forward
Despite the transformative effects of MDT pain programs, as demonstrated by this low-cost, low-risk intervention; health system investment in New Zealand continues to focus predominantly on biomedical approaches—often yielding suboptimal outcomes, and very limited investment into MDT pain services.
We hope that sharing Ninah’s experience will help with the momentum needed to effect meaningful change for the one-in-four women living with PPP.
Conflicts
Dr Joseph is a partner in Pelvic Pain NZ which owns the PIPPI programme, and a medical advisor for the Ella Health App.
References
- Royal Australian and New Zealand College of Obstetricians and Gynaecologists. Australian Living Evidence Guideline: Endometriosis [Internet]. Melbourne (AU): Royal Australian and New Zealand College of Obstetricians and Gynaecologists; 2025 Available from: [ranzcog.edu.au/wp-content/uploads/Endometriosis-Clinical-Practice-Guideline.pdf].
- Joseph K. Emergency department attendances for persistent pelvic pain are not reduced following laparoscopic surgery for women with or without endometriosis. The New Zealand Medical Journal (Online). 2024 Mar 8;137(1591):49-54.
- Joseph K, Mills J. Unmet treatment needs in patients with chronic pelvic pain in a New Zealand gynaecology service. Australian and New Zealand Journal of Obstetrics and Gynaecology. 2019 Dec;59(6):856-60.
- Joseph K, Mills J. Improvements from a small group multidisciplinary pain self management intervention for women living with pelvic pain maintained at 12 months. Australian and New Zealand Journal of Obstetrics and Gynaecology. 2024 Oct;64(5):482-8.






Leave a Reply