‘Teaching is about igniting the mind rather than filling it up with information.’ Plutarch
Trainees are expected to be well versed in critical appraisal and good research methodology, including audit. They look to us for assistance. How can we help them, our patients and ourselves?
For some ‘academia’ sounds irrelevant and dry, but I would like to suggest quite the contrary: it can be refreshing, exciting even fun to challenge or justify what we do, and why we do it. Academia can also refer to a systematic way of learning to think and question, rather than just what to know. It is training the brain to look for new strategies to manage complex questions. Sometimes it is just recognising the obvious. I have listed academic opportunities available in every unit anywhere at the end of this article.
Reflecting on objective information, to my mind the cornerstone of academic procedure, provides a strong foundation for good clinical practice. Best practice must be a flexible dynamic process, able to change as evidence and understanding evolve. Far from receiving the wooden spoon from the Cochrane Committee, as at its inception, our specialty now leads the way in providing an evidence-based approach to clinical care.
Case study: Karyn Anderson
‘As a fourth-year medical student, my introduction to research was positive. Over the 2010–11 summer break, I undertook a research scholarship, investigating the effects of maternal smoking on the developing placenta. This gave me clinical exposure to pregnant and labouring women and database experience. This research was subsequently accepted for a poster presentation at the 2011 RANZCOG Annual Scientific Meeting (ASM) in Melbourne, alongside approximately 60 other posters from Trainees and Fellows.
For me, the conference theme: ‘Today’s science; tomorrow’s practice’ was pivotal. My research studentship changed into a passion for clinical practice of obstetrics and gynaecology and the desire to one day make this a reality.
It is hard to believe I boarded my plane to the Australian conference with feelings of trepidation. I was asking myself: was I making a mistake? Would I even understand what they were talking about? However, I need not have worried as I was greeted with the same warmth and sense of collegiality as the Trainees and Fellows attending. At the conference I learned about a range of topics and current updates and controversies. I would strongly encourage every medical student to participate in projects and submit to conferences while they are still at medical school to develop a greater appreciation of the medical specialties.’
From 2014, there will be an academic pathway to Fellowship that encompasses a PhD, using a part of advanced training time from the outset of training. Research, both clinical and purely scientific, is about looking for relevant information to inform best practice and seeking new understanding of age-old problems.
Sharing knowledge and disseminating facts and conclusions is a core responsibility of all practitioners. This goes beyond formal teaching; it encompasses the everyday ward round and handover.
Nurturing the future of O and G is also about enhancing learning experiences in the discipline, enabling the acquisition of new skills and questioning why and what we do. Moreover, it requires that we are willing to change ourselves and our practice in response to new information.

Karyn Anderson and Dr Rupert Sherwood, then President of RANZCOG, at the 2011 ASM held in Melbourne. Karyn presented her poster on the effects of maternal smoking on the placenta at the ASM. Karyn is currently completing her Trainee intern year.
Audit as a learning tool
Audit is about determining and ensuring best clinical practice and should not be viewed as a chore. Rather, it should be seen as a dynamic process enabling best care. It indicates where changes should be made and then measures the effectiveness of those changes. This can have a real impact on women’s experience of care. A recent audit of emergency department gynaecology visits showed an increase in referrals to the department after pregnancy termination following introduction of a medical termination option. It transpired that this was because GPs had not been educated about the expectations from the medical process. Without audit no one would have known there was a problem. Similarly, a vaginal birth after caesarean (VBAC) audit showed that once a VBAC choice was made, the outcomes were successful, but numbers were limited at point of entry due to inconsistent information provided within the unit. This was corrected by reaching a consensus statement within the unit and education evenings for parents. Uptake is now more appropriate.
Case study: Flora Kwon
‘At the end of fourth year I took the opportunity to do a summer research project, looking at correlation between clinical obstetrics and placental pathological findings in pregnant diabetic women. This is a current topic of increasing interest, aiming to identify biochemical markers hypoxia and prediction of pregnancy problems. I met women at the diabetic antenatal clinics and during their hospital admissions and collected their placentas. Women with a BMI of over 39 were also recruited. A database of their pregnancies and outcomes was created and compared with their placental pathology. I learned to prepare slides from the placenta, with our pathologist co-researcher. We reviewed macroscopic, microscopic and histo-biochemical changes. I gained insight into clinical risks of both diabetes and obesity during pregnancy.
‘I was able to present this project at the New Zealand ASM in Napier this year. Many clinicians approached me with interest and support for my presentation even though I was only a student.
‘My interest and passion for obstetrics and gynaecology has become much stronger. I hope to be involved with further projects in and to learn more in this field. I am very grateful for my amazing experience.’
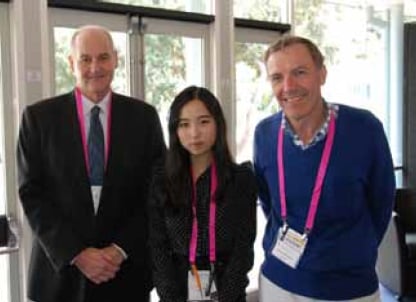
Flora Kwon, RANZCOG CEO Dr Peter White and President Prof Michael Permezel at the New Zealand ASM held in Napier, earlier this year.
Encouraging students
How as academics do we best nurture young professionals into their future career? The enthusiasm and sincerity of a role model are clearly important, as is their willingness to give time and to share their knowledge.
Studies suggest medical students are most open to making career choices in their early clinical attachments. Summer student projects provide a way of viewing the discipline in a more relaxed manner without the time pressures of a run. It is also an opportunity to really see how specialists work and behave.
Case study: Dr Kate van Harselaar Year 4 Trainee
‘My first academic research experience was a master’s degree before commencing Integrated Training Program (ITP) training.
‘The beginning and the end of any research project tend to be the most gruelling parts. Any research requires ethical approval, so this needs to be done before your research can start. Obtaining ethical approval can be challenging, but there are many benefits to it. By the time you’ve ticked all the boxes you truly understand what you’re doing and why you’re doing it. The process helps you iron out any weaknesses that might be present from risks to participants, number of participants needed to achieve an adequate power of the study, inclusion and exclusion criteria, funding and the need for Maori consultation. The final stages of writing up are also a challenge. The critical thinking acquired during this process is a great recompense for the time invested. I have just completed another ethics application as part of my elective year project.
‘Research is also an essential part of our everyday clinical practice, as all our clinical decisions should be evidence based. For those that don’t have an interest, try it, there are many hidden rewards.
The RANZCOG ITP training program offers many avenues for research. These can be projects, publications, registrar presentations for an ASM or even a PhD through the academic stream. All ITP Trainees need to undertake a research program. For many trainees this provides an opportunity to trial research for the first time.’

Dr Kate van Harselaar at College House in Melbourne.
A student’s innate empathy or aptitude for obstetrics, surgery or fetal medicine can be ignited by a case experience. The sense of being valued and respected by the speciality team, involvement in patient care and responsibility are all essential factors. Making time for students to assist or perform simple procedures is also greatly valued, especially when abundant patience and a sense of humour accompany the exercise. Teaching others is also part of the professional responsibilities of any Fellow.
There are many ways we can nurture our future specialists. Our College provides all Fellows with wide opportunities to assist our future specialty while updating our own skills at the same time.
What can you do now?
Aside from research, there are many ways of assisting with our juniors’ academic needs with regard to audit and teaching. Furthermore, Medical Councils now expect medical practitioners to participate in audit as terms for registration. Your participation in any of the following will help current Trainees and those yet to start training:
- Create or participate in a guidelines group. It is also in our own interest to reflect critically on how protocols and guidelines are followed and other quality issues.
- Assist junior staff with local surgical audits for mutual benefit.
- Submit a poster to an ASM or regional meeting.
- Complete a practice audit. Audit templates are available through the College website. C-QuIP also expects audit of outcomes in colposcopy. CPD points are available and increasingly the expectation is that all specialists are involved in some form of practice audit.
- Get involved with undergraduate teaching. This is increasingly less formal and looks to both provincial and private sectors for wider clinical experience for increasing student numbers.
- Get involved with Diploma and Certificate teaching and supervision. Increasing postgraduate year 1 and 2 interest in postgraduate training supervision translates to a greater demand for teachers with clinical experience to act as supervisors and tutors.
- Provide RANZCOG pre-training registrars with practical support with their learning and applications.
- Hospital-based clinical competencies and assessments, such as OSATS, are likely to increase – read up on them and be willing to offer training opportunities.
- Training supervisors are often in short supply. Irrespective,attend a training supervisor workshop to better understand Trainees’ needs. They are gratis!
- Apply to be a RANZCOG examiner. Examining for written and oral Membership and Diploma examinations provides all important opportunities that enhance current knowledge.
- Make yourself available for mock exams or courses for Membership exams through your regional Training Accreditation Committee.
- Encourage your unit’s participation in multicentre randomised controlled trials such as the current Magenta and APPTS. Postgraduate research is a possibility for us all.
- Undertake a Cochrane Review. Cochrane Reviews are within the capacity of any Fellow whatever their role or circumstances. They can be focused on an area of interest or relevance.
- Allow insight into real-life O and G. Even a remote Provincial Fellow or urban private practice can offer a summer studentship to a medical student to look at, say, audit of rural transfers, normal births or community outreach programs,using any clinical indicator.
- Create learning opportunities through inter-departmental meetings to present and discuss cases of mutual interest with ultrasonographers, midwives, paediatricians, emergency department staff, physicians, GPs and/or the ICU team.
- Instigate teaching topics in your region open to all health practitioners on anything from ‘ovary’ to ‘fetal abnormality’ It is surprising how much pooled learning and discussion there can be.
- Run in-house emergency drills with midwives and emergency department rural hospital transfer staff. Just practising makes for better communication.
- Become a PROMPT, ALSO or MOET instructor.
- Teach and lead critical appraisal of journal articles. Use a template such as ‘GATE’. Practice makes perfect.
- Start a fund for a Pacific island exchange experience fora student or doctor, work with the College’s Asia Pacific Committee.
- Offer your services as a volunteer through RANZCOG and take a student or Trainee with you.
- Invite a visiting expert to share current knowledge or research.Universities have lists of overseas visitors.
- Create a current research board for local awareness. Provide information and landmark articles – your own or others.
- Create an Advanced Year 5 and 6 training position in your unit that offers teaching or research opportunities.
- Offer assistance with an interesting case report or write one yourself.
- Create a local fund for research using charity sources, such as the lotto or bequests.
- Enrol in postgraduate classes in medical education, distance teaching or statistics.
- Explore the RANZCOG interactive program for teaching supervisors on CLIMATE. It is appropriate to all Fellows.
I believe that success in teaching is when one person follows a career choice because you made a difference to their learning. We are in charge of the profession’s future and there is an academic within us all. I challenge every reader to consider participating in just one additional activity from the above as your means of the nurturing the future. What are we waiting for?






Leave a Reply