Although much has been done to raise awareness of stillbirth over the last decade, it remains a major public-health problem. Healthcare providers need to understand the current rates, primary risk factors and aetiologies of stillbirth as well as how to mitigate them.
Over the past decade there have been only minor fluctuations in the rates of stillbirth in Australia and New Zealand (see Figure 1). Indeed, this plateau can be traced back to 1995, when a consensus was established between the two countries regarding the definition of stillbirth.1 The Australian Institute of Health and Welfare (AIHW) and the New Zealand Ministry of Health define perinatal death as:
‘The complete expulsion or extraction from its mother of a baby of at least 20 weeks gestation or weighing at least 400 grams at birth whether born alive or stillborn, where the births included were at least 20 weeks gestation or, if gestation was unknown, the birth weight was at least 400 grams. Stillbirths include termination of pregnancy after 20 weeks.’2
The accepted definition of stillbirth is now the absence of a heartbeat at birth. As such, the rate of stillbirths per 1000 in 2009 was 7.6 and 7.5 for Australia and New Zealand, respectively.3,4 However, according to the World Health Organisation (WHO), which defines stillbirth as: ‘a baby born with no signs of life at or after 28 weeks’ gestation’, the rates of stillbirth per 1000 are 2.9 and 3.5 for Australia and New Zealand, respectively.5 This variation in definition is important in understanding the static nature of the stillbirth rates in both countries. Advancements in science and technology have improved outcomes for numerous risk factors and disorders, but also allowed for greater identification of abnormalities that may affect termination rates, which after 20 weeks will count as stillbirths. As such, it is important healthcare providers understand current rates, primary risk factors and aetiologies of stillbirth in Australia in conjunction with how to mitigate them.
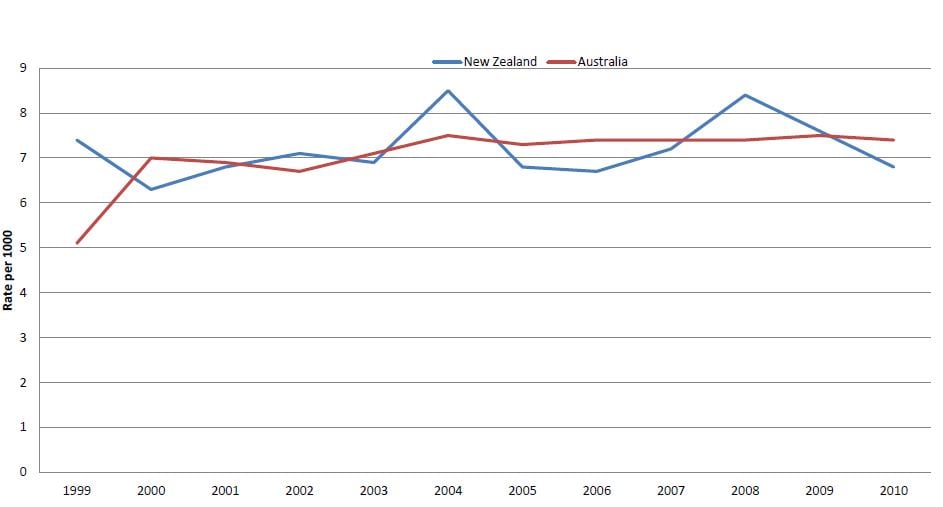
Figure 1. Stillbirth rate per 1000 from 1999–2010 in Australia and New Zealand.
Source: Australia’s Mothers and Babies 1999–2010, AIHW; Fetal death rates 1999-2010, Statistics New Zealand.
Risk factors for stillbirth
According to the Australian Mothers and Babies Report 2010, there were 2206 stillbirths in Australia, with rates ranging from 5.8 per 1000 births in New South Wales (NSW) to 11.3 per 1000 births in the Australian Capital Territory (which includes many high-risk pregnancies and terminations from residents of surrounding NSW, which therefore inflates the rate).2 Analysis of these data indicates the major non-modifiable risk factors for stillbirth in Australia include maternal age, early gestation, plurality, pregnancies conceived with assisted reproductive therapy (ART), primigravid women, grand multiparous women and women identifying as Aboriginal or Torres Strait Islander. Pre-existing hypertension and diabetes also feature prominently and, in addition, there are some lifestyle related risk factors, of which maternal overweight/obesity and smoking are considered the most important.6
Women under the age of 20 had the highest age-related stillbirth rate of 14.4 per 1000, followed by women over the age of 40, with a rate of 10.4 per 1000. Rates were also higher for babies of first-time mothers (6.6 per 1000 births) than those whose mothers had at least one previous birth (6.3 per 1000 births). However, for grand multiparous women (women who have had four or more previous births), the rate was much higher at 10.9 per 1000 births. The fetal death rate of twins (18.9 per 1000 births) and higher-order multiples (40.0 per 1000 births) was significantly higher than that of singleton babies (7.0 per 1000 births). The fetal death rate was 12.2 per 1000 births for women giving birth after ART treatment. Most stillbirths were preterm (82.0 per cent of the total). Women identifying as Aboriginal or Torres Strait Islander had a higher rate at 11.1 per 1000 compared to 7.1 for non-Indigenous women.2 Meta-analysis indicates maternal overweight and obesity increases the odds of stillbirth by 23 per cent and 60 per cent, respectively. Any smoking during pregnancy increases the risk by 36 per cent. Indeed, the population-attributable risk (PAR) for overweight and obesity, smoking and maternal age is about 30 per cent of all stillbirths.6 The increased risk of stillbirth for women with pre-existing diabetes is three times and for pre-existing hypertension the risk is increased 2.6 times.6
The aetiology of stillbirth
The Perinatal Society of Australia and New Zealand (PSANZ) created a classification system to ensure homogenous reporting of fetal death (see Box 1).7
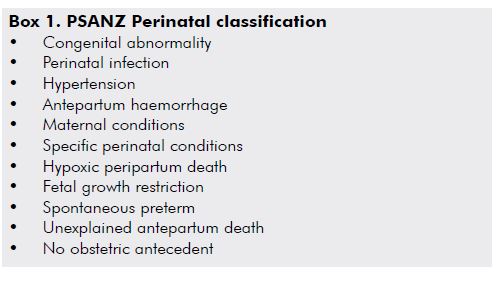
Following this classification system, the most common causes of stillbirth in Australia are: congenital abnormalities (25.8 per cent); unexplained antepartum death (22.5 per cent); spontaneous preterm (15.3 per cent); specific perinatal conditions (nine per cent); fetal growth restriction (8.8 per cent); antepartum haemorrhage (4.4 per cent); hypertension (3.2 per cent); perinatal infection (3.1 per cent); maternal conditions (three per cent); hypoxic peripartum death (1.3 per cent); and no obstetric antecedent (one per cent).2 The pathophysiology of some of the above aetiologies is complex. While congenital abnormalities are the leading cause of stillbirths, the specific syndromes and chromosomal abnormalities responsible vary widely. They are generally grouped into systems (such as the cardiovascular), chromosomal and metabolic abnormalities. There are over 90 disorders within these categories – some incompatible with life, but others causing major handicap – and no single diagnosis accounting for more than two per cent of all occurrences. The more common of these are jugulolymphatic obstruction, trisomy 21, Turner syndrome and anencephaly. Spontaneous preterm birth is another leading cause, defined as commencement of labour or membrane rupture <37 weeks. At times the labour may occur too early for the birth to be compatible with extra-uterine life and sometimes there is associated heavy bleeding leading to fetal death, while extended periods of membrane rupture increase the risk of chorioamnionitis.8
Investigations
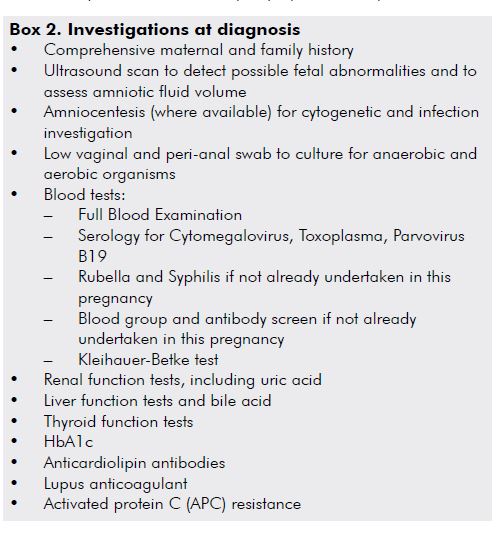
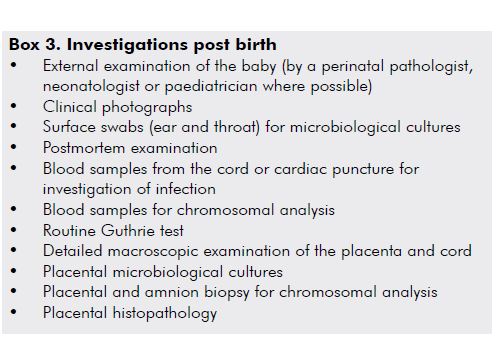
Once fetal death has been confirmed and plans have been made for the birth, PSANZ recommends a number of core steps to determine the cause. These investigations are divided into those undertaken at diagnosis (see Box 2) and those undertaken following birth (see Box 3).7 Each investigation has some merit in the diagnosis of cause of stillbirth, but the yield of each test will vary based on the clinical details. For example, external visualisation of the child after birth can demonstrate external abnormalities, some of which may have been missed by chromosomal analysis. Similarly, a karyotype may reveal trisomy 21 in a baby who has not been sent for autopsy. These investigations are important to establish the cause of stillbirth to provide answers and ensure appropriate management of future pregnancies. At present, the stillbirth autopsy rate across the country is only about 40–50 per cent, and a higher rate may reduce the numbers of stillbirths which are classified as unexplained.
Managing the next pregnancy
One of the many important uses of a clear diagnosis of the cause of stillbirth is the guidance it may give about the next pregnancy, especially if there is some chance of recurrence such as with inherited congenital anomalies. On the other hand, it is known that after unexplained stillbirth there is at best a modest increased risk of stillbirth in the next pregnancy of about 1.5 to two times, although some authors report no increased risk.9 Even taking the worst estimates, this may mean the absolute risk of a recurrence is extremely low. The management of the next pregnancy is always a compromise between what is medically indicated (in terms of the recurrence risk) and dealing with the inevitable anxiety couples will experience up to the point a healthy baby is born. A survey of Fellows from a few years ago produced some interesting results when they were faced with the conundrum of managing the next pregnancy after an unexplained term stillbirth.10 Almost all would initiate increased levels of fetal surveillance, most would consider early induction of labour, with the most common time for this around 38 weeks, and some would opt for elective caesarean section. Whatever the birth plan for an individual woman, it is a good practice point to discuss the pregnancy and birth plan early on (even pre-pregnancy in some cases to allow for interventions to reduce any modifiable risk factors) and stick to an agreed approach. Uncertainty fuels anxiety and this can make the next pregnancy extremely challenging for all concerned.
Summary
Stillbirth remains a major public health problem, with 2206 stillbirths reported in Australia in 2010. The first-ever comprehensive report on stillbirth will be released by AIHW in the next few months. In 2011, the Lancet released a series of articles on stillbirth that grabbed much media attention.11 Despite an increased focus, there is little sign the rate is reducing and indeed some of the risk factors for stillbirth are increasing in our population. At present there is also much attention on the importance of fetal movement monitoring and maternal sleeping position as two possible areas of intervention to reduce the risk of late term stillbirth. Hopefully, the next decade will see some significant inroads into better management of this tragic adverse outcome of pregnancy and some significant reductions in the rate.
References
- Births, Deaths, Marriages, and Relationships Registration Act 1995, New Zealand; Department of Internal Affairs (1995).
- Zeki Z, Hilder L, Sullivan E. Australia’s Mothers and Babies 2010 Perinatal statistics series no. 27 Cat. no. PER 57. Canberra: AIHW National Perinatal Epidemiology and Statistics Uni; 2012.
- Zeki Z, Hilder L, Sullivan E Australia’s Mothers and Babies 2009 Perinatal statistics series no. 25 Cat. no. PER 52. Sydney: AIHW National Perinatal Epidemiology and Statistics Uni; 2011.
- Fetal and infant deaths 2008 and 2009. Wellington: Ministry of Health; 2012.
- Stillbirth. Geneva: World Health Organisation; 2013; Available from: www.who.int/reproductivehealth/topics/maternal_perinatal/stillbirth/en .
- Flenady V, Koopmans L, Middleton P, Froen JF, Smith GC, Gibbons K, et al. Major risk factors for stillbirth in high-income countries: a systematic review and meta-analysis. Lancet 2011; 377 (9774):1331-40.
- Perinatal Society of Australia and New Zealand Perinatal Mortality Audit Guideline; Second Edition, Version 2.2. Section 7: Perinatal Mortality Classifications; 2009.
- Reddy UM, Goldenberg R, Silver R, et al. Stillbirth classification – developing an international consensus for research: executive summary of a National Institute of Child Health and Human Development workshop. Obstet Gynecol. 2009; 114: 901–914.
- Robson S, Thompson J & Ellwood D. Obstetric management of the next pregnancy after an unexplained stillbirth: an anonymous postal survey of Australian obstetricians ANZJOG 2006 46, 278-282.
- Robson SJ, Chan A, Keane RJ, Luke CG Subsequent birth outcomes after an unexplained stillbirth: preliminary population-based retrospective study ANZJOG 2001, 41: 29-35.
- Lancet Stillbirths April 2011.







Leave a Reply