The changing landscape of obstetric care in Australia and elsewhere in the world has brought new challenges to our practice. As well as the changing demographics of women who become pregnant, the steady rise in the rate of caesarean sections means we will encounter more complex forms of placentation, including placenta praevia and placenta accreta.
In normal placentation, the trophoblast does not invade deeper than the deciduas. Invasion of part or all of the placenta, through the deciduas into the myometrium and beyond, is termed morbidly adherent placentation and is divided into three subtypes: placenta accreta is trophoblast invasion into the superficial layer of the myometrium; placenta increta is extension of trophoblast invasion deep into the uterine myometrium1; and placenta percreta is trophoblastic invasion through the entire myometrium to, and sometimes beyond, the uterine serosa.1
The risk of placenta accreta increases significantly with consecutive caesarean sections.2 The complications of placenta accreta are significant and include a risk of maternal death due to severe haemorrhage, as well as damage to the uterus, bladder and bowel. These complications can be managed with prior knowledge of the underlying condition, allowing for appropriate resource allocation at the time of surgery. This may include provision of blood products, interventional radiology, appropriate surgical and anaesthetic cover, as well as intensive care facilities.2
Our ability to diagnose placenta accreta has changed over the last decade and, like most things in medicine, a high index of suspicion and experience has increased our chance to make a correct diagnosis. ultrasound, MRI or a combination of these modalities are nowadays utilised depending on the availability of expertise and equipment. This article will explore the features of placenta accreta on ultrasound and MRI. Patients at risk of placenta accreta include those with a history of previous operative delivery; previous gynaecological procedures that disrupt the integrity of the uterus (such as curettage and myomectomy); and retained placenta. Advanced maternal age is also an independent risk factor.3
It is important for both the sonographer and sonologist to ask a patient about previous uterine surgery and also document relevant history in the report. The classical features of placenta accreta/increta/percreta at the morphology ultrasound are summarised in Table 1.4,5,6
Table 1. Features of placenta accreta/increta/percreta at ultrasound
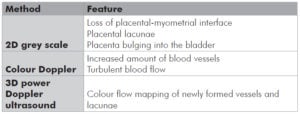
A number of studies looking at all these factors have been published, some with conflicting evidence. Interestingly, a recent study suggests that if multiple features of placenta accreta are present, the risk of a false positive is far less likely. We should therefore include assessment and documentation of all the features mentioned in Table 1.7
With improved equipment and insight, this diagnosis may also be possible in early first trimester (as early as seven weeks). A retrospective study considered early features of placenta accreta to be a low-lying gestational sac and myometrial thinning of the uterine scar area.8 In two of the six reported cases, there was early fetal demise. Subsequent curettage lead to very heavy bleeding requiring a hysterectomy in both cases. It is also important to remember that a morbidly adherent placenta can also occur without any risk factors. We should take care to look at every placenta at morphology study to allow for appropriate referral to a tertiary care centre in case of suspicious findings.
Figure 1a. 2D and colour Doppler imaging showing loss of placental-myometrial interface, lacunae and increased blood vessels. Placenta bulging into the bladder.
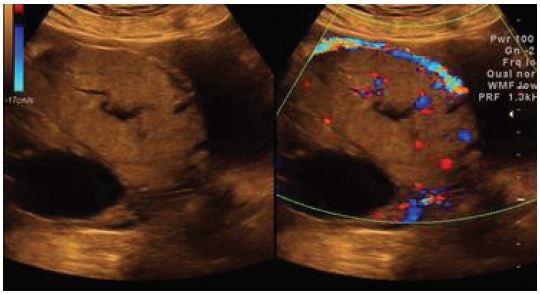
Figure 1b. 3D power Doppler: Newly formed blood vessels and lacunae.
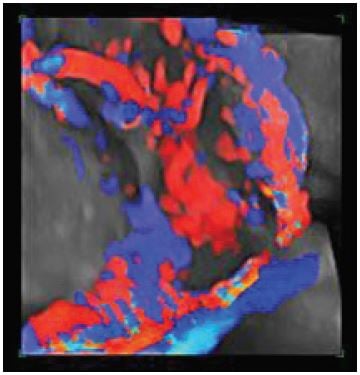
Figure 2a (left) and 2b (right). 2a: Sagital True FISP image showing placenta accreta at bladder/placental interface (arrow). 2b: Coronal blade image showing placenta accreta at bladder placental interface.
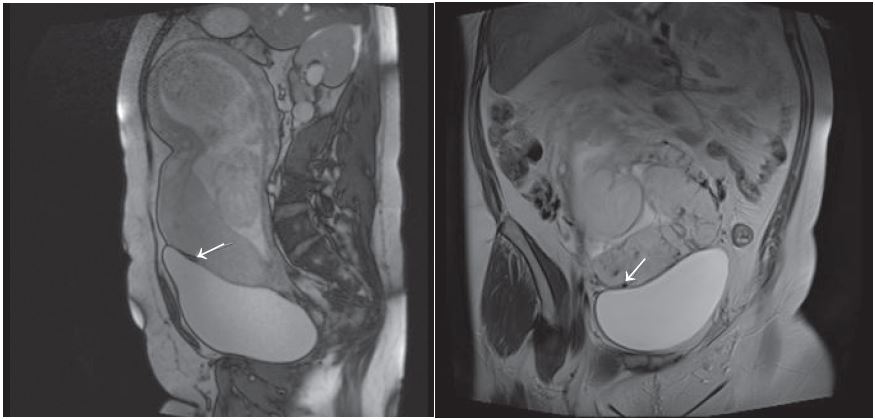
Placental MRI is now frequently utilised in diagnosing placenta accreta. It complements ultrasound and Doppler evaluation in cases suspected of placenta accreta. With improvement in Fast T2 imaging, sensitivity and specificity of MRI now reaches that of ultrasound with Doppler.9 In our institution, we acquire True Fast T2 images (True FISP and Blade sequences) in three planes through the placenta (Avanto, Seimens, Germany). A loss of placental-myometrium interface with signal alteration (see Figures 2a and 2b) suggests abnormal placental adhesion. A wide field of view is an added advantage of MRI over ultrasound. It provides a complete view of placenta with relationship to adjoining structures.
The presence of fetal and placental cells in maternal circulation in placenta accreta is a novel approach under research. A study by Muira and colleagues has suggested that higher levels of placental mRNA are present in the maternal circulation in the subgroup of patients at risk of placenta percreta.10 It might assist us in future to decide on the most appropriate procedure for the individual patient.
References
- Ozcan T, Presman EK. Imaging of the placenta. ultrasound Clin. 3 2008; 13-22.
- Welsh A, Ellwood D, Carter J, Peduto A, Vedelago J, Bennett M. Opinion: Integration of diagnostic and management perspectives for placenta accreta. ANZJOG 2009; 49 (6) 578-87.
- Miller DA, Chollet JA, Goodwin TM. Clinical risk factors for placenta previa-placenta acreta. Am J Obstet Gynecol. 1997;177:210-214.
- Chomstock CH. Antenatal diagnosis of placenta accreta: a review. ultrasound Onstet Gynecol. 2005; 26:89-96.
- Yang JI, Lim YK, kim HS, Chang KH, Lee JP, Ryu HS. Sonographic findings of placental lacunae and the prediction of adherent placenta in women with placenta totalis and prior caesarean section. ultrasound Obstet Gynecol. 2006; 28: 178-182.
- Wong HS, Cheung YK, Strand l, Carryer p, Parker s, Tait J, Pringle KC. Specific Specific sonographic features of placenta accreta:tissue interface disruption on gray-scale imaging and evidence of vessel crossing interface-disruption sites on Doppler imaging. ultrasound Onstet Gynecol. 2007; 29:239-241.
- Shih JC, Palacios Jaraguemada JM, Su YN, Shyu MK, Lin CH, Lin SY, Lee CN. The role of three-dimensional power Doppler in the antenatal diagnosis of placenta accreta: comparison with gray-scale and colour Doppler techniques. ultrasound Obstet Gynecol. 2009; Feb:33(2):
193- 203. - Comstock CH. Antenatal diagnosis of placenta accreta: a review. Ultrasound Obstet Gynecol. 2005; 89-96.
- Masselli, et al. MR Imaging in the evaluation of placental adhesive disorders: correlation with color Doppler ultrasound. Eur Radiol. 2008; 18: 1292-1299.
- Miura S, Yamasaki K, Yoshida A, Yoshiura k, Nakayama D, Niikawa N, Mazuzaki H. Increased level of cell-free placenta mRNA in a subgroup of placenta previa that needs hysterectomy. Prenat Diagnosis. 2008; Sep 28(9):805-9.






Leave a Reply