Until the mid-20th century, obstetricians in developed countries were preoccupied with the prevention of maternal death. As maternal mortality rates declined in the second half of the 20th century, attention turned to the welfare of the unborn and newborn child.
In the early 1940s, Dugald Baird reported that the perinatal mortality rate for nulliparous women delivering after 42 weeks gestation in Aberdeen, Scotland, was a staggering one in eight, due to a combination of antenatal and intrapartum asphyxia, meconium aspiration and birth trauma. He was among the first obstetricians to advocate induction of labour for prolonged pregnancy and more liberal use of caesarean section. These views were supported by the British birth survey in 1958, which showed a two-fold increase in stillbirth for pregnancies delivering at 42 weeks, compared to 40 weeks gestation.1 From the 1960s onwards, it became common practice to induce labour before 42 weeks gestation. Randomised controlled trials showed a policy of induction at 41 to 42 weeks gestation was associated with reduced perinatal morbidity and mortality without a significantly increased rate of caesarean section.2
Current practice
In most developed countries, prolonged pregnancy is now managed by planned delivery. The most recent evidence-based guideline on induction of labour from the uK National Institute for Health and Clinical Excellence (NICE) recommends offering induction any time from 41 weeks, provided resources allow.3 Prior to formal induction, membrane sweeping is commonly practised, as this reduces the need for ‘post-dates’ induction.4 Most women with a previous caesarean section have repeat caesarean delivery if the pregnancy becomes prolonged, as induction is associated with an increased risk of uterine rupture.
There is considerable variation in practice. Women with induced labour are likely to need more support, analgesia and monitoring than women in spontaneous labour, so most units limit the number of inductions. Local custom and resources largely dictate the gestation at which ‘routine’ delivery is offered.
Gestational age is calculated inconsistently. Estimated date of delivery (EDD) is most reliably predicted by ultrasound measurement of crown-rump length (CRL) at eight to 12 weeks or biometry at 14 to 20 weeks.5 However, clinicians often use an EDD based on the last menstrual period (LMP) or CRL measured before eight weeks or after 12 weeks, both of which are less reliable.
Women who do not have a scan until late in pregnancy pose a particular problem. Estimating gestational age is unreliable and women may be offered induction on the basis of an uncertain EDD, or serial monitoring while awaiting spontaneous labour. It is not known which of these strategies is more effective.
Problems with current practice
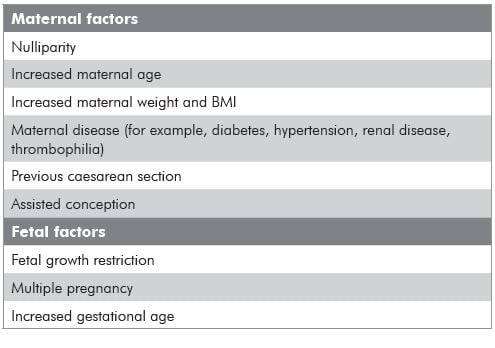
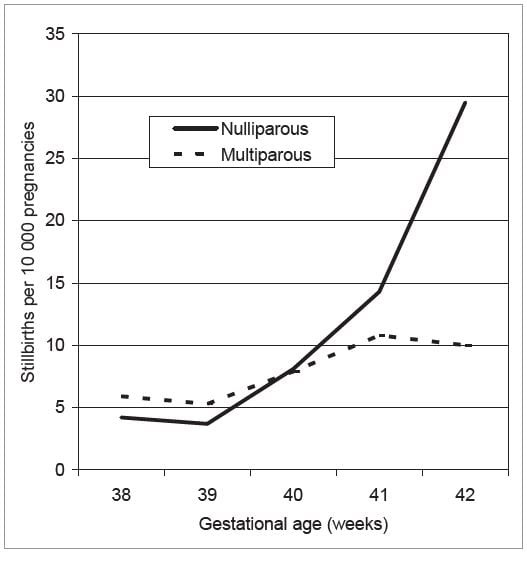
In most cases, the purpose of labour induction is to reduce the risk of stillbirth. unfortunately, a policy of routine ‘post-dates induction’ has little impact on the overall term stillbirth rate, as most stillbirths happen before 41 weeks gestation and the pregnancies at greatest risk are often not identified. Many factors, other than gestational age, are associated with an increased risk of stillbirth (see Table 1). Women with these risk factors may be offered earlier induction, but this is not applied in a systematic or consistent way. Conversely, some women have a very low risk of stillbirth despite prolonged pregnancy and may benefit little from induction. For example, while the stillbirth rate for nulliparous women increases exponentially between 39 and 42 weeks, the increase in the rate for multiparous women is much less marked (see Figure 1).6,7
Table 1. Risk factors associated with unexpected term stillbirth
It is also unclear what the stillbirth rate would be in prolonged pregnancy with modern maternity care. Most of the randomised trials of induction for prolonged pregnancy were conducted 20 to 40 years ago. Some women undoubtedly benefit from induction at 41 to 42 weeks (or earlier), while others are at very low risk of stillbirth and may be worse off with induction. The question is: can we identify who benefits most from delivery?
The current situation with regard to fetal risk assessment at term resembles Down’s syndrome (DS) screening as it was 30 years ago. Invasive testing was offered on the basis of maternal age and most DS pregnancies went undetected. With the introduction of serum screening and ultrasound assessment, it is now possible to detect a much higher proportion of DS pregnancies without increasing invasive testing rates. Our future goal should be to reduce unexpected term stillbirths by a policy of risk assessment and selective delivery, while minimising the harm caused by unnecessary interventions.
The future
We need to devise customised assessment tools so that we can estimate the stillbirth risk for individual pregnancies. Factors assessed would include maternal age, parity, ethnic group, past history, co-morbidity and estimated fetal size. Women would be offered delivery at a gestation where the estimated stillbirth risk exceeds an agreed threshold. As a result, an overweight nulliparous woman might be delivered at 39 to 40 weeks gestation; an uncomplicated multiparous woman might be advised against induction at any gestation. This strategy would have the potential to reduce term stillbirths without an increase in interventions.
There will be many challenges to developing a risk assessment strategy to reduce perinatal morbidity and mortality. Factors such as age, parity and co-morbidity are not independent variables and risk ratios cannot simply be multiplied, as is done for DS screening. We also need to debate the level of risk that would justify delivery and the level of maternal morbidity that would be acceptable in order to reduce stillbirths – particularly as induction before 41 weeks is likely to be associated with an increased caesarean section risk. What is appropriate for one community may not be appropriate for others.
Conclusion
Prolonged pregnancy is a common indication for planned delivery. However, in the future we need to develop more effective strategies to reduce perinatal morbidity at term by selective delivery based on overall risk, not on gestational age alone.
Figure 1. Stillbirth rate by week of gestation. North-East London 1989-92.6
References
- Butler NR, Bonham DG. Perinatal Mortality: The First Report of the 1958 British Perinatal Mortality Survey. E&S Livingstone Ltd, London 1963.
- Gülmezoglu AM, Crowther CA, Middleton P. Induction of labour for improving birth outcomes for women at or beyond term. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No.: CD004945. DOI:10.1002/14651858.CD004945.pub2.
- National Institute for Health and Clinical Excellence (uK). CG 70 –Induction of Labour: Clinical Guideline. July 2008.
- Boulvain M, Stan CM, Irion O. Membrane sweeping for induction of labour. Cochrane Database of Systematic Reviews 2005, Issue 1. Art. No.: CD000451. DOI: 10.1002/14651858.CD000451.pub2.
- Bottomley C, Bourne T. Dating and growth in the first trimester. Best Practice & Research Clinical Obstetrics & Gynaecology 2009; 23: 439- 52.
- Hilder L, Sairam S, Thilaganathan B. Influence of parity on fetal mortality in prolonged pregnancy. European Journal of Obstetrics & Gynaecology and Reproductive Biology 2007; 132: 167-70.
- Ingemarsson I, Kallen K. Stillbirths and rate of neonatal deaths in 76 761 post-term pregnancies in Sweden 1982-1991: a register study. Acta Obst Gynaecol Scand. 1997; 76: 658-62.






Leave a Reply