In 2006, the Fertility Society of Australia commissioned a large survey of how fertility problems affect Australians. Some of the findings are quite surprising in terms of how little general knowledge is held in the community about fertility.1 As general practitioners, we are ideally placed to highlight these fertility issues for our patients.
Infertility is defined as failure to conceive after 12 months of regular unprotected intercourse. The majority of couples matching this definition will have subfertility, with true sterility estimated at only one per cent. It is helpful to bear in mind that 50 to 60 per cent of ‘infertile’ couples will conceive in the second year of trying, if no reason for subfertility is found. It is important to counsel these couples to be hopeful of eventual success if age is on their side.2 However, once three years of trying to conceive have passed, the chances of success are much less and intervention is recommended (if wanted and not already pursued).
Extent of the issue
Fertility problems affect one in six Australian couples and this has been constant over the past several decades.1 What has changed, however, is the time at which couples start to try for pregnancy, now much later, when age-related fertility decline is starting to have an impact. Consequently, couples don’t have as long in their reproductive lives to either continue trying for spontaneous conception, or give themselves the best chance with assisted reproductive technologies (ART).
It is a problem for the couple together, with an estimated 30 per cent female factors, 30 per cent male factors, 30 per cent combined factors and ten per cent unexplained.
Over the last five years, the number of ART procedures has increased on average by over ten per cent per year in Australia and New Zealand. Latest estimates indicate that 3.1 per cent of babies born in Australia are conceived as a result of ART treatment.7
Lifestyle factors that influence fertility
A lot of emphasis is put on medical causes and interventions for fertility. In fact, lifestyle factors play a significant role and are perhaps underestimated in general practice and certainly in mainstream media.
Age
Female fertility starts to drop off after the age of 31 and the rate of decline increases as a woman approaches her 40s. The percentage of infertility is estimated at:
- Eight per cent for women aged 19 to 26 years;
- 13 to 14 per cent for women aged 27 to 34 years; and
- 18 per cent for women aged 35 to 39 years, therefore, twice the rate from age 25 to late 30s.2
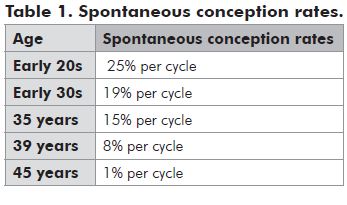
Another way of looking at it is by spontaneous conception rates (see Table 1).
The message is not getting through
Despite stating they knew fertility declines with age, a surprising 42 per cent of Australian women aged 40 to 49 years thought they could have a child without any problems.1 Pregnancy for an older woman also presents a higher risk for an array of complications, the discussion of which is beyond the scope of this article.
So what about men? Not one person, either male or female, in a Fertility Society of Australia (FSA) survey realised that a man’s age might be a reason for needing IVF treatment.
Although not as dramatic, it is now clear male age does affect conception rates. Specific sperm parameters have been shown to change with age, in particular, motility rates deteriorate, and observed conception rates fall from the late 30s onwards.2,3 If a woman is 35 years of age, the risk of infertility increases from 18 per cent if the male partner is 35 years old to 28 per cent if he is 40 years old.2
It is also documented that with advancing paternal age there is a small increased risk of autism, schizophrenia and some types of malformations in offspring. Up to seven per cent of Down’s syndrome cases can originate from the paternal side.5,6
As GPs, we should take every opportunity to bring up the issues around delayed parenting with our patients.
Smoking
39 per cent of women and 36 per cent of men experiencing fertility problems smoke.1 The smoking community know it is unhealthy, but perhaps don’t understand the possible implications for fertility. Smoking and reproductive life is a detailed report published by the British Medical Association which documents all the usual information, with concise and highlighted boxed summaries.6 I find picking some of these boxes out from the pdf copy can be a useful visual tool when talking to couples. For example:
- Men who smoke have a lower sperm count and a higher proportion of malformed sperm.
- Women who smoke take longer to conceive.
- Women who smoke are twice as likely to be infertile as non-smokers.
- Men and women who smoke have a poorer response to fertility treatment.
- Women who have stopped smoking take no longer to become pregnant than women who have never smoked.
- Stopping smoking improves sperm count and quality.
There is also evidence that if a man has been smoking for five years or more prior to conception, his child is four times more likely to develop childhood cancer before the age of five years.
There is a careful line to tread, I find, when giving negative information without being punitive or judgemental, especially if the male partner is not a regular attendee and has been dragged along by his partner, already feeling inadequate about not achieving pregnancy. If one partner is a smoker but the other is not, I try to see them separately for smoking cessation counselling.
Alcohol
30 per cent of men and 19 per cent of women affected by fertility problems report they drink more than 14 alcoholic drinks per week and that is probably underreported.1 Even moderate alcohol intake is related to delayed conception. The evidence quantifying the effects (therefore, how much is safe, if any) is not entirely conclusive and is difficult to control for confounding factors.14 The National Health and Medical Research Council (NHMRC) recommendation for women who are pregnant or planning a pregnancy is that abstinence from alcohol is the safest option to reduce the risk of harm to the developing fetus.
Weight
Fertility for women declines with increasing weight, miscarriages are more likely, and pregnancy and perinatal complications are higher. In one large study, after adjusting for other lifestyle variables, age and menstrual pattern, women with a body mass index (BMI) of more than 25 (or less than 20) were at twice the risk of infertility compared to women with a normal BMI.4 Male BMI of less than 20 or more than 25 has also been associated with a reduction in sperm quality.4
There is good evidence that modest weight reduction and increased exercise can improve fertility, especially in very obese women. Some fertility clinics now offer lifestyle programs in conjunction with, or prior to, treatments to improve outcomes.
Further history and investigations
Causes of subfertility
- Tubal factors with incomplete blockage (for example, pelvic inflammatory disease, endometriosis, adhesions).
- Endometriosis.
- Ovulation factors – irregular or infrequent (for example, PCOS).
- Uterine abnormalities – fibroids, septum.
- Lifestyle factors.
- Abnormal sperm.
Causes of complete infertility
- Complete tubal occlusion.
- Azoospermia.
- Absence of ovulation and menstrual cycle:
- Temporary (for example, amenorrhoea, hyperprolactinaemia, hypothalamic suppression from stress).
- Permanent (for example, congenital malformation, genetic abnormality).
The female partner
- Ensure adequate folate (400 mcg daily) supplements, adequate iodine intake/supplements (150 mcg daily), vitamin D intake (sun and supplements 10 mcg daily). Most prenatal vitamin mixes will cover this, but it is helpful to check.
- A Pap smear and pelvic examination.
- Hormone levels on day 2 and day 21 of the cycle.
- Gynaecological ultrasound.
- HyCoSy/hysterosalpingogram.
With a history of painful periods, especially beyond the first day or two, spotting premenstrually, pain with sex, or pelvic pain between periods, endometriosis should be considered.
If endometriosis is detected by scans showing endometriomas, or with a high index of suspicion, then laparoscopy with a surgeon experienced in excision of all visible spots of endometriosis is the best treatment option for subsequent fertility outcomes and early referral is recommended. Laparoscopy is also indicated in asymptomatic women with failure to conceive, as endometriosis is found in a significant proportion of asymptomatic infertile women.
There is fascinating new research being done whereby an endometrial sample taken in the office can diagnose endometriosis based on abnormal changes within the eutopic endometrium.8 If we can confidently rule out endometriosis without invasive surgery, it is a huge advantage. This treatment is not widely available yet.
Although the number of women having IVF for tubal occlusion due to pelvic inflammatory disease is significantly less than it used to be, the chlamydia notification rates are increasing in young people. We need to be vigilant in screening young women. For anyone with delayed fertility, it is useful to rule out current infection with an endocervical swab or first void urine for PCR testing.
Testing hormones
Measuring day 2 follicle-stimulating hormone (FSH), estradiol (E2), prolactin and thyroid-stimulating hormone (TSH) is a reasonable minimum. It is good to use this opportunity to check rubella and chicken pox immunity; blood group and infectious screen of HIV; hepatitis B and C; and Venereal Disease Research Laboratory (VDRL) tests. It is considered unnecessary in regular menstrual cycles, but luteal phase progesterone (seven days prior to the next expected period) can be reassuring.
Anti-Mullerian hormone
Anti-Mullerian hormone (AMH) is produced by the granulosa cells and regulates growth and development of follicles. It correlates highly with antralfollicle count and age, decreasing over time. AMH is stable throughout the cycle and between cycles, which makes it a useful marker of reduced ovarian reserve.10 We can also measure it when a woman is still on the contraceptive pill. In an older woman, AMH is likely to be low commensurate with her age and therefore adds no new information about her chances of conception. It can a useful test in younger women, because if an unexpected low level is found, it would prompt early referral. On the other hand, if a higher than expected level was found in an older woman, while it is good news, don’t delay referral on that basis alone. AMH levels can help to predict response to stimulation in ART.
In the presence of oligomenorrhoea, acne problems, hirsutism, alopecia and weight gain, polycystic ovary syndrome (PCOS) is easily suspected, and I would include androgen hormone testing in the follicular phase with free androgen index, dehydroepiandrosterone sulfate (DHEAS) and androstenedione. The extent of PCOS is generally under-recognised and has significant repercussions for general health and for obstetric health when pregnancy is achieved.1 I would consider measuring androgens and order a pelvic ultrasound in all patients presenting with infertility, even with regular cycles. It is possible to find polycystic ovaries with chemical hyperandrogenism in women with regular cycles and a normal BMI.
Insulin resistance is an important part of the pathophysiology of PCOS and when documented indicates a better response to metformin.10 Metformin has been shown to be safe peri-conceptually and throughout pregnancy9, in some studies improving conception rates and reducing miscarriage rates in women with PCOS.9,10
Discussing and initiating metformin use with women diagnosed with PCOS, while undergoing lifestyle measures, is something GPs can do in conjunction with endocrine/fertility specialist assessment, particularly if waiting for those specialists to be available.
Clomiphene is the drug of choice for women with infrequent or absent ovulation. GPs with an interest in managing infertility can initiate clomiphene treatment if comfortable doing so and if they have fully informed patients of the rare but possible side effect of hyperstimulation. We need to have a plan in place for investigating and managing this, should hyperstimulation occur.
Hysterosalpingogram or HyCoSy?
Imaging the patency of the tubes and uterine lining is valuable. HyCoSy (hysterosalpingo contrast sonography) is done with ultrasound while contrast is passed into the uterus and observed to pass out the end of the tubes. HyCoSy will only be available in ultrasound facilities with a skilled and experienced operator. The best way to determine if this test is available in smaller centres is to ask your local fertility specialist or fertility clinic. If HyCoSy is not available, then a hysterosalpingogram is a better choice, done at hospital radiology departments and some private practices. Both tests require a catheter to be inserted through the cervix, which can be uncomfortable, and taking pain relief an hour before the procedure is usually recommended.
The male partner
Enquire about history of testicular surgery, sexually transmitted diseases, medications taken and illicit androgen use, which will depress spermatogenesis.
Semen analysis is mandatory, even if a female factor is present, and must be performed by an experienced laboratory. The sample should be examined within an hour of being produced, so if distance from home is an issue, encourage men to go to the collecting room at the laboratory. Instructions on collection and abstinence requirements are provided by the laboratory and it is important the patient knows these details. As an initial test, basic analysis and sperm antibodies is sufficient and may cost up to A$110. If any of the parameters (sperm count, motilityand morphology) are low, it is worth repeating the test. If the parameters remain low, particularly if there are additional female contributing factors, it may be worth testing for sperm DNA integrity (sperm chromatin structure assay [SCSA]). This is an expensive test (approximately A$250) and one can manage couples well without it until invasive technologies are planned. If semen parameters are abnormal, it is indeed possible there may also be some reduced DNA integrity, but the advice remains the same: be a non-smoker; drink alcohol moderately or abstain completely; ejaculate regularly; include plenty of antioxidants in the diet; and consider antioxidant supplements for which there is some evidence of effectiveness. For a low sperm count and/or if erectile dysfunction is present, measure testosterone, luteinising hormone (LH) and follicle-stimulating hormone (FSH). Do a general medical check up for blood pressure, BMI, fasting lipids and blood suger level (BSL) (if not already known). Hypoandrogenism needs to be treated for general health and for fertility purposes will need specialist treatment, with possible testicular biopsy. A karyotype is advisable if a very low count is found.
When to refer
The rule of thumb is to refer couples to a specialist after 12 months of trying to conceive, or six months if the woman is over 35 years of age. Having a good understanding of what might be influencing a couple’s fertility means we can get a good amount of the groundwork established prior to a couple’s first appointment with the fertility clinic.
If no abnormality is found and the couple are under 35 years of age, then depending on their desires and urgency to intervene, it is reasonable to advise them their chances of conceiving without treatment are good. If the woman is over 35 years and they have been trying for six months or longer, it is appropriate to initiate referral, while encouraging the couple to continue trying to conceive, as they too have a good chance of requiring no intervention to get pregnant. With any combination of factors present, or a past history of infertility, early referral is appropriate.
References
- National Fertility Study 2006, Fertility Society of Australia. Access at: www.fertilitysociety.com.au (go to news menu).
- Dunson D, Baird D, Colombo B. Increased infertility with age in men and women. Obstetrics and Gynaecology, January 2004; 103(1).
- Dunson, et al. Impact of male age on chance of natural conception. Hum Reproduction 2002; 17:1399-4033.
- Homan G, Davies M, Norman R. The impact of lifestyle factors on reproductive performance in the general population and those undergoing infertility treatment: a review. Human Reproduction update 2007; 13(3): 209-223.
- Yang Q, Wen S , Leader A, Chen X, Lipson J, Walker M. Paternal age and birth defects: how strong is the association? Human Reproduction 2007; 22(3): 696-701.
- Smoking and reproductive life. The British Medical Association. Access at: www.bma.org.uk/health_promotion_ethics/tobacco/smokingreproductivelife.jsp.
- Wang Y, Chambers G, Dieng M, Sullivan E. Assisted reproductive technology in Australia and New Zealand 2007. 2009. AIHW.
- Al-Jefout M, Dezarnaulds G, Cooper M, Tokushige N, Luscombe G, Markham R, Fraser I. Diagnosis of endometriosis by detection of nerve fibres in an endometrial biopsy: a double blind study. Hum Reprod. Advance Access published online 18 August 2009.
- Glueck C, Wang P. Metformin before and during pregnancy and lactation in polycystic ovary syndrome. Expert Opin Drug Saf. 2007 Mar; 6(2):191-8.
- Palomba S, Falbo A, Zullo F, Orio F. Evidence-based and potential benefits of metformin in the polycystic ovary syndrome: a comprehensive review. Endocr. Rev. 2009; 30:1-50.
- Nawroth F, Ludwig M. What can we expect if we measure hormones in eumenorrhoeic infertile patients? Reproductive BioMedicine Online 2008; 16(5): 621-626.






Leave a Reply