The incidence of infertility in Australia, one in six couples, has remained the same over the last three generations and affects first and subsequent pregnancies equally.
However, societal changes, particularly later marriage and increased divorce, have impacted significantly on couples so that they might not be in a position to have children until the time their fertility has already started to decline. This decline becomes most significant for both men and women from their mid 30s onwards.
Despite enormous advances in the management of fertility problems, such as in vitro fertilisation (IVF), lifestyle factors have been virtually ignored as a preservation and/or treatment option to improve the chance of conception. Lifestyle factors are not only important to boost conception, but also to maximise a healthy periconceptional period and therefore a healthy ongoing pregnancy. Dose-dependent exposures of adverse lifestyle factors during this window can result in permanent, adverse, irreversible effects, which can continue into subsequent generations.
Much is now known about the negative impact of lifestyle issues on a couple’s fertility, in particular increased weight, smoking, excessive caffeine and alcohol intake, but unfortunately, that information has not been well conveyed to couples. For example, although cigarette smoking now accounts for 13 per cent of all fertility problems (less than tubal disease, which only makes up ten per cent), when surveyed, only one in five women knew it impacted on fertility. Even less women realised that smoking brought menopause forward by one to four years, decreasing further the time in which a woman has to conceive, particularly if she is already in her 30s. Most men are unaware that their smoking around the time of conception increases by four times the risk of the child developing a cancer in childhood.
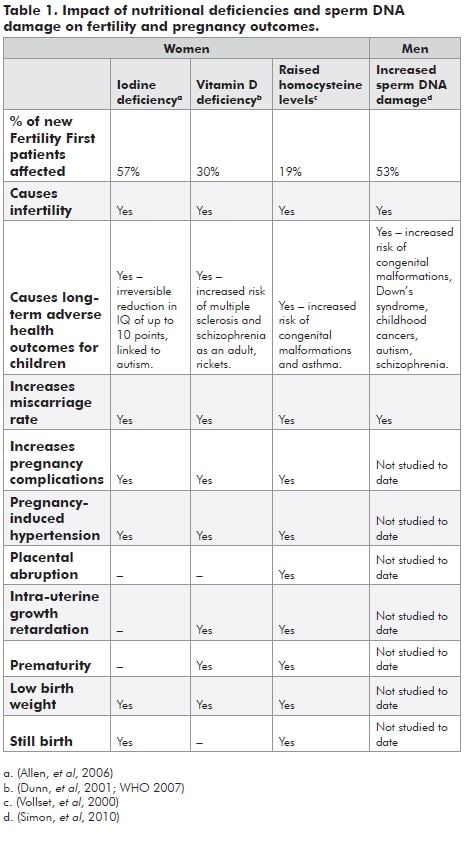
Men rarely get half the attention when it comes to fertility assessment, even though we know sperm contribute an equal amount of genetic material to a pregnancy and the placenta is largely dependent on expression of genes from the paternal chromosome. Fifty per cent of men with normal sperm counts and 70 per cent of men with abnormal sperm counts who present with fertility problems have been shown to have increased levels of sperm DNA damage. This damage reduces the chance of pregnancy, increases the miscarriage rate three to four times and can lead to genetic problems in the offspring (see Table 1). Much of this damage is due to an accumulation of lifestyle effects. Inadequate nutrition, increased weight, smoking, substance abuse and excessive coffee and alcohol intake are all lifestyle factors that increase oxidative stress, the principal cause of sperm DNA damage. Raised plasma homocysteine levels are also strongly associated with decreased fertility and poorer embryo quality. Both can be readily corrected in up to 70 per cent of affected men within two to three months with the appropriate lifestyle changes and antioxidant/nutritional supplements. This should be the first line of treatment before any other fertility program is embarked upon, otherwise chance of success will be significantly compromised.
It appears that much of what was thought to be a reduction in a woman’s fertility over time is actually a reflection of changes for both partners. The likelihood of conception for spontaneous pregnancies and IVF is halved for women 38 to 40 years of age if their partner is 40 years or older, the likelihood of miscarriage is doubled and there is an increased incidence of congenital anomalies and genetic disorders. Once both partners are aged 40, for example, half the risk of having a child with Down’s syndrome is related to the male partner alone. These poor outcomes associated with increased paternal age are once again associated with increasing sperm DNA damage as a result of increased oxidative stress, as above, and should be treated the same way.
At Fertility First, it is now routine practice for both partners to be screened for nutritional deficiencies and all men have an assessment of sperm DNA fragmentation as part of their initial assessment. Fifty-nine percent of men (n = 3264) and 62 per cent of women (n = 3986) were found to have a deficiency of folate, iodine and/or vitamin D. Fifty-three percent of men with normal sperm counts and 70 per cent of men with abnormal sperm counts had abnormal levels of sperm DNA damage. Table 1 shows the impact of these issues on fertility, fertility outcomes and the child’s long-term health.
However, apart from studies looking at cigarette smoking, alcohol and caffeine consumption and extremes of body mass index, there is very little data available on the impact of changes in lifestyle on fertility and fertility outcomes.
Fertility First’s experience is that correcting these deficiencies and/or making the required lifestyle changes, though it seems a very low key approach to a significant problem, for up to 30 per cent of couples it is the only treatment required for a spontaneous healthy ongoing pregnancy to occur.
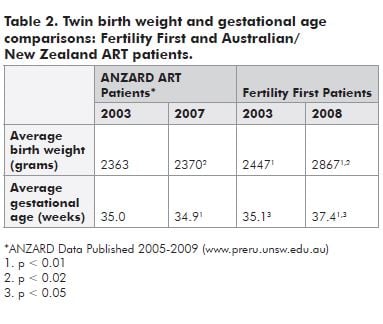
Indirect evidence of the positive effect of this approach on neonatal outcomes can be seen in outcome data for twins over the past five years. Table 2 shows the difference in birth weight and gestational age at birth for twins conceived at Fertility First, compared to the national data for all patients attending Australian and New Zealand fertility units. As periconceptional health measures have increased, there has been a corresponding significant improvement in both measures of neonatal wellbeing, compared to Fertility First’s initial 2003 statistics and to the national figures, which have shown no change over the five-year period.
There are some additional points that are important for selected patients. Firstly, women with polycystic ovarian syndrome (PCOS), who are already predisposed to higher serum homocysteine levels, should take additional B-group vitamins as well as folic acid when started on metformin therapy. After three months of metformin, there is a 27 per cent rise in homocysteine levels, but these are only decreased by eight per cent if folic acid supplementation alone is used.
Secondly, women using ‘over-the-counter’ pain relief should be warned to avoid the prostaglandin synthetase inhibitors, such as aspirin, Indocid and Nurophen, mid-cycle as they can inhibit the egg’s release from the follicle at ovulation by 50 to 100 per cent, depending on which drug is taken.
Thirdly, couples trying to conceive should be warned not to abstain until the day of ovulation. The longer the sperm sit in the testicular ducts and epididymis, the longer the exposure to oxidative stress and as a result the greater the increase in sperm DNA damage. Intercourse several days before the expected day of ovulation and on the day or day before is ideal. Normal sperm maintain their potency in a woman’s reproductive tract for up to three days, so daily intercourse is not necessary and reduces the likelihood of the couple’s physical relationship becoming one of just ‘making babies’ as opposed to making love.
To conclude, improvements in lifestyle and nutritional risk factors not only enhance the long-term health of prospective parents, but are important aspects of maximising fertility and pregnancy outcome. They are practical, cost-effective, readily amenable curative and/or preventive measures and therefore should be the first line of treatment for any fertility problems.
Fertility and reduction in fertility with increasing age is a couple issue, not just a woman’s issue, so good reproductive outcomes require an equal focus on both partners. ‘It takes two to tango.’
Infertility is a World Health Organization classified disease, it is not a choice. It is the source of much pain, not just for the couples involved but also their families. They need our support and compassion throughout the treatment process, whatever it may be.
References
- Dun JT and Delange F. Damaged reproduction: The most important consequence of iodine deficiency. J Clin Endocrinol Metab. 2001; 86, 2360-3.
- Simon L, Brunborg G, Stevenson M, Lutton D, McManus J, Lewis SEM. Clinical significance of sperm DNA damage in assisted reproduction outcome. Human Reproduction May 2010; Vol 25 No.7 pp.1594-1608.
- Vollset SE, Refsum H, Irgens L, Emblem B, Tverdal A, Giessing H, Monsen A, ueland PM. Plasma total homocysteine, pregnancy complications and adverse pregnancy outcomes: the Hordaland Homocysteine Study. American Journal of Clinical Nutrition April 2000; Vol 71, pp. 962-68.
- WHO (2004) Iodine Status Worldwide. WHO Press Geneva.






Leave a Reply