Where a woman gives birth and a baby is born has cultural, social and emotional implications far greater than is often acknowledged by many health systems and health providers. While the focus on the physical outcomes for babies and their mothers is essential, wellbeing also relies on the health system caring for the person as an integrated person. The ’non-physical‘ dimensions of a person or persons carry the potential for a positive or negative effect on their physical and mental wellbeing. There is a consequent need and demand for maternity care that is woman-, baby- and family-friendly and safe at the same time.
The land and place of one’s birth, the presence or otherwise of the family, the cultural mores, the need for environmental and cultural safety (or secure haven) within which to give birth and the burial place of the whenua (afterbirth) can all impact on the wairoa (or spiritual aspect) of a baby’s birth. These factors resonate with people across almost all cultures. The World Health Report 2005 states that, ‘There is a value in the rituals surrounding birth and in keeping these as a central feature of family life.’
Maori families in New Zealand traditionally place great emphasis on where a baby is born. Of the 3379 homebirths documented in the 2009–10 New Zealand College of Midwives Clinical database, almost 18 per cent are Maori.
Homebirth as a human right
The midwifery profession has always strongly supported women’s choice of birth place and has done for centuries. Birth at home is seen, not just as a valid choice, but as a human right. The International Confederation of Midwives (ICM) position on homebirth was reconfirmed this year at their Council meeting and it is clear: ‘The ICM supports the right of woman to make an informed decision to give birth at home supported by a midwife.’
The ICM believes that in environments where women can make a choice as to where to give birth, among the options they are able to consider for a safe birth, should be their homes. They also believe the midwife who elects to provide professional services for women in their homes should be able to do so within the nation’s health service. In the ICM statement on keeping birth normal they ’support normal childbirth since for the majority of women, pregnancy and childbirth are physiological life events.’ As part of their evidence-based approach to keeping birth normal, they specifically refer to homebirth. They say ’women should have access to midwifery-led care, one-to-one support and interdisciplinary working, including the choice of a homebirth and immersion in water.’ The ICM position goes on to say, ’ICM regrets that not all nations have the legislation or health systems which support planned homebirth, and urges national governments to review the scientific literature and work towards a maternity care system which includes this option.’
The New Zealand Government agrees with this position and homebirth is a state-supported option for all New Zealand women who choose this. Midwives providing homebirth care are also supported to do so and while many midwives attend births at home some eight per cent of midwives regularly provide a homebirth service.
In 2010, the European courts also supported the ‘rights‘ aspects of place of birth in a judgement that declared ’the choice of homebirth is a European human right.’
International Bill of Rights for Women and Midwives
ICM have also recently highlighted their commitment to human rights for women, specifically in pregnancy and childbirth and as a woman-dominated profession. At a 2009 meeting in Hyderabad, India, the Asia Pacific Region of the ICM (12 countries which included Australia and New Zealand) drafted and approved a Bill of Rights for women and midwives. They called for women in their region to be able to make their own choices around their pregnancy and birth. This statement was reinforced and approved at the ICM Council meeting in South Africa 2011. The ICM Bill of Rights lists the following as women’s rights in relation to her health and maternity; every woman has the right to:
- receive care in childbirth from an autonomous and competent midwife;
- be respected as a person of value and worth;
- security of her body;
- be free from any form of discrimination;
- up-to-date health information;
- participate actively in decisions about her healthcare and to offer informed consent; and
- privacy.
Moreover, every newborn baby has the right to a healthy and well-informed mother.
The Bill also identified that both women and midwives require the support and respect of governments if childbirth (regardless of where it takes place) is to be a safe and satisfying option for women and their newborns. ’Women and midwives have the right to be respected by governments and government institutions for health and education.’
At the same 2011 Conference, the ICM launched its new Global Competencies and Global Standards for Regulation and Education, the first profession to do so. These global statements set the standards for midwives everywhere and recognise midwives will attend and provide care wherever women and their families choose to give birth to their baby, including at home. These standards gained pledges of support from the International Federation of Obstetricians and Gynaecologists (FIGO), the WHO and the UN Population Fund.
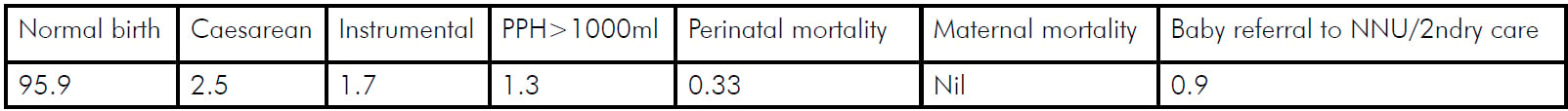
Table 1. Homebirth outcomes (%) 2009–10 (n=3379).
Homebirth in New Zealand
The New Zealand College of Midwives statement on normal birth reflects both New Zealand’s and the international midwifery position on birthplace choices and the safety of homebirth. The 2006 collaborative statement from 19 wide-ranging health professional and consumer groups, was re-ratified in 2009 and provides a further social mandate in New Zealand for this choice.
’Women who are experiencing normal pregnancies should be offered the option and encouraged to give birth in primary maternity facilities or at home. The evidence clearly demonstrates that women, who receive effective antenatal care and are assessed to be at low risk for complications, will give birth to healthy babies and need fewer interventions if they are supported to give birth in a primary maternity unit or at home.’
New Zealand women have had legislation supporting the right to a homebirth attended by a midwife since 1938. From the 1980s until the 2000s the Domiciliary Midwives Society and the Homebirth Association collected and reported data on the outcomes. A study from this considerable dataset was published in the NZ Medical Journal. The New Zealand College of Midwives has also published midwifery outcome data for homebirth since 2004, and currently has a research report in press on homebirth outcomes (see Table 1). All of these reports over seven years continue to demonstrate excellent outcomes for planned homebirth for both the mother and the baby.
However, excellent outcomes are more easily attained in an environment that is supportive of homebirth. Where there is no support, decisions are compromised as blame and legal challenge become the norm rather than the exception.
Integrated primary and secondary services
Good outcomes require the supportive continuum of care that may be needed by an individual pregnant woman from all those who provide maternity services. This collaboration is the chain that links community-based primary midwifery care with district and regional care from hospital-based midwives and medical specialists.
It is the positive and supportive relationships between midwives and obstetricians that make a homebirth service safe and trustworthy for women and their families. It is the maturity of New Zealand maternity services and the good relationships between midwife and obstetric colleagues that enables the safe homebirth option. In fact, about 20 per cent of births in New Zealand occur in localities without on-site medical back-up, which has allowed this country to develop more mature systems of consultation and referral. The outcomes of these births are excellent. For example, the adjusted relative risk of emergency caesarean section for women of the same risk status at a homebirth is 0.81(0.56–1.15) compared to an adjusted relative risk of 2.73 (2.17–3.44) in a secondary hospital (p<0.001) and 4.62 (3.66–5.84) (p<0.001) in a tertiary hospital.
Consultation and Referral Guidelines contribute to each discipline’s understanding of risk. These have been in place since 1996, and have stood the test of time. They were reviewed by a multidisciplinary team in 2011, with minor changes and coding clarifications. The Guidelines are owned and respected by all parties and help assist everyone to make sound and safe decisions about when another level of care is required.
Midwives know that if they need to transfer to hospital they will be received by obstetricians that respect their expertise and support the woman’s right to minimum intervention. The women are treated with respect and care plans maintained as much as possible in light of the need for transfer and obstetric involvement. Midwives and women are not castigated for opting to give birth at home, but supported when they are admitted to hospital due to circumstances that require extra obstetric support. This supports safety because women (and their midwives) know that their treatment at hospital will continue to respect and support the woman’s choices as much as possible.
At each level of care, women should receive respect, quality care, timely consultation and referral when necessary to doctors, midwives and other specialists. The collaboration between midwives, specialists, other health professionals and consumer groups should be constructive and focused on women’s and babies needs at every level. If professional care and services are accessible, integrated, responsive, affordable and effective the issue of where a women and her family choose to give birth will be factor of the past.
References are available from the author upon request.






Leave a Reply