Q&a attempts to provide balanced answers to those curly-yet-common questions in obstetrics and gynaecology for the broader O&G Magazine readership, including Diplomates, Trainees, medical students and other health professionals.
Should I request a routine cervical length scan at 20 weeks in all women?
Cervical length measurement is commonly used in women with risk factors for preterm birth to more accurately predict those at highest risk who may benefit from interventions such as cervical cerclage or progesterone therapy. Recent clinical trials have also explored the potential of these interventions in women with short cervices, with or without other risk factors. A demonstration of a reduction in preterm birth rates associated with progesterone use has led some to suggest that universal cervical length screening should be introduced.
Maternity care providers are therefore asking the important question as to whether or not a routine cervical length should be done in all women at the time of the second trimester ultrasound. Indeed, in some settings this is being done as part of the routine scan without any specific request or even knowledge of the woman and her caregiver. However, before introducing a policy of universal cervical length screening there are several questions that should be asked and considered.
What test should we use, is it acceptable and reliable?
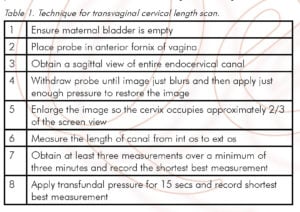
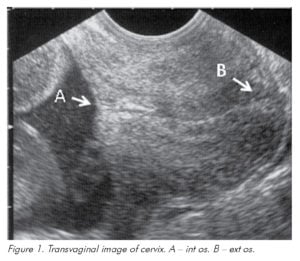
A transvaginal scan is the gold standard test for measurement of cervical length.1 It is easily reproducible2 when accepted methodology3 is followed (see Table 1 and Figure 1) and the vast majority of women have only mild or no discomfort associated with the test.2 The predictive ability of many different cervical parameters have been assessed including funnel length, funnel width, cervical index, loss of cervical plug and altered mucus glands. However, functional (closed) cervical length is the best single predictor and these other parameters do not appear to add significantly to the predictive value.
The alternative of an initial transabdominal approach followed by a transvaginal scan if the cervical length is short has been proposed4, but has not yet been evaluated in large studies. This may have the advantage of being more acceptable to women and easier to implement in a routine setting. However, recent intervention studies have been based on transvaginal measurement and so, if we are to consider routine cervical length screening to select patients for these interventions, a transvaginal scan should always be undertaken, performed by someone skilled and experienced in the technique.
How good is the test?
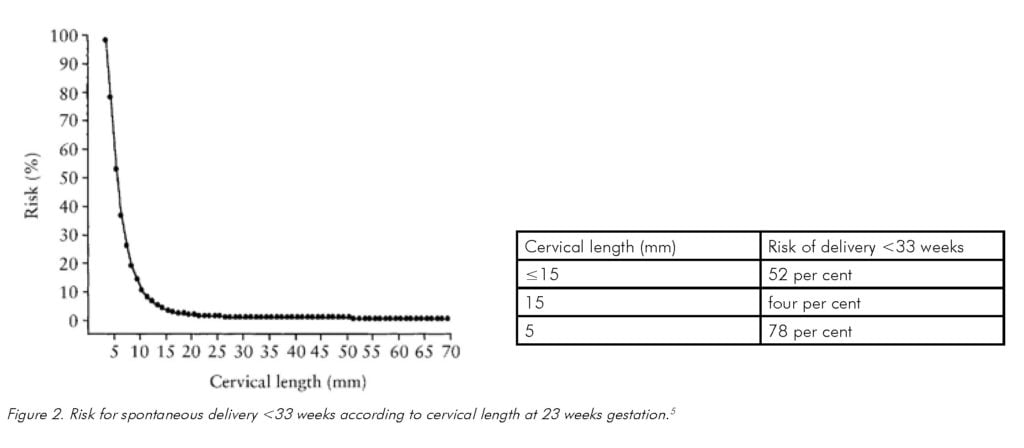
It is clear that the relative risk of preterm delivery increases as the length of the cervix decreases3, but it is less clear how short the cervix must be before an intervention should be considered in a low-risk population. The majority of prediction studies using cervical length have been in general populations, which include women with risk factors for preterm birth, multiparous women with no previous preterm birth and nulliparous women.5,6 It is likely that for each of these groups of women the test and potential interventions will behave differently and this should be considered when reviewing their results.
One of the earliest prediction studies is from a UK general population, including 2567 women with a cervical length measurement at 23 weeks gestation, identifying women with a very short cervix (≤15mm).5 Of 43 women with a cervical length ≤15mm, only 21 were observed (the remainder had a cervical cerclage) and compared to 1231 women with a cervical length ≤15mm. The test identified 58 per cent of the women delivering <33 weeks gestation and the overall risk of delivery <33 weeks with cervical length ≤15mm was 52 per cent. However, the risk rose exponentially in those with a short cervix (see Figure 2). This suggests the cervix must be very short to significantly increase the risk of early preterm birth. Similar risks of preterm birth with cervical length ≤15mm were seen in a study of a general US population where scans were performed at a mean gestational age of 19 weeks.6 For delivery <33 weeks, a cervical length ≤15mm had a positive predictive value of 47.6 per cent, negative predictive value of 96.7 per cent, sensitivity of 8.2 per cent and specificity of 99.7 per cent.
It should be noted that the prevalence of a very short cervix in a general population is low, with only 1.7 per cent and 0.6 per cent of the populations in the UK and US studies respectively having a cervical length ≤15mm. Similar low prevalence rates have been seen in much larger population screening for intervention studies with cerclage (one per cent ≤15mm)7 and progesterone (1.7 per cent ≤15mm and 2.3 per cent 10–20mm)8,9, however, again these studies include women at varied risk. In the SCOPE study of nulliparous women in an Australian and New Zealand population (likely to be at lower risk than a general population) only 0.5 per cent of women had a cervical length ≤20mm at 18–23 weeks (personal communication).
A very short cervical length is associated with an increased risk of early preterm birth; however, a very short cervix has a low prevalence in a general population. If women with previous preterm births are excluded the prevalence is even lower and so very large numbers of women need to be screened to find a small number of cases that may benefit from possible interventions.
What can we do about the result?
The two main interventions that have been considered are cervical cerclage and progesterone therapy. However, these have been applied to different populations of women and the results need to be considered in this context.
Women with risk factors for preterm birth
Cervical cerclage for a short cervix has been demonstrated to be beneficial in women at high risk. A recent meta-analysis of randomised trials included 504 women with singleton pregnancies, a history of preterm birth and a short cervical length. All but one study randomised women to cerclage or no cerclage with a cervical length <25mm (one study ≤15mm). Cerclage was associated with a reduction in the rate of delivery <35 weeks from 45 per cent to 28 per cent (RR 0.70, 95 per cent CI 0.55–0.89).10
There are no specific trials of progesterone in high-risk populations with a short cervix, but subgroup analysis of women with a history of previous preterm birth in the most recent progesterone trial
in women with a cervical length 10–20mm demonstrated no significant difference in preterm birth rates <33 weeks (16 per cent versus 21 per cent, RR 0.77 95 per cent CI 0.3–2.1). However, the study was not powered for this small subgroup. It is unlikely that further intervention trials in high-risk women with a short cervix will be undertaken as progesterone has been demonstrated to reduce rates of preterm birth when used in women with a history of preterm birth, regardless of cervical length.11,12
Women with no risk factors for preterm birth
There are no specific studies assessing cervical cerclage in women with a short cervix with no history of preterm birth. However, in a general population with a short cervix (≤15mm) at 23 weeks gestation, despite the inclusion of women with previous preterm birth, cervical cerclage has no apparent affect on early preterm birth.7
Progesterone therapy has been associated with a reduction in preterm birth in two studies of women in a general population with a short cervix. The first published study included twin and singleton pregnancies and randomised women with a cervical length ≤15mm at 20–25 weeks to placebo or 200mg of vaginal micronised progesterone.9 The rate of delivery <34 weeks was lower in the progesterone group, 19 per cent versus 34 per cent (RR 0.56 95 per cent CI 0.4–0.9) and the relative risk did not seem to vary regardless of obstetric history but was non-significant when analysed as independent groups. In the more recent published study of singleton pregnancies, women with a cervical length 10–20mm at 19–24 weeks were randomised to placebo or 90mg of vaginal progesterone gel.8 Again, progesterone use led to a significant reduction in early preterm birth and this was significant when assessing only women without a history of preterm birth, eight per cent versus 15 per cent (RR 0.5 95 per cent CI 0.3–0.9).
It has therefore been demonstrated that once a short cervix has been identified, progesterone is likely to be beneficial. However, it is important to note that very large numbers of women were screened in both studies to identify only a very small group who may have benefited from the intervention. Over 24 000 women were screened to identify 413 women with a cervical length ≤15mm and over 32 000 women to identify 733 women with a cervical length 10–20mm.8,9
Summary
Current evidence and practice supports cervical length scanning in women with previous preterm birth. Cervical cerclage has been shown to be of benefit in these women if they develop a short cervix. Other interventions such as elective cerclage and routine use of progesterone invite further debate and, at present, should be considered on an individual basis according to risk. The same applies for additional risk factors such as large cone biopsy and congenital uterine/cervical anomalies.
As for women without risk factors for preterm birth, recent evidence from clinical trials supports the use of progesterone in the event of an incidental finding of a short cervix in an asymptomatic low-risk woman. However, these trials do not yet support routine cervical length measurement in all women. To accurately assess if there is a benefit to such a change of practice, both in terms of clinical outcome and cost, a randomised trial of a policy of screening with treatment in the event of short cervix would be required. Such a study will help to determine if routine cervical length scanning at 20 weeks ultimately improves outcome and if it should be introduced to antenatal care for all. The health benefits and economic aspects of such a screening program would need to be carefully considered in any interpretation of the results.
References
- Mella, M.T. and V. Berghella, Prediction of preterm birth: cervical sonography. Semin Perinatol, 2009. 33(5): p. 317–24.
- Heath, V.C., et al., Cervical length at 23 weeks of gestation: relation to demographic characteristics and previous obstetric history.
Ultrasound Obstet Gynecol, 1998. 12(5): p. 304–11. - Iams, J.D., et al., The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med, 1996. 334(9): p. 567–72.
- Stone, P.R., et al., Transabdominal scanning of the cervix at the 20-week morphology scan: comparison with transvaginal cervical measurements in a healthy nulliparous population. ANZJOG, 2010. 50(6): p. 523–7.
- Heath, V.C., et al., Cervical length at 23 weeks of gestation: prediction of spontaneous preterm delivery. Ultrasound Obstet Gynecol, 1998. 12(5): p. 312–7.
- Hassan, S.S., et al., Patients with an ultrasonographic cervical length < or =15 mm have nearly a 50 per cent risk of early spontaneous preterm delivery. AJOG, 2000. 182(6): p. 1458–67.
- To, M.S., et al., Cervical cerclage for prevention of preterm delivery in women with short cervix: randomised controlled trial. Lancet, 2004. 363(9424): p. 1849–53.
- Hassan, S.S., et al., Vaginal progesterone reduces the rate of preterm birth in women with a sonographic short cervix: a multicenter, randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol, 2011. 38(1): p. 18–31.
- Fonseca, E.B., et al., Progesterone and the risk of preterm birth among women with a short cervix. N Engl J Med, 2007. 357(5): p. 462–9.
- Berghella, V., et al., Cerclage for short cervix on ultrasonography in women with singleton gestations and previous preterm birth: a meta-analysis. Obstet Gynecol, 2011. 117(3): p. 663–71.
- da Fonseca, E.B., et al., Prophylactic administration of progesterone by vaginal suppository to reduce the incidence of spontaneous preterm birth in women at increased risk: a randomized placebo-controlled double-blind study. AJOG, 2003. 188(2): p. 419–24.
- Meis, P.J., et al., Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med, 2003. 348(24): p. 2379–85.







Leave a Reply