Less than one per cent of all births in Australia are planned homebirths, yet the topic continues to provoke heated discussion between advocates for increased support and funding of homebirth services, and opponents of such measures.1–11 Much of the discussion is informed by reference to homebirth services in other developed countries, including Canada, the UK, New Zealand, the USA and, particularly, the Netherlands, in the latter case usually with an implication that the Dutch system could serve as a model for Australia.5–9,11 Of developed countries, the Netherlands has the highest rate of planned homebirths supervised by midwives, with the availability of transfer to obstetric care if needed: currently 30 per cent of all births, a figure down from 35 per cent in 1979 and 74 per cent in 1958.12,13 In this article we review all reports and studies of homebirth in Australia published in the period 1990–2011, together with relevant peer-reviewed literature regarding homebirth from the same timeframe from the Netherlands, with the aim of assessing overseas experience that might be relevant to Australian practice.
Homebirth in the Netherlands
Midwives in the Netherlands do not require prior training in nursing, but undertake four years of training in midwifery schools, including working with midwives in independent practice. Qualified midwives have been formally recognised as autonomous practitioners in the care of normal pregnancy and childbirth since 1941. Most now work in group practices, each midwife averaging 110 deliveries annually. They are legally permitted to undertake certain intrapartum interventions, including perineal suturing, but may not perform instrumental deliveries, fetal electronic monitoring or labour augmentation.12,13,14
Any pregnant woman in the Netherlands can refer herself directly to a midwife and provided she remains within certain defined risk criteria, the midwife can undertake all maternity care, with the delivery being conducted either at home, in a kraamhotel (maternity hostel) or in a polyclinic attached to a hospital. Responsibility for deciding that a woman fulfils the risk criteria lies with the midwife. A list of medical indications that would exclude a woman from midwife-only care has been developed in conjunction with Dutch obstetricians.15 About 15 per cent of women are initially judged as high risk and therefore unsuitable for midwife care and the percentage of deliveries performed or overseen by hospital doctors, usually obstetricians, has risen from 28 per cent in 1970 to around 50 per cent in 2010.12,15
Under the Dutch system, women are assigned to the midwife on-call on the day of booking. In the course of her antenatal care, a woman can expect to meet all the midwives in the group so that those attending her in labour and birth will be known. All routine antenatal investigations are organised by the midwife, with obstetric referral if abnormal results so indicate; the decision for referral is made by the midwife under the criteria already described.
There are three ‘lines’ of maternity care in the Netherlands. The first consists of midwives only, who provide care for women (in any setting) provided pregnancy and birth remain normal. The second line includes hospital midwives caring for higher risk women under the supervision of an obstetric team (as occurs in Australian public hospitals). The third line of maternity care is that provided directly by medical practitioners including subspecialist obstetricians.12,15,16 A first-line midwife must be able to reach the home of any woman booked for homebirth within 15 minutes and emergency care should be not more than 15 minutes away by ambulance. A midwife conducting a labour at home is not necessarily present throughout the first stage, but will call frequently to the woman’s home to check on her condition and progress. Thus a single midwife may involve herself in a woman’s care over 24 hours or more.16,17
The cost of maternity care is covered by private health insurance schemes. Where the woman has care provided entirely by first-line midwives, the full cost is covered by insurers, as it is when there is a medical indication for hospital care. Where the woman chooses hospital care for no medical indication, she is liable for at least some of the cost, dependent on the level of insurance she holds. First-line midwives are independent practitioners, owning their practices and billing insurers for their fees. Insurance funds will not cover maternity care by general practitioners in districts where a midwife is in practice; general practitioners attend only about four per cent of births in the Netherlands. Funding schemes therefore tend to direct low-risk women towards homebirth or other forms of first-line care.12
The Dutch system is designed to allow the smooth transfer of women from first- to second- or third-line care.16 Where urgent transfer is required, the regular Dutch ambulance service is used and the midwife accompanies the woman to the hospital, with which she has been encouraged to become familiar with during her pregnancy.17,18 Over the last two decades there have been increasing numbers of transfers to second- or third-line care. In a large retrospective study of transfers, involving nearly two million pregnancies between 1988 and 2004, the proportion of women transferred increased from 36.9 per cent of all those booked for first-line care to 51.4 per cent.12
Another large retrospective study included 280 000 women who were under the care of a midwife at the time of starting labour (either at home or in a clinic/hospital) during the period 2001–03.16 Women in preterm labour or who were referred for induction of labour were excluded. Sixty-eight per cent of the women completed childbirth under midwife care and 32 per cent were referred for hospital care, with 11.2 per cent of those being urgent referrals.
Midwives conducting home and hospital births are authorised to administer nitrous oxide gas and narcotic analgesia. There has been a strong tradition in Dutch homebirth practice of not encouraging pharmaceutical pain relief in labour that recently has come under scrutiny. Dutch feminists have called for the right of women to pain relief, in particular with epidural analgesia, and questioned ‘the ideology of natural delivery and the positive meaning attached by midwives to women’s capacity to deal with pain without pharmacological support’.19 Following a 2006 directive from the Dutch Ministry for Health, women may now access epidural analgesia on request, but if they are under first-line care they must be transferred.20 Epidural analgesia is now used in 22 per cent of hospital births.
From 1993–2002, the caesarean rate for the Netherlands rose from 8.1 per cent to 13.6 per cent. However, current rates in hospital practice are reported at approximately 24 per cent, with an overall national rate of around 16 per cent, considerably lower than rates in most other European countries, North America and Australia.21–23
The maternal mortality rate (MMR) in the Netherlands has increased since 1983–92, when it was 9.7 per 100 000 live births.24 In the period 1993–2005 the MMR was 12.1 per 100 000 births (in comparison, the Australian MMR for 2003–05 was 8.4 per 100 000).25 Women aged less than 20 years or more than 45 years, those of high parity and those from non-European immigrant populations were all at greater risk of pregnancy-associated death, and there has been an increase in the numbers of such women in the pregnant population of the Netherlands over the last two decades, although the same is also true of Australia.
In 1999, the perinatal Dutch perinatal mortality rate (PMR) was substantially higher than in other European countries.26,27 A retrospective study of all Dutch births in the period 2000–06 reported an improvement, with a decline in the PMR from 10.5 to 9.1 per 1000 births (in the same period, the Australian PMR was 8.2 per 1000).27,28,29 The high PMR was attributed to formerly restrictive policies on the resuscitation and intensive care of very preterm infants, the absence of antenatal screening programs for congenital anomalies and ‘substandard care, including homebirth’.27 The decline in PMR noted by 2000–06 was most marked among very preterm infants and births complicated by congenital anomalies. Table 1 summarises all relevant Dutch studies comparing outcomes of women booked for homebirth with women booked for hospital birth in the last 20 years. These studies show that where low-risk women are booked for homebirth and deliver at home, perinatal outcomes are similar to those of low-risk women booking in hospital under midwife care and delivering in that setting. When women are transferred from low-risk to high-risk care intrapartum, perinatal death rates rise. In the single, but important, study in which PNM among infants of high-risk women booking for hospital care by obstetricians was compared to that of low-risk women booking for ‘low-risk’ midwife-led care, PNM was lower in the former group.29
In 2009, a committee was appointed by the Dutch Minister for Health to investigate perinatal mortality rates. Among contributing factors, the committee noted increasing age at first pregnancy among native-born Dutch women, late booking by women at high-risk of pregnancy complications, failure of collaboration between the different lines of care and the fact that a significant proportion of homebirth women lived farther from a hospital than recommended.20
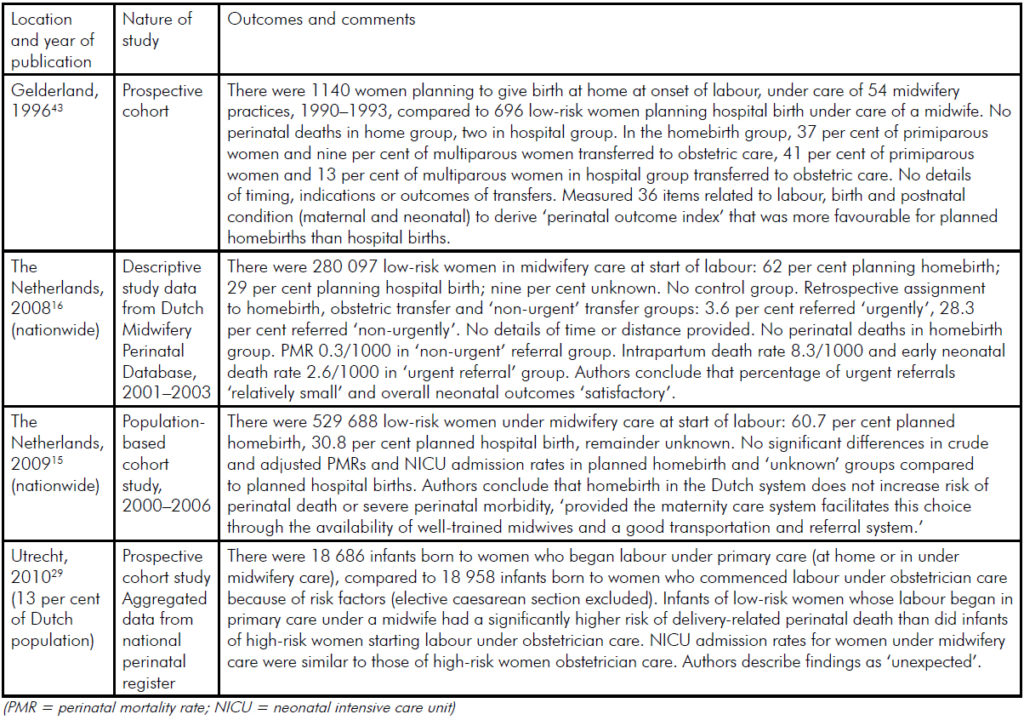
Table 1. Summary of comparative homebirth studies from the Netherlands, 1990–2010.
Homebirth in Australia
RANZCOG does not endorse planned homebirth, outlining the reasons in its statement C-Obs2 (see p58). Most currently practising midwives in Australia are nursing graduates with a further 12 months of midwifery training. However, direct-entry three-year Bachelor of Midwifery courses are being offered by increasing numbers of Australian universities. Both courses aim to prepare students for hospital-based midwifery practice. It has been suggested the graduates of direct-entry midwifery courses may be more inclined to pursue careers involving the provision of homebirth care, although no evidence has been offered for this.7
Current Australian obstetric and midwifery practice includes a booking visit with a medical practitioner, who makes the decision, when required, as to whether a woman is medically low risk and therefore suitable for midwife-led care. Where formal homebirth programs have been established in Australia, as in the St George Hospital program in Sydney (see article on p44), obstetricians act as direct referral sources in the event of an abnormality arising.11
Some established Australian homebirth programs, for example St George, have replicated aspects of Dutch care in limiting planned homebirth to women living within defined geographical regions around a base hospital to which midwives and supporting medical staff are attached.11 Midwives work both in the hospital and in the homebirth service and good relationships are reported between midwifery and medical staff. Normal ambulance services are used for transfer to hospital when required. In all Australian studies and reports, there is reference to the fact that women seeking homebirth are older, of higher educational, social and employment status and are less likely to smoke, than women giving birth in hospital.
Table 2 summarises all studies and reports on homebirth in Australia published since 1990.30–36 Apart from the St George report, all studies are retrospective. Two are simply descriptive and have no control groups; among the other four, three have control groups of state-wide hospital births that would have included those to many medium- and high-risk women (including in some cases women planning a homebirth, but transferred to hospital due to some complication of pregnancy or birth). Only one has a matched control group, but although women in this are matched for age, parity, social status and previous pregnancy loss they are not matched for medical and obstetric complications in the index pregnancy.
The St George study includes 100 women over a period of three-and-a-half years, of whom 30 were transferred to hospital care antenatally. Of the remaining 70 women, 63 gave birth at home (where each was attended by two midwives) and seven (ten per cent) were transferred intrapartum. Women were assessed as low-risk by an obstetrician prior to their acceptance into the program. There was no perinatal mortality or significant morbidity reported.11
In all other studies and reports, the homebirth groups contained women with important obstetric risk factors, including previous caesarean section, previous perinatal death and breech presentation or twins in the index pregnancy. In most cases the birth attendant was a registered midwife, although on occasion births were attended by lay midwives or by medical practitioners. In all studies and reports where perinatal death rates are reported these are either similar to those reported for hospital births (whereas they might be expected to have been lower, if only low-risk women had been selected for planned homebirth) or are significantly higher for homebirths. No details are given of proximity to available obstetric care, either geographically or in terms of the time required for transfer, in any study or report apart from the St George study.11,30–36
That the option of homebirth is widely accepted in the Netherlands, generally functions well and is appreciated by many Dutch women is indisputable. However, there has been animated discussion about the safety and appropriateness of first-line care following increased public awareness of Dutch perinatal mortality figures and the input of Dutch feminists into the rights of women to choice in childbirth.
The long tradition of homebirth, the very specific training of midwives and the existence of an established body of first-line midwives and women delivering at home indicate that a very different environment exists for the provision of safe homebirth services in the Netherlands, in comparison to the current Australian situation. The Netherlands is a western European country with an area of 41 500 sq km, a population of 16.5 million and a birth rate of 10.4 (per 1000 of the population per year); in comparison, Australia has an area of 7.7 million sq km, a population of 22.5 million and a birth rate of 12.4.37,38 The small size of the Netherlands and the high urban density mean emergency services are, in general, able to respond to requests for urgent transfer within prescribed time limits. The number of women delivering at home and being transferred also means emergency services personnel are more familiar with intrapartum complications that may need to be dealt with during the journey to hospital.
While 89 per cent of Australian women live in urban areas, those areas are considerably more dispersed than in the Netherlands and ensuring safe transfer in urgent cases may pose problems. The homebirthing woman transferred to hospital in the Netherlands finds herself part of a system specifically designed to take over her care. In Australian programs, such as St George, this is also the case, but in other areas of Australia obstetricians are called upon to deal with unbooked homebirthing women arriving suddenly in the hospital birth suite, often out of hours, requiring considerable input from staff having little access to information about their previous care.4,11,39,40
An increasing proportion of women in the Netherlands initially booked for homebirth and considered low risk by first-line midwives are nevertheless transferred to hospital, either antenatally or intrapartum. Medical claims and litigation are still exceptional in Dutch midwifery practice so defensive obstetrics is not a significant cause of these increased numbers of transfers. It does appear that women at increased risk are not always identified or transferred to second- and third-line services in a timely manner. This phenomenon has been noted in several Australian homebirth studies, where independent homebirth midwives have accepted women for planned homebirth who were not low risk.1,39,40
The 12th Triennial Western Australia (WA) Report of the Perinatal and Infant Mortality Committee in 2007, recommended a review of homebirths in that state, after identification of a higher mortality rate in term neonates whose mothers had planned a homebirth compared to planned hospital births.41 The review, duly conducted in 2008 by Dr Michael Nicholl and Prof Caroline Homer, made a number of recommendations concerning homebirth practice in WA, including: improved mechanisms for the assessment, accreditation and registration of homebirth midwives, and for improved systems for professional development and clinical governance; the identification of planned homebirths in perinatal data collections; and the auditing of all homebirth outcomes.36,40 Nevertheless, in December 2010, in its 13th Report, the Committee noted with concern that the perinatal death rate for term homebirths in WA remained almost four times higher than that for hospital term births. The Committee recommended an independent audit of the implementation of the recommendations of the 2008 Review, and commented that some women were choosing homebirth ‘as a surrogate means to access midwifery continuity of care and waterbirth.’40 It should also be noted that comprehensive guidelines for homebirth published by the South Australian Department of Health in 2007 have not yet been implemented in that state.42
As well as raising questions about rates of adverse outcomes for both mothers and babies, lessons for advocates of increased access to homebirth in Australia include the vastly different demographic features of the two countries, the differences in midwifery training and the structured relationships between all lines of maternity care in the Netherlands.43 While some of the features of the Dutch system have proved portable to Australia, others have not and in many outer suburban and rural areas safe care on the Dutch model could not be replicated in current Australian practice.
Although impossible to determine from Australian studies, evidence from overseas – in particular from the Netherlands, which may or may not relate to the Australian situation – suggests that homebirth for women who are carefully screened and who plan to deliver at home, but with sympathetic collaborating hospital staff, may be as safe as delivering under midwifery care in hospital/birth centre settings, although not as safe as in obstetrician-led care.12,29,43 This presupposes that the woman lives an acceptable distance from the hospital, with accessible emergency transport systems. It is likely that serious adverse outcomes are reduced where midwives have an adequate caseload (possibly combined homebirth/hospital practice). However, for the small proportion of low-risk women who develop serious intra- or postpartum complications, outcomes are probably worse than for women having conventional hospital care. Where high-risk women are accepted for homebirth then outcomes are, and will be, correspondingly poorer.
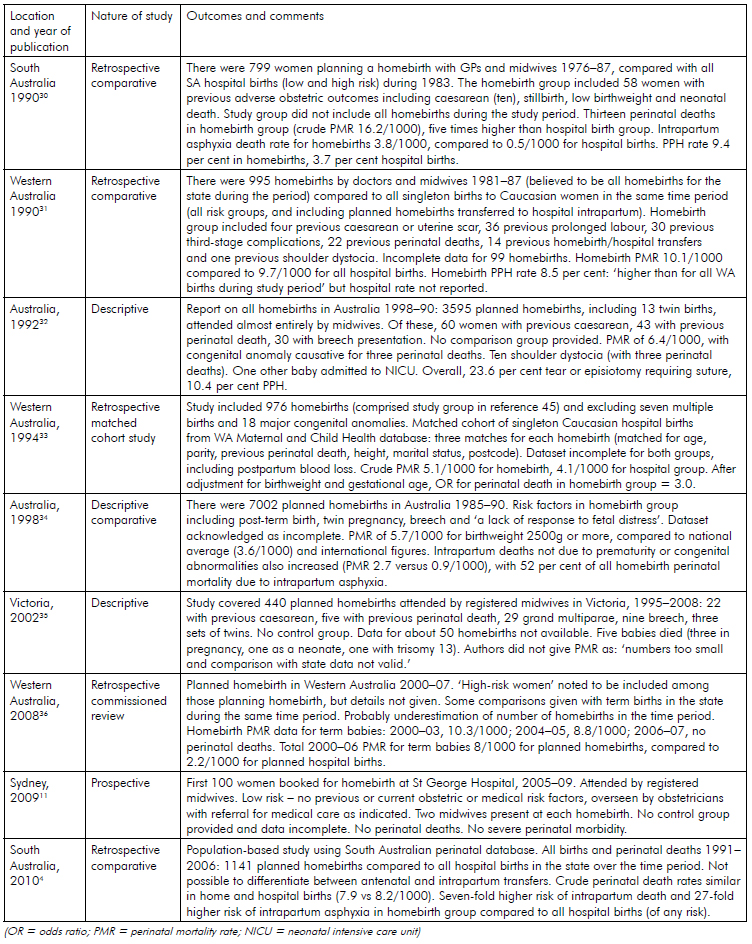
Table 2. Summary of Australian homebirth studies and reports, published 1990–2011.
Acknowledgements
We would like to thank all those Dutch medical practitioners, midwives and women who have experienced maternity care in the Netherlands who assisted one of us (HP) during a two-month visit to the Netherlands in 2010, when much of the research for this article was undertaken. Special thanks to Marlen Rauch and Tineke De Backer. Thanks also to A/Prof Stephen Robson for his input during the writing of this article.
References
- Pesce AF. Planned homebirth in Australia: politics or science? MJA 2010; 192; 60–61.
- Newman LA. Why planned attended homebirth should be more widely supported in Australia. ANZOG 2008; 48: 450–53.
- Harvey J. Comment on – Why planned attended homebirth should be more widely supported in Australia (letter). ANZJOG 2009; 49:340–41.
- Kennare RM, Keirse MJNC, Tucker GR, Chan AC. Planned home and hospital births in South Australia, 1991–2006: differences in outcomes. MJA 2010; 192: 76–80.
- Dahlen HG, Homer CSE, Tracy S, Bisits AM. Planned home and hospital births in South Australia, 1991–2006: differences in outcomes (letter). ANZJOG 2010; 192: 726.
- Johnson KC, Daviss B. Planned home and hospital births in South Australia, 1991–2006: differences in outcomes (letter). ANZJOG 2010; 192: 726–7.
- Kennare RM, Keirse MJNC, Tucker GR, Chan AC. Planned home and hospital births in South Australia, 1991–2006: differences in outcomes (letter). MJA 2010; 192: 727.
- Smith H. Cascade of interventions (letter to the editor). The Australian, 21/1/10: 13.
- Christensen P. Opinions divided on a special delivery. The Australian, 10-11/4/10: 10.
- Miles J. Star baby birth raises home risk. Brisbane Courier Mail, 9/7/10:20.
- McMurtrie J, Catling-Paul C, Teate A, et al. The St George Homebirth Program: An evaluation of the first 100 booked women. ANZJOG 2009; 49: 631–36.
- Amelink-Verburg MP, Rijnders ME, Buitendijk SE. A trend analysis in referrals during pregnancy and labour in Dutch midwifery care 1988–2004. BJOG 2009; 116: 923–32.
- Tew M, Damstra-Wijmenga SMI. Safest birth attendants: recent Dutch evidence. Midwifery 1991; 7: 55–63.
- Van Der Hulst LA, Van Teijlingen ER, Bonsel GJ, et al. Does a pregnant woman’s intended place of birth influence her attitudes toward and occurrence of obstetric interventions? Birth 2004; 31: 28–33.
- De Jonge A, van der Goes BY, Ravelli AC, Amelink-Verburg MP et al. Perinatal mortality and morbidity in a nationwide cohort of 529,688 low-risk planned home and hospital births. BJOG 2009; 116 (9):1177–84.
- Amelink-Verburg MP, Verloove-Vanhorick SP, Hakkenberg RMA, et al. Evaluation of 280,000 cases in Dutch midwifery practices: a descriptive study. BJOG 2008; 115: 570–8.
- Bonsel GJ, Birnie E, Denktas S, Poeran J, Steegers EAP. Lijnen in de Perinatale Sterfte: Signalementstudie Zwangerschap en Geboorte 2010 [‘Trends in Perinatal Mortality: Signalstudy Pregnancy and Birth 2010’]. Rotterdam: Erasmus Medical Centre, 2010.
- Stuurgroep Zwangerschap en Geboorte. Een Goed Begin: Veilige Zorg Rond Zwangerschap en Geboorte [‘A Good Start: Safe Care around Pregnancy and Childbirth’]. Advice to Minister of Health. Amsterdam, 2009.
- Hardon, A. Reproductive Health Care in the Netherlands: Would Integration Improve It? Reproductive Health Matters 2003; 11: 59-73.
- Effting M. ‘In Nederland Sterven Onnodig Baby’s’ [‘In the Netherlands Babies Die Unnecessarily’] Volkskrant, 21 Oct 2009. At www.volkskrant.nl/2009/10/21/lsquo-In-Nederland-sterven-onnodig-baby-s-rsquodhtml accessed 5/11/10.
- Kwee A, Bots ML, Visser GHA, Bruinse HW. Obstetric management and outcome of pregnancy in women with a history of caesarean section in the Netherlands. EJOG 2007; 132: 171–6.
- Kwee A, Elferink-Stinkens PM, Reuwer PJ, Bruinse HW. Trends in obstetric interventions in the Dutch obstetrical care system in the period 1993–2002. EJOG 2007; 132: 70–75.
- Van Dillen J, Lim F, van Rijssel E. Introducing caesarean section audit in a regional teaching hospital in The Netherlands. EJOG 2008; 139:151–6.
- Schutte J, Steegers E, Schuitemaker N, et al. The Netherlands Maternal Mortality Committee. Rise in maternal mortality in the Netherlands. BJOG 2010; 117: 399–406.
- Perinatal and Reproductive Epidemiology Unit, UNSW. Maternal deaths in Australia 2003-2005. At www.preru.unsw.edu.au accessed 30/10/0.
- Buitendijk S, Zeitlin J, Cuttini M, Langhoff-Roos J, Bottu J. Indicators of fetal and infant health outcomes. EJOG 2003; 111: s66–77.
- Ravelli AC, Tromp M, van Huis AM, et al. Decreasing perinatal mortality in the Netherlands, 2000-2006: a record linkage study. J Epidemiol Community Health 2009; 63: 761-5.
- ACT Health. Report of Perinatal Mortality in the ACT 2001–2005. At www.health.act.gov.au/c/health accessed 30/10/10.
- Evers ACC, Brouwers HAA, Hukkelhoven CW, et al. Perinatal mortality and severe morbidity in low and high risk term pregnancies in the Netherlands: a prospective cohort study. BMJ 2010; 341: c5639.
- Crotty M, Ramsay AT, Smart R, Chan A. Planned homebirths in South Australia 1976-1987. MJA 1990; 153: 664–71.
- Woodcock HC, Read AW, Moore DJ, Stanley FJ, Bower C. Planned homebirths in Western Australia 1981–87: a descriptive study. MJA 1990; 153: 672–8.
- Bastian H, Lancaster. Homebirths in Australia 1998–90. AIHW/NPSU and Homebirth Australia, 1992.
- Woodcock HC, Read AW, Bower C, Stanley FJ, Moore DJ. A matched cohort study of planned home and hospital births in Western Australia 1981–1987. Midwifery 1994; 10: 125–35.
- Bastian H, Keirse MJNC, Lancaster PA. Perinatal death associated with planned homebirth in Australia: population-based study. BMJ 1998; 317: 384–8.
- Parratt J, Johnston J. Planned homebirths in Victoria, 1995–1998. Aust J Midwifery 2002; 15: 16–25.
- Homer C, Nicholl M. Review of homebirths in Western Australia. Department of Health, Western Australia, 2008.
- Netherlands. At www.cbs.nl accessed 5/11/10.
- Australian Bureau of Statistics. Population clock. At www.abs.gov.au accessed 5/11/10.
- O’Sullivan B, Bushati T, Ho T. Homebirth transfers at Lismore Base Hospital – a retrospective survey. O&G Magazine 2009; 11: 31–33.
- Dept of Health, Western Australia.13th Report of the Perinatal and Infant Mortality Committee of Western Australia for Deaths in the Triennium 2005–07. Government of Western Australia, 2011.
- 12th Report of the Perinatal and Infant Mortality Committee of Western Australia, Deaths 2002-2004. Office of the Executive Director, Dept of Health, WA, Perth, 2007.
- Government of South Australia, Department of Health. Policy for Planned Birth at Home in South Australia. Adelaide: 2007, SA Department of Health.
- Wiegers TA, Keirse MJNC, van der Zee J, Berghs GAH. Outcome of planned home and planned hospital births in low risk pregnancies: prospective study in midwifery practices in the Netherlands. BMJ 1996;313: 1309–13.







Leave a Reply