The UK’s Confidential Enquiries into Maternal Deaths has been in existence for more than 50 years. In that time much has changed, but the learning process remains the same.
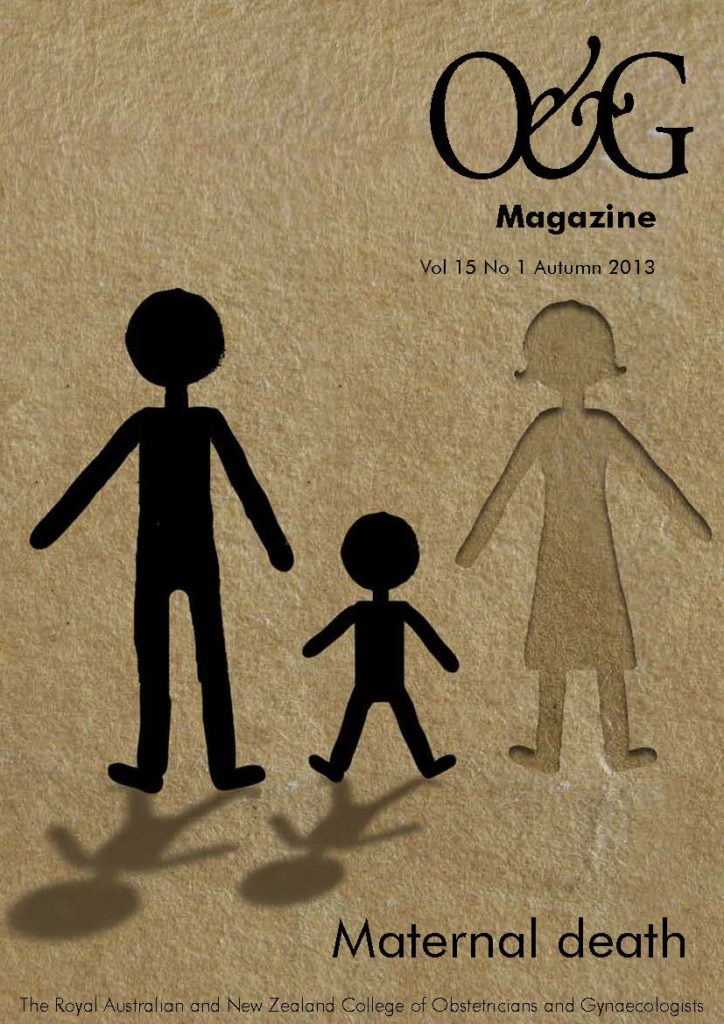
Death in pregnancy is rare in developed countries such as Australia and the UK, but it still happens. When it does, our reaction, after the first shock, is to investigate and try to prevent the same thing happening again. Learning lessons from tragedy, however, is no easy task. There is a natural tendency to look for scapegoats. Organisations are reluctant to find fault with their own systems. Individuals directly involved feel guilty and either reproach themselves needlessly or become over-defensive when facing official enquiries.
Having seen these reactions many times in various countries, I am full of admiration for the people who set up the UK’s Confidential Enquiries into Maternal Deaths (CEMD) in the early 1950s. They might easily have decided not to bother – maternal mortality had already fallen by three-quarters in 15 years, thanks to sulphonamide and penicillin eliminating puerperal sepsis – but instead of feeling complacent, that optimistic post-war generation wanted to tackle the remaining causes.
Their new initiative involved a national panel of obstetricians receiving detailed summaries of all maternal deaths across the country. The Ministry of Health published a report of their findings every three years, after which the papers on individual cases were destroyed. The published report contained no identifying details, so the staff involved could be completely frank about what had happened.
My generation of obstetricians grew up with this system, established in an era when government and doctors trusted each other. Confidentiality was never breached (though lawyers sometimes tried) and professionals knew their anonymous reports would be used to good effect. There was no extra pay for members of the national panel or for the Regional Assessors who organised local reporting: an invitation to do the job was a mark of respect from one’s colleagues and was reward enough.
The triennial reports became best-sellers in the Royal College of Obstetricians and Gynaecologists (RCOG) bookshop, not just because they were required reading for the MRCOG, but because they told the truth. Death is not an arbitrary outcome measure dreamed up by managers. It makes unpleasant reading, though, and during my 20 years as a Central Assessor there were times when I was moved to tears by first-hand accounts from midwives and doctors, anonymised by marker pen or correction fluid even before their reports reached me.
During those 20 years there were many changes, though not to the basics such as confidentiality. The number of specialties involved in the panel increased, finally including a psychiatrist and a family doctor as well as a pathologist and members from the acute hospital services. The arrival of midwives was important and prompted a handwritten letter from the ex-Chief Medical Officer who had set up the enquiry (and was now approaching his 100th birthday). He had wanted midwives on the original panel in 1952, but had been overruled. The midwives are now the UK CEMD’s strongest supporters.
The purpose has always been to learn lessons, as shown by the title of the most recent reports, ‘Saving Mothers’ Lives’. How do we do this? The process, now known as the ‘audit loop’, has five steps, the first being identification of cases. We have always insisted that every maternal death, from around the time of conception until well after delivery, must be reported. If you try to be selective you risk missing important messages, particularly about poor people. It can be hard work to find out about the deaths of socially excluded women outside hospital, and not all countries want to do so. Unfeasibly low maternal mortality rates look good in international comparisons, but you can be sure that they don’t include the deaths of migrants or even the indigent poor.
Step two is to gather information. We encourage those involved to tell us not only what happened, but also what lessons they have learned. Their thoughts can be insightful and may be quoted in the report. By contrast, the paperwork from a hospital’s own internal investigation, often sent to us in full nowadays, is rarely helpful. It is not that hospitals want to cover things up, but proper investigation of a maternal death needs experience of many similar events, which is now, thankfully, impossible for a single hospital to achieve. This is one reason why a national, or at least state-wide, enquiry is essential.
Step three of the audit loop is to analyse the results. Statistical help is needed, but the CEMD has always relied mainly on clinicians. Cases are grouped by cause – hypertensive disorders, sepsis, haemorrhage and so forth – and when each group is looked at patterns begin to emerge. You start to see who is at risk and what are the first signs of a life-threatening problem, and you can suggest what steps should be taken to avert disaster.
This pattern recognition is just like gaining clinical experience and teaches powerful lessons. Over the years we learned, for example, that the only symptom of ectopic pregnancy may be diarrhoea, fatally dismissed as a ‘tummy bug’. We discovered how often a woman with postpartum psychosis seems to be managing well until she kills herself in a chillingly violent way. Recently, we found that some ethnic groups, even when well integrated in the UK, still have persistently high maternal mortality rates.1
Step four is to formulate recommendations. In the past, readers were left to decide for themselves what action to take, but in recent years we have become more prescriptive. To my surprise, clinicians like being told what to do. Recommendations are now targeted at specific groups – clinicians, managers and politicians. Nobody can be forced to comply, but external pressure to do so comes when recommendations are incorporated into hospital protocols, RCOG guidelines and the National Health Service’s indemnity scheme.
Nevertheless, the final step – implementation – remains the most difficult. It requires a readership that pays attention to the report. Some specialties, such as obstetric anaesthesia, have a tradition of doing so, but others, such as emergency medicine, do not. Even for obstetricians and midwives, the sheer number of recommendations can be daunting, which is why we recently developed a ‘top ten’ list of recommendations that must be prioritised.
In the National Health Service, clinicians cannot improve the service without the co-operation of managers and pressure from politicians. Engaging the attention of these groups requires some flair, and publicity helps. The launch of each report is a media event, which needs careful handling. A well-informed public is fundamental to improving women’s health, but we don’t want to scare women with a litany of fatal cases.
The CEMD has had its detractors, particularly in the early days of evidence-based medicine, when the process was criticised for being based on expert opinion rather than on randomised controlled trials. There is, however, a symbiotic relationship between the CEMD, epidemiology and laboratory science. The reference list of many a research paper shows it was inspired by CEMD findings, and the CEMD’s recommendations are informed by the latest research. For example, in 1994, we drew attention to current research on hypertensive disorders2, and our next report3 endorsed treatment with magnesium sulphate, following a recent major RCT.4 With some life-threatening conditions, however, adequately powered trials are not possible and there is no alternative to expert opinion.
Is there evidence that the CEMD has succeeded in saving mothers’ lives? Without control groups blinded to the recommendations it is hard to be certain, but the timing of some improvements is highly suggestive. For example, from 1991 onwards thromboembolism was, by an increasing margin, the leading cause of direct maternal deaths in the UK. After the RCOG issued recommendations on thromboprophylaxis at caesarean section there was a sharp fall in deaths in this group, and the CEMD recommended extending the guideline to other women at risk. In 2004, the RCOG published a new thromboprophylaxis guideline that was followed by a statistically significant fall in deaths from thromboembolism.1
The fact remains, however, that despite its effectiveness and universal clinical support, the UK CEMD has been around for over half a century. Its longevity became an increasing irritant to a health service that likes to promote change, and in 2011 it sank into a bureaucratic quicksand and disappeared. Paradoxically, this happened just as many other countries, from South Africa to Kazakhstan5,6, were adopting and adapting the UK model. Fortunately, the UK Enquiry is re-emerging under the auspices of the National Perinatal Epidemiology Unit and there is good reason to hope that under new management the process of saving mothers’ lives will continue.7
References
- Centre for Maternal and Child Enquiries (CMACE). Saving Mothers’ Lives: reviewing maternal deaths to make motherhood safer: 2006–2008. The Eighth Report on Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG 2011; 118 Suppl 1: 1-203.
- Department of Health, Welsh Office, Scottish Office Home and Health Department, Department of Health and Social Security, Northern Ireland. Report on Confidential Enquiries into Maternal Deaths in the United Kingdom 1988–1990. London: HMSO, 1994.
- Department of Health, Welsh Office, Scottish Office Home and Health Department, Department of Health and Social Services, Northern Ireland. Report on Confidential Enquiries into Maternal Deaths in the United Kingdom 1991–1993. London: HMSO, 1996.
- The Eclampsia Trial Collaborative Group. Which anticonvulsant for women with eclampsia? Evidence from the Collaborative Eclampsia Trial. Lancet 1995:345:1455-63.
- National Committee on Confidential Enquiries into Maternal Deaths. Saving Mothers 2008–2010. Fifth Report on Confidential Enquiries into Maternal Deaths in South Africa. Pretoria: Department of Health, 2012.
- Central Committee on Confidential Audit (CCA). Saving Mothers’ Lives: Confidential Enquiries into Maternal Deaths in the Republic of Kazakhstan for 2009–2010. Astana: Ministry of Health, 2012.
- Knight M. How will the new Confidential Enquiries into Maternal and Infant Death in the UK operate? The work of MBRRACE-UK. The Obstetrician and Gynaecologist 2013:15:65.





Leave a Reply