Examination of cases of women who survived a severe complication of pregnancy, childbirth or the puerperium is increasingly being recognised as a potentially useful tool in assessing the quality of healthcare.
A maternal death is one of the most devastating complications in obstetrics, with wide-ranging implications for both the family and the staff involved. Thankfully, maternal mortality is now a rare event in Australia, which has one of the world’s lowest maternal mortality rate (MMR).1 Mortality rates in the developed world have plateaued over the last 40 years, while mortality rates in the developing world, though still high, have shown significant improvement over this time.2 The epidemiology of maternal deaths has also changed, particularly in the developed world, where indirect obstetric causes such as venous thromboembolism (VTE), psychiatric disease and cardiac disease have overtaken direct obstetric causes such as postpartum haemorrhage (PPH) and pre-eclampsia as primary causes of mortality. One of the many primary reasons for improvement in the maternal mortality rates has been an understanding of the aetiology of maternal deaths and a subsequent improvement in clinical care. Confidential enquiries into maternal deaths (CEMD) have, in this regard, been a valuable tool, providing a thorough evaluation of the quality of healthcare and recommending improvements.3
However, as the MMR has improved, reviews of maternal deaths, though useful, do not necessarily reflect the scope of complications in obstetric practice. Resource-rich countries, such as Australia, have a low MMR and to attain a large enough sample to identify trends in quality of maternal healthcare takes from three to ten years.3 This is reflected in the infrequent publications of the Australian Institute of Health and Welfare maternal mortality statistics. Furthermore, the circumstances related to a maternal death in a developed country are often very particular to the individual case and the value of this information for general use might be limited. This is certainly the case in many developed countries where maternal deaths tend to be the result of rare complications and an indication of the complexity and unpredictability of the condition, for example, amniotic fluid embolism or complex cardiac disease. In countries where maternal deaths are relatively frequent, CEMD give a better indication of problems in the health system, provided most deaths occur within health institutions. However, in resource-poor settings the vast majority of deliveries are still undertaken in the ‘home’ setting, thus creating difficulties with collection of data. Additionally, maternal deaths per institution in these countries are still uncommon, even in countries with a high MMR. Therefore, the relevance of such deaths to small district units may not highlight local issues and processes that require examination.
Table 1. The proposed WHO near-miss criteria
| Clinical criteria | |
|---|---|
| Acute cyanosis | Loss of consciousness lasting >12 hours |
| Gasping | Loss of consciousness and absence of pulse/heart beat |
| Respiratory rate> 40 or <6/min | Stroke |
| Shock | Uncontrolled fit/total paralysis |
| Oliguria | Jaundice in the presence of pre-eclampsia |
| Clotting failure | |
| Laboratory-based criteria | |
| Oxygen sats < 50% for >60 mins | Ph <7.1 |
| PaO2/FiO2 < 200mmHg | Lactate > 5 |
| Creatinine > 300µmol/l or >3.5mg/dl | Acute thrombocytopenia (< 50000 platelets) |
| Bilirubin > 100µmol/l or > 6.0 mg/dl | Loss of consciousness and the presence of glucose and ketoacids in urine |
| Management-based criteria | |
| Use of continuous vasoactive drugs | Intubation and ventilation for > 60 mins not related to anesthesia |
| Hysterectomy following infection or haemorrhage | Dialysis for acute renal failure |
| Transfusion > 5 U of red cell transfusion | Requiring CPR |
Say L, Souza, JP, Pattinson RC. Maternal near miss – towards a standard tool for monitoring quality of maternal health care. Best Practice and Research Clinical Obstetrics and Gynaecology. 23 (2009) 287-296.
Review of cases of maternal near miss has the potential to highlight both deficiencies and positive elements in the provision of obstetric services and to provide information about the epidemiology of severe obstetric complications.4 This is analogous to the review of neonatal near misses that highlights the potential for improvements in intrapartum care.5 Furthermore, as a result of their near-death experience and often complicated recoveries, near misses do have significant psychological and physical morbidity, as well as issues related to resource utilisation that need to be continually addressed to attain the best clinical outcomes. Auditing near misses ensures we do not forget those lessons from our past that have resulted in the dramatic reductions in maternal mortality.3
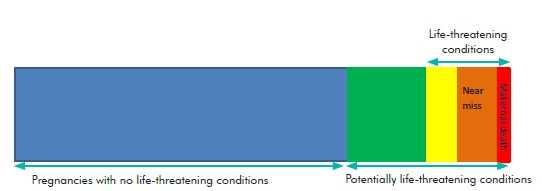
Figure 1. Classification of pregnancies at CBH.
The concept of maternal near miss is not a new one with it known by various names, such as severe acute maternal morbidity (SAMM), over the last 20 years. In recent years, a considerable body of research has focused on the analysis of maternal near miss with a view to understanding health system failures in relation to obstetric care.6 Some clinicians argue that the auditing of cases of severe adverse maternal events already occurs within institutions, with root cause analysis (RCA), and at a national level, with the Australasian Maternity Outcomes Surveillance System (AMOSS). While mechanisms exist within most hospitals for the reporting of severe adverse events and for the performance of RCAs, these are designed to identify deficiencies within the hospital system or in the provision of care and thus do not incorporate suitable mechanisms for the detection of all individual cases of maternal near miss.4 The AMOSS is now established in hospitals across Australia with the aims of improving knowledge of rare obstetric disorders and their management in Australia, and translating research findings into policy, clinical guidelines and educational resources for clinicians. However, AMOSS has been developed to deal with national trends and rare events and not audit data in individual units or area health services.4
Despite the collection of data, assessment of obstetric morbidity has been hampered by the various criteria used to define a maternal near miss. What had been lacking is a standardised definition of a near miss, with criteria that can be applied in a systematic and consistent manner allowing a standardised comparison between units and within obstetric units over time. A WHO working party addressed this issue in 20096 and came up with a number of parameters for inclusion as a near miss (see Table 1).
The use of these broad categorisations in defining near miss has limitations and advantages, but what the categorisations encompass is a set of criteria that are consistent, validated and can be applied in both resource-rich and resource-poor settings.
A study at the Cairns Base Hospital (CBH), in Far North Queensland (FNQ), that began in 2009, was the first in Australia to incorporate the newly developed WHO criteria. At CBH we were concerned with adapting this tool to assess our own obstetric performance in the region. Collecting near miss data involved identifying those pregnancies that may be at risk, such as ruptured ectopic pregnancies or HELLP syndrome, and then further refining the process using the WHO criteria proposed to identify those cases that are true near misses (see Figure 1).
In identifying pregnancies that may be at risk, a combination of clinical and management-based criteria from the WHO working party were incorporated (see Table 2).
Table 2. CBH criteria for potential cases of obstetric near misses
| Any APH requiring delivery for maternal reasons | Any admission to ICU |
| Any PPH requiring operative interventions | Severe pre-eclampsia complicated by HELLP, renal failure or other major morbidity |
| Any postnatal cases that returned to OT | Any pulmonary embolus |
| Any ruptured ectopic pregnancy | Any patient experiencing severe shock or collapse |
| Any condition that required immediate medical assessment |
Over the 12 months of the study, we found 58 cases considered by staff to fulfil the criteria outlined in Table 1. Of those cases, 18 were subsequently classified as not potentially life threatening and as responding promptly to care; 40 were considered to fall in the category of having potentially life-threatening conditions; of these 17 met one or more of the WHO criteria for having life-threatening conditions and were classified as true near misses (see Figure 2).
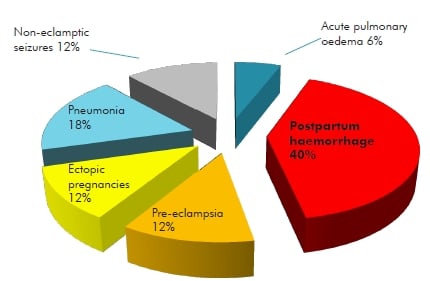
Figure 2. Obstetric near misses at CBH
The most common cause of a maternal near miss was PPH followed by pre-eclampsia and VTE. These conditions previously often resulted in death, but with improved management have become rare causes of maternal mortality in the developed world. Non-obstetric near misses accounted for a significant number of cases, reflecting the high level of comorbidity in FNQ. Additionally, Indigenous women were over represented in our data. The significant utilisation of resources by cases of near miss is also highlighted with the cost of admission being five- to ten-fold greater than an uncomplicated delivery (see Figure 3).
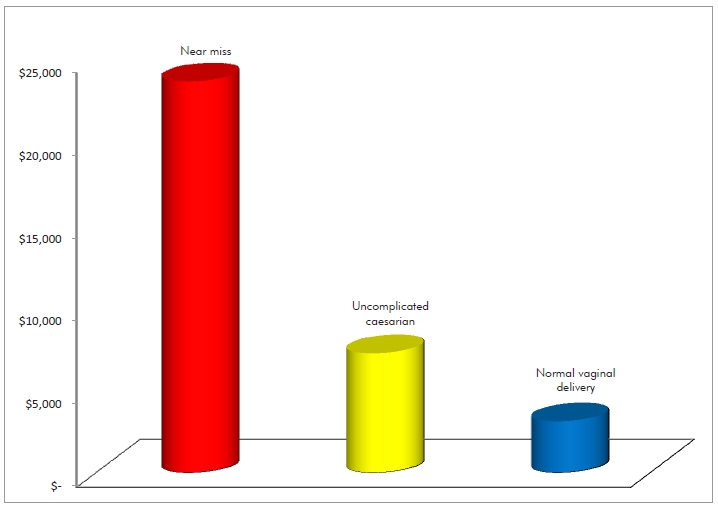
,Figure 3. Cost of admission at CBH (comparison of near miss with uncomplicated delivery). Cost of admission was calculated by duration of stay in hospital, but did not incorporate other miscellaneous expenses such as use of blood products/factor 7 that would have significant increased the costs of cases of near miss.
The results indicate the continued significant morbidity of these conditions as well as the need for ongoing training and simulation sessions for obstetric staff in the recognition and management of severe obstetric morbidity. It also highlights the significant resource allocation that is required in the management of near misses and the continued need to be alert to the presence of possible obstetric complications.
In summary, while review of maternal deaths and identification of avoidable contributing factors will undoubtedly continue to occur both nationally and in individual hospitals, incorporation of analysis of maternal near miss in assessing the process of obstetric care will be a valuable contribution in taking necessary action to improve the quality of care. The addition of near-miss audits will allow the care of critically ill women to be analysed, deficiencies in the provision of care to be identified and comparison within and between institutions and countries to be carried out over time. This will, ultimately, improve the quality of obstetric care and further reduce maternal morbidity and mortality.
References
- AIHW media release – Maternal death low in Australia (Fri 2nd May 2008). (Accessed 19 February 2013). Available from URL:http://wwwaihw.gov.au/mediacentre/2008/mr20080502.cfm.
- WHO media release – Maternal Mortality fact sheet May 2012
(accessed 21 February 2013) Available on URL: http://www.who.int/mediacentre/factsheets/fs348/en/index.html. - Pattinson R, Near Miss audit in Obstetrics. Best Practice and Research in Obstetrics and Gynaecology. (23) 2009 285-286.
- Jayaratnam, S. de Costa C, Howat P. Developing an assessment tool for maternal morbidity near miss – A prospective study in a large regional hospital. Australian and New Zealand Journal of Obstetrics and
Gynaecology. 2011 51: 421-425. - Avenant, T. Neonatal near miss: a measure of the quality of obstetric care. Best Practice and Research Clinical Obstetrics and Gynaecology 23 (2009) 369-374.
- Say L, Souza, JP, Pattinson RC. Maternal near miss – towards a standard tool for monitoring quality of maternal health care. Best Practice and Research Clinical Obstetrics and Gynaecology. 23 (2009) 287-296.





Leave a Reply