The practical applications of pathology in cases of perinatal death or termination of pregnancy for fetal anomolies.
The death of a baby or termination of pregnancy for fetal anomalies is a difficult time for many families. In this situation, pathology provides important information for the family, clinical team and even the wider community. However, not all clinicians are familiar with the perinatal pathology system. These are some of my comments and observations, after several years working in perinatal pathology.
Legalities and preliminaries
One of the first things that we tell our pathology trainees, on hearing about an autopsy, is to check the paperwork – consent, perinatal death certificate and clinical notes. Although this sounds fairly routine, there are unexpected traps for the less experienced. For example, signed consent is not legally required for fetuses less than 20 weeks gestation. However, many pathology laboratories request signed consent for fetal autopsies at any gestational age. In some laboratories, this will also need to be signed by a ‘designated officer’ of the hospital. Each hospital has its list of designated officers, usually from medical or nursing administration. An error that sometimes occurs is for the doctor seeking consent to sign as the designated officer.
Sometimes parents are unable to consent to a full autopsy, but agree to a partial autopsy. Partial autopsies, postmortem imaging or multiple needle biopsies do not provide the same information as full autopsies and prior discussion with the perinatal pathologist is helpful to clarify their likely limitations and usefulness. Specific consent may be required for dissection of organs/tissues not included in the standard autopsy procedure; for example, removal of limb bones in cases of skeletal dysplasia. Consent forms and information about autopsy consent and procedures can be obtained from perinatal pathology laboratories. A perinatal death certificate is required for fetuses of 20 weeks gestation or older. If these documents are not provided, the autopsy will be delayed until they are received. As degenerative changes occur after death, delay of the autopsy examination may limit its usefulness.
Lack of adequate clinical information can be another cause of delay; the clinical notes of both mother and infant are required. Scan reports, laboratory test results, discharge or clinical summaries and birth summaries can supply much information and copies of these should accompany the consent form. Phone discussions with the pathologist prior to the autopsy are often helpful. Some of the clinicians in our institution also send emails prior to the deliveries, giving brief details about impending autopsy cases. This is much appreciated by pathologists, as it gives an opportunity to plan ahead and also allows time for discussion about any special tests or procedures that may be required; for example, muscle biopsies or metabolic tests, which must be collected as soon as possible after death (preferably within two hours).
Scope of pathological findings
The autopsy and placental examinations often provide information to guide management of future pregnancies. The autopsy findings may suggest the sequence of events that led to fetal death, give information about fetal nutrition and growth, complications of medical care, occurrence of trauma, haemorrhage and infection. The degree of maceration in a stillborn infant may suggest an approximate time of fetal death in utero, but many factors affect the changes that occur after death, so that an exact time of death cannot be given. Congenital anomalies can be documented, some of which are associated with a familial or recurrence risk. This is helpful for counselling for later pregnancies. Negative findings are also important in this context. However, in about a third of cases, careful examination of the placenta and fetus at autopsy fails to reveal a specific cause of death, especially for fetal demise after 35 weeks gestation.1 Fetal autopsies provide an audit for clinical policies and practices and information for regional and national statistics. Research opportunities should not be overlooked.
Procedures
Clinical photographs, babygram X-rays, external examination and measurements are done before opening the body cavities. In some cases, tissue is removed for genetic studies and stored, so that material will be available for genetic testing if required in the future. It is preferable to send the fetus fresh (not in formalin), as dissection is easier and material can be obtained for microbiology, genetic studies or other ancillary tests as required. The standard autopsy procedure involves opening the thoracic and abdominal cavities and head. The incisions are placed so that they will be covered when the baby is clothed, if the parents wish to view the baby later. The body structures and organs are examined and the major organs weighed. Fetal weights and measurements are compared to normal values obtained from standard biometric charts, such as those published by Phillips et al.2 The organs are replaced and the body is reconstructed after the examination is completed and samples have been removed for further tests. The brain is soft and pathological examination is very limited if cut in the fresh state. The pathologist may therefore wish to retain the brain for fixation for a few days, before examination and dissection, after which the brain can be replaced in the body. This may delay completion of the autopsy for one or more days, but can be discussed with the pathologist before the autopsy.
Autopsy reports
Some laboratories issue a preliminary autopsy report within one to seven days of the autopsy, listing the macroscopic findings. The final autopsy reports often include other ancillary tests, such as genetic screening tests, radiology, microbiology results and clinico-pathological correlations, and are not usually available for one or two months.
Placental examination
Indications for placental examination
The placenta gives an indication of what happened during pregnancy. The placenta can provide information needed for early neonatal care, reproductive planning, risk assessment for infant neurological outcome and medico-legal issues.
For practical reasons, not all placentas can be examined. Indications for placental examination include maternal issues (pre-existing disease, infection/fever, gestational hypertension, haemorrhage, biophysical or biochemical monitoring abnormalities); fetal/newborn issues (intrauterine fetal demise or growth restriction, hydrops, prematurity, congenital anomalies, suspected infection, haematological abnormalities); or gross placental abnormalities. This information should be included in the placental request form.
Pathological examination of the placenta
Pathological examination of the placenta is essential in the investigation of stillbirths. One study found that the cause of fetal death could be explained by placental examination alone – without autopsy – in 48.1 per cent of cases, while 69.2 per cent of cases showed placental changes that could explain fetal/infant death and only 16.3 per cent of deaths could be explained by autopsy alone.3
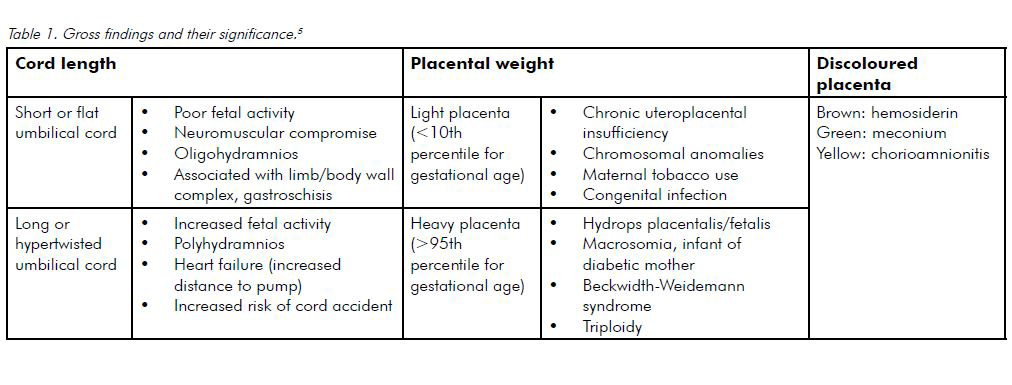
Gross examination of the placenta may suggest clinical correlates (see Table 1). Gestational age should always be stated on the pathology request form so the pathologist can correlate this with measurements, including placental weight and microscopic findings such as villous morphology. Details of labour are also useful for clinicopathological correlation. For example, histological subchorionitis (acute inflammatory cells in the fibrin layer beneath the chorionic plate) evolves within hours following membrane rupture, which may occur when membrane rupture precedes delivery by six or more hours, even in the absence of clinical chorioamnionitis.4 Much clinical information is present in the birth summary and it is useful to attach this to the placental request form. If special studies are needed, for example, injection of fetal vessels for assessment of vascular anastomoses in monochorionic twin placentas, this should be discussed with the pathologist before sending the specimen.
Placental pathology report
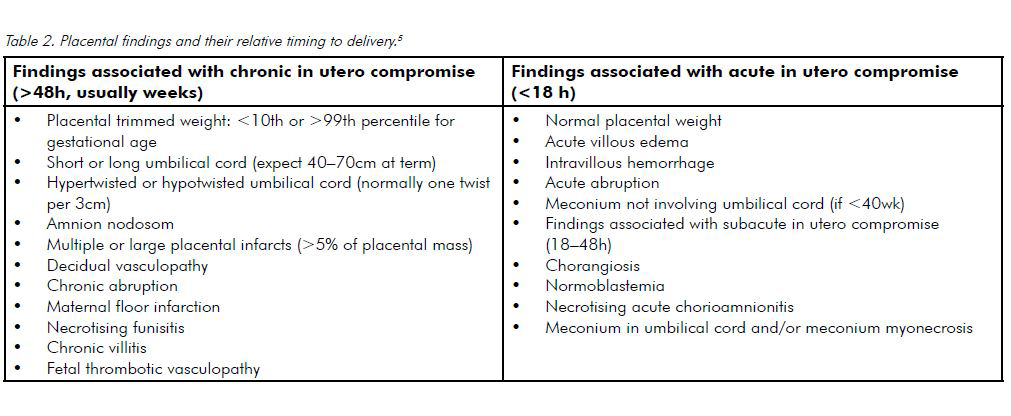
The placental report often indicates the presence and severity of the lesions and risk of recurrence. Schemata exist for specific lesions, for instance, the duration (stage) and intensity (grade) of both maternal and fetal inflammatory responses in cases of acute chorioamnionitis. Studies have found an association between some placental abnormalities and fetal neurological compromise, such as diffuse severe acute villous oedema and cerebral palsy and marked chorionic plate vasculitis and other forms of neurological compromise.5 The significance of some findings such as umbilical cord coiling may not be fully understood6, but such findings are still included in pathology reports, as currently available studies suggest they are probably significant and further studies may indicate their full relevance. Placental findings may have medicolegal implications, for example, the presence of chronic placental abnormalities (such as infarcts or maternal decidual vasculopathy) suggest that fetal damage occurred antenatally rather than perinatally (see Table 2) and also document possible predisposing factors for poor fetal outcome.
Postscript
The best outcomes in perinatal pathology can be achieved only if there is coordination and cooperation between pathology and clinical teams. Good communication and organisation are essential for this.
References
- Craven C and Ward K: Stillbirth: Tissue findings with environmental and genetic links. Seminars in Perinatology, 2002; 26: 36-41.
- Phillips JB, Billson VR and Forbes AB: Autopsy standards for fetal lengths and fetal weights of an Australian perinatal population.
Pathology 2009; 41: 515-526. - Tellefsen CH and Vogt C: How important is placental examination in cases of perinatal death. Ped Dev Pathol 2011; 14: 99-104.
- Boyd TK and Redline RW: Pathology of the placenta. In Gilbert-Barness E (ed): Potter’s Pathology of the Fetus, Infant and Child, second edition. China: Mosby Elsevier. 2007, pages 645-693.
- Roberts DJ: Placental pathology, a survival guide. Arch Pathol Lab Med 2008: 132: 641-651.
- Khong TY: Evidence – based pathology: umbilical cord coiling. Pathology 2010; 42: 618-622.






Leave a Reply