Uterine torsion is a rare obstetric complication that is almost always identified perioperatively. Clinicians should consider it as a differential diagnosis in the presence of uterine malformation or the presence of fibroids.
Uterine torsion is an uncommon obstetric finding and is considered to be pathological at greater than 45 degrees rotation along the long axis. There are relatively few documented cases of levorotation of the uterus. Contributing factors such as maternal trauma, fetal malpresentation, ovarian tumours and uterine abnormalities are recurringly identified. A recent incident of uterine torsion was identified intraoperatively in an outlying metropolitan hospital, which is discussed below.
A 29-year-old patient had been seen throughout her pregnancy without any major concerns until she was admitted for an induction at six days post-term, after being identified as having an unstable fetal lie.
Her obstetric history included three previous pregnancies – all resulting in vaginal deliveries – that had been induced for gestational hypertension between 38 and 39 weeks gestation each time. Her current pregnancy had not been complicated by gestational hypertension or any other specific concerns, despite having the same partner. On review of her handheld record it was noted that fetal lie had continued to alternate between antenatal visits.
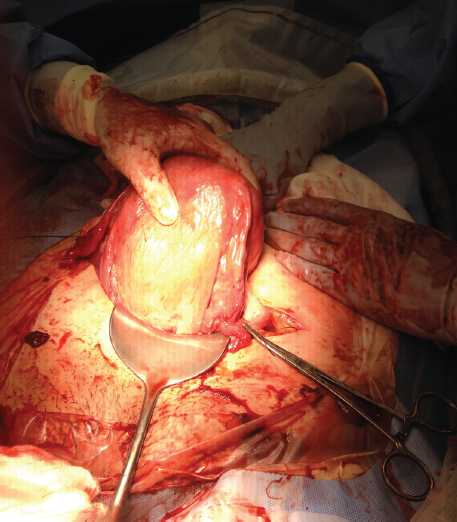
Anterior surface after detorsion.
On the eve of induction the baby was noted to be cephalic with head at station -3. Overnight, palpation showed baby to be transverse, but by morning baby was cephalic again. The patient was fully informed of the risk of cord prolapse and need for emergency caesarean section, and the decision was made to proceed with induction in business hours to minimise risks. Following a reassuring cardiotocograph (CTG), an artificial rupture of membranes was attempted by the birth suite registrar. The vaginal examination was noted to be particularly difficult, with the registrar unable to palpate through the internal os. The consultant on call was asked to attend and review. The consultant confirmed the fetus was cephalic with a bedside ultrasound and with the assistance of fundal pressure; rupture of membranes was performed with a fetal scalp electrode. This was a very technically difficult procedure with the head noted to be at station -4 and at times impossible to feel at all vaginally. The cervix was noted to be 2cm long and quite firm.
The fetus continued to be very active during this process. After descent of fetal head with draining of liquor, and with the reassurance of an exemplary CTG, the decision was made to start syntocinon and proceed with the induction as per protocol with repeat vaginal examination in two hours or as indicated.
After 40 minutes, the birth suite registrar was asked to attend to review an abdominal palpation after a particularly vigorous bout of fetal movement. It was felt that the baby was now transverse, which was confirmed by the registrar on bedside ultrasound. A vaginal examination was performed and no cord or fetal parts were palpated; again the registrar was unable to palpate through the internal os, which was again noted to be particularly tight given the parity and gestation.
An emergency caesarean section was called, for the now-significant risk of cord prolapse. In the operating theatre, a spinal anaesthetic was placed and pfennensteil entry commenced. At the uterus, the fallopian tube, ovary and engorged pampiniform plexus were noted to be overlying the uterus diagonally from the right iliac fossa to the left fundal surface, continuing posteriorly. This was thought to be the left tube with acute dextorotation so was accordingly semi-corrected with difficulty. At examination of the exposed uterine surface, the lower segment was poorly formed and the bladder was unidentifiable. Ongoing fetal movement throughout the entry resulted in the fetal head being oblique at the time of transverse uterine incision. The fetus was manipulated internally, as it remained very active, and was delivered cephalic. The placenta was delivered without incident.
At uterine closure, the anatomy was noted to continue to be unusual. The uterus was exteriorised and it became obvious that the uterus was levorotated to 270 degrees and the uterine incision had been made on the posterior aspect of the uterus. The incision was closed in double layers and the uterus was rotated back 270 degrees on the cervix to normalise anatomy. The uterus appeared to be fully perfused with no evidence of necrosis. The mother and baby both recovered well.
Discussion
Uterine torsion is rare and reported only as case studies.Some degree of uterine rotation is quite normal in term pregnancies, but rotation greater than 45 degrees is considered pathological.2 The case studies available since the first reported case in 1876, describe torsion between 60 to 720 degrees with outcomes ranging from live, well mother and baby to peripartum hysterectomy and fetal demise and maternal death. Torsion is clockwise in two-thirds of cases. It is associated with malpresentation of the fetus, maternal trauma and, in a third of cases, uterine tumour or mobile uterine fibroid during pregnancy.
Prolonged torsion results in constriction of the uterine vessels to ultimately include uterine artery occlusion. As obstructed outflow increases pressure within the placental cotyledons, fetal distress becomes apparent and the risk of placental abruption significantly increases. Necrosis of the uterus has also been identified in several case studies. Uterine torsion is rarely diagnosed prior to emergency caesarean section.3 It was originally theorised that torsion only occurred in the presence of uterine tumours: ‘no tumour, no torsion’. Over time this understanding has been modified to include uterine abnormality until now when it is understood that most cases occur in normal anatomy, though causative factors are identified as repeat offenders in case reports. These include uterine myomata (31.8 per cent), congenital uterine abnormalities, mostly bicornuate uteruses (14.9 per cent), pelvic adhesions (8.4 per cent), ovarian cysts (seven per cent) and fetal malpresentation (two per cent). Single cases of external cephalic version and maternal trauma have been reported as causative factors.3
There are 212 documented cases in literature to date, the first of which was reported in 1876.4 Differential diagnosis is usually obstructed labour, placental abruption, uterine rupture or fibroid degeneration as symptoms include intense colicky abdominal pain that progresses to severe generalised abdominal pain and is associated with eventual fetal compromise. Vaginal bleeding, urinary or bowel disturbances are also regularly described, along with fetal arrhythmias in cases with prolonged torsion. Symptoms usually present unexpectedly and acutely in labour and occasionally, antenatally. Cases have been identified in all age groups, and at all gestations, but most occur in the third trimester.2,4
Torsion is almost always misdiagnosed and then identified unexpectedly at emergency caesarean section, but can be identified antentally. An example of antenatal diagnosis was described by Wilson et al when an abnormal vaginal examination prompted an MRI, which identified torsion by demonstrating an ‘X’ shaped shadowing at the level of the vagina where a ‘H’ shaped shadowing would normally be seen.2,4 However, MRI diagnosis has also been documented to fail to identify torsion in a case where the images were not taken specifically at the level of the vagina, as symptoms indicated an acute abdomen, and therefore failed to identify the tell-tale ‘X’.3 Ultrasound has also been used to identify a change in position of a previously documented uterine fibroid or placenta as a diagnostic tool.6 Presentation is generally acute with severe abdominal pain and signs of pregnancy compromise in the third trimester, so an MRI or ultrasound may not the most appropriate diagnostic tool.
Once symptoms are identified and a differential diagnosis made, pregnancies at, or close to, term are delivered by emergency caesarean section.
If diagnosed in the second trimester of the pregnancy, laparoscopic reversal of the torsion can be attempted, though is associated with significant risk to the pregnancy, with 13 per cent perinatal mortality.3 Some sources recommend plication of the round or uterosacral ligaments to prevent repeat torsion of the gravid uterus.7,8 Closer to term, or at term, delivery by caesarean section can be undertaken, usually with minimal risk, though in the presence of necrosis, hysterectomy may be recommended. Depending on the degree and duration of torsion, anatomy can be grossly distorted and oedematous, making identification of landmark structures difficult. The lower segment and bladder may not be identifiable at all increasing risk of maternal injury.4 In many cases, torsion is not recognised, or is too difficult to reverse prior to delivery; however, the position of the uterus should be deliniated as much as possible prior to uterine incision and the bladder reflected if possible to avoid damage to uterine arteries, ligaments, tubes and uterine vessels. Caesarean delivery through the lower posterior surface of the uterus has been reported in a number of cases5,9 as occurred in the above case.

Posterior surface after detorsion.
Across all reported cases, maternal mortality is 13–18 per cent.4 Further advanced pregnancies have higher mortality, with 18.5 per cent at term, though this number is skewed by the majority of cases reported being in the third trimester. Rotations of higher than 180 degrees are associated with a mortality rate of 50 per cent. There have been no reported cases of lovorotation greater than 270 degrees since 1985.
Since 1976, 12 per cent of cases report fetal demise and no cases report maternal demise.4 The outcomes are not always congruent with the degree of torsion or the severity of the symptoms, with 11 per cent of documented cases being asymptomatic, as in this case.4 Most reported cases have a positive outcome for both mother and baby; however, before 1976, there are reported cases of maternal death and two cases of peripartum hysterectomy for ascending necrosis secondary to torsion.
In the case presented at the beginning of this article, both patients remained asymptomatic throughout. The emergency caesarean section was performed for the high risk of cord prolapse not for a suspected torsion of the uterus. Given the urgency of the delivery, diagnosis was not made until exteriorisation of the uterus following delivery. As discussed, it was only upon more detailed examination of the exposed uterus that the engorged left fallopian tube and paminiform plexus were identified as the structures diagonally crossing the uterus and the oedematous bladder was noted deep in the pouch of Douglas on the rotated anterior surface of the uterus.
The risks of recurrent torsion are unknown and recommendations for future pregnancies vary, so it was recommended to the mother that clinically she could attempt a vaginal birth; however, an elective caesarean section was appropriate and should certainly be seriously considered should there be a failure of the fetal head to appropriately engage in a future pregnancy.
References
- Piot, Gluck and Oxorn. Torsion of the Gravid uterus. CMA Journal.1973;vol109:1010-1011.
- Wilson, Mahalingham, Ross. Third Trimester Uterine Torsion: Case Report. JOGC 2006.
- Gururaj Deshpande, Rajesh Kaul, and Manjuladevi P. Department of Obstetrics and Gynecology, Kamineni Institute of Medical Sciences, Nalgonda District, Andhra Pradesh State, Narketpally 508254, India.
- Jensen, JG, Uterine torsion in pregnancy Acta Obstet Gynecol Scand. 1992 May;71(4):260-5.
- Gule P, Adjobi R, Nguessan E, et al. Uterine torsion with maternal death: our experience and literature review. Clinical and Experimental Obstetrics and Gynecology. 2005;32(4):245–246.
- Pelosi MA, III, Pelosi MA. Managing extreme uterine torsion at term: a case report. Journal of Reproductive Medicine for the Obstetrician and Gynecologist. 1998;43(2):153–157.
- Mustafa MS, Shakeel F, Sporrong B. Extreme torsion of the pregnant uterus. Australian and New Zealand Journal of Obstetrics and
Gynaecology. 1999;39(3):360–363.
Further reading
Albayrak M1, Benian A, Ozdemir I, Demiraran Y, Guralp Deliberate posterior low transverse incision at cesarean section of a gravid uterus
in 180 degrees of torsion: a case report O.J Reprod Med. 2011 Mar-Apr;56(3-4):181-3.
De Ioris A1, Pezzuto C, Nardelli GB, Modena AB. Caesarean delivery through deliberate posterior hysterotomy in irreducible uterine torsion: case report Acta Biomed. 2010 Sep;81(2):141-3.





Leave a Reply