Over the past four decades the scope and availability of interventional radiology has increased remarkably, offering many new services to patients across many disciplines, including obstetrics and gynaecology.
It was more than half a century ago when Dr Charles Dotter, the ‘father of interventional radiology’, conceived concepts of percutaneous angioplasty and vascular stent placement, successfully dilating the superficial femoral artery of a woman with severe vascular disease who refused to have an amputation for an ischaemic foot. Dotter was subsequently nominated for the Nobel Prize in medicine for his pioneering work. In the decades that have followed, percutaneous interventional techniques have revolutionised many areas of medicine and are now routinely employed to selectively ablate tumours, manage stroke and myocardial infarction, lyse thromboses in many parts of the body, and arrest haemorrhage. These interventional radiology (IR) tools now have an important role in many areas of obstetrics and gynaecology.
Placenta accreta
The incidence of placenta accreta is increasing and management of delivery in the presence of morbidly adherent placentation is associated with a high risk of massive haemorrhage and hysterectomy. There is an emerging consensus that endovascular techniques have a major role to play in this setting. About 15 years ago, Dubois’ group described pre-operative placement of non-inflated balloon catheters in the hypogastric arteries. Following delivery, and before the hysterectomy, the balloons could be inflated to minimise pelvic haemorrhage. At the completion of the procedure, the balloons were deflated and, if there was ongoing bleeding, embolisation of the pelvic arteries could be performed. Variations on this theme include performing caesarean section leaving the placenta in situ and embolisation of the placental bed, thus preserving the uterus. There is no consensus on the correct technique, but use of interventional radiology allows considerable scope to tailor the management in the individual case. Overall, the use of balloon catheters is associated with good outcomes for mother and baby, with a low incidence of complications. There have been reports of iliac vessel thrombosis, but these have resolved with conservative management.

Figure 1. Angiogram in preparation for balloon placement pre-delivery.
Postpartum haemorrhage
Like placenta accreta, postpartum haemorrhage (PPH) is increasing in incidence for reasons that are not clear. However, PPH has the potential to be very serious and is one of the common causes of quite severe morbidity or maternal mortality. Multiple approaches can be used to manage PPH and interventional techniques may have a significant role in major obstetric haemorrhage and can be lifesaving. Although hysterectomy is an important part of the management of massive haemorrhage, this is obviously a sterilisation. In some cases, embolisation of bleeding vessels can allow for preservation of the uterus and possibly fertility.
Arterial embolisation is often considered after other conservative treatments, such as use of uterotonics, encirclement sutures and balloon tamponade, have been unsuccessful. Use of uterine artery embolisation has been described for at least two decades and was adopted from pre-existing management strategies for controlling haemorrhage in pelvic trauma and tumours. Typically, the interventional radiologist will sequentially and selectively catheterise the internal iliac arteries and uterine arteries. In situations of heavy bleeding, it is common to find multiple points of extravasation in the placental bed. Embolisation of the whole vascular territory is effective management in the majority of cases.
From a technical standpoint, there is often upward displacement of the arteries caused by the large uterus, markedly altering the anatomy from the non-pregnant state. A number of embolic materials can be used, but gelatine sponge is very commonly employed because of its (usually) temporary effect potentially increasing the safety of future pregnancies. Synthetic particles, such as polyvinyl alcohol (PVA) and other material may be employed, but there is some debated concern that the more permanent materials may prejudice future pregnancies.
Pelvic vascular ‘congestion’
Women are commonly referred to interventional radiologists for management of so-called pelvic congestion. This is a condition that is usually characterised by long-standing pelvic pain that is not cyclic. Imaging with ultrasound and computed tomography (CT) or magnetic resonance imaging (MRI) typically reveals pelvic venous distension associated with venous valvular insufficiency. Patients are typically in their 30s or 40s and present with low back and pelvic pain often described as ‘heaviness’, experienced in the lower pelvis, vulva and sometimes thighs. The symptoms may be worse with prolonged standing or physical effort and straining. Occasionally, the pain is associated with intercourse or is worse following sexual activity.
Pelvic vascular congestion results from incompetent valves in the ovarian veins and this may be affected by hormonal vasomotor effects. The condition is more common in parous women, probably because of the chronic venous distension of pregnancy renders valves in the ovarian veins incompetent. The valvular incompetence allows retrograde flow in the pelvic veins and, over time, causes development of varicosities. Imaging reveals tortuous pelvic veins of wide diameter (greater than 5mm) often with collateral flow, and there is often evidence of retrograde flow with Valsalva. There is often associated pelvic floor venous incompetence and a history of vulval and inner-thigh varicosities and/or recurrent leg varicosities is common.

Figure 2. Balloon in uterine artery test inflation pre delivery.
The use of pelvic vein embolisation is a very effect and minimally invasive treatment for pelvic venous congestion. The left ovarian vein is incompetent most commonly, but occasionally both gonadal veins are involved. The procedure involves catheterisation of the affected gonadal vein down to the level of the uterus and occluding the full length of the vein and any parallel channels with fibred metal MRI compatible coils and foamed sclerosant. Venous access from the common femoral or the jugular vein allows both diagnosis and treatment. Complications of the procedure are relatively rare and include non-target embolisation (for example, losing a coil to the pulmonary circulation), vein perforation, thrombophlebitis in the veins, and recurrence of the varices.
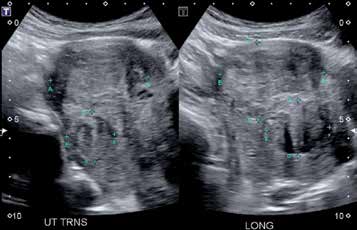
Figure 3. Ultrasound of fibroids.
Embolisation of fibroids
Benign leiomyomas, or fibroids, are very common and a uterine artery embolisation (UAE) has been shown to have a role in management. The advantages of UAE are reduced morbidity, compared to surgical treatments, and more rapid recovery. The technique is particularly useful for women unwilling to undergo surgery, or those who have co-morbidities that place them at particular risk for operative complications.
While fibroids are common peri- and postmenopausally, younger premenopausal women commonly develop fibroids. The technique was initially developed as a preoperative adjunct before planned myomectomy, to reduce intraoperative blood loss. However, many patients had such a good result from the UAE along that the surgery was no longer necessary. MRI provides a good method of selecting women likely to have a good result from embolisation treatment. A strong response on T2-weighted MR images predicts a good response to embolisation, whereas fibroids with a pre-existing poor blood supply and incipient necrosis show prominently on T1-weighted MR images and are likely to respond poorly to embolisation as their vascular supply is compromised already.

Figure 4. Angiogram showing left ovarian vein (LOV) reflux.
In a small proportion of women, the fundal portion of the uterus receives its blood supply from the ovarian vessels. The reverse is true too, and a small proportion of women will derive their ovarian blood supply from the uterine artery and not the ovarian artery. These are important considerations when considering UAE as a treatment for fibroids. The ideal patient for UAE is a premenopausal woman with menorrhagia, and it is important to rule out other conditions associated with heavy bleeding such as endometrial polyps, hyperplasia or carcinoma, and leiomyosarcoma. The effect of UAE on fertility and the course of subsequent pregnancy is not well-established, so women who wish to preserve fertility need to be very carefully counselled. The risk of the procedure inducing menopause is low, but this is an important potential complication and needs to be discussed.
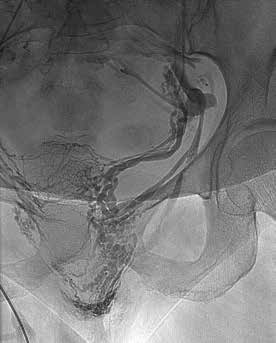
Figure 5. Reflux down LOV into peri-uterine plexus into vulva (varicose veins).
There is extensive collateral flow within the myometrium and, for this reason, bilateral UAE is usually required to achieve fibroid infarction – the aim being to use the higher metabolic rate of fibroids relative to uterine muscle to result into infarction of the fibroids alone. Bilateral uterine artery catheterisation is usually achieved using a single right femoral vein approach and a size 4 or 5 French gauge catheter. Owing to the potential for arterial spasm, microcatheters are usually used to access the uterine arteries. Embolic materials must be large enough to allow small vessel collateralisation from cervical and other branches to preserve the uterine muscle and embolisation must be complete enough to deprive the fibroids of oxygen and cause infarction. PVA particles and Gelfoam were typically used when UAE was first described, but newer hydrophilic particles that reduce the risk of aggregation and allow smoother delivery are now commonly used. Assessing the degree of embolisation takes some experience and is often a matter of individual judgement.
Pain is the major acute management issue and typically begins within at the end of the procedure when uterine ischaemia is maximal, but this acute phase subsides in 12–24 hours of the procedure. This acute phase is managed by intravenous opioids, paracetamol and NSAIDs. Many institutions use a presacral block at the time of the procedure to manage this acute phase and this often obviates the need for narcotics. The routine use of antibiotics is not usually employed. Pain may continue for five to ten days after the acute phase and is managed by NSAIDs, paracetamol and oral narcotics for breakthrough episodes. A postembolisation syndrome is described with pain, fever, and a raised white cell count. This syndrome may affect as many as one-third of patients undergoing the procedure.
Complication rates from UAE for fibroids are low, although very rarely death has been reported. The potential causes of death are pulmonary embolus and infection, but the rates of complications are less than those for hysterectomy for benign disease. Non-target embolisation is largely precluded by taking microcatheters into the uterus, but damage to the ovary, resulting in premature menopause, and damage to other organs can occasionally cause serious harm. Catheter complications are uncommon in experienced hands. The very rare transcervical expulsion of the fibroid can be a surprise for the patient and so warning should be given. The necrotic fibroid tissue can become infected occasionally necessitating hysterectomy, but this occurs very rarely.
The results of UAE are good with appropriate patient selection and an experienced interventional radiologist. Technical occlusion can be achieved in more than 90 per cent of cases, with arterial spasm or inability to access the uterine arteries as causes of failure. Symptoms of menorrhagia are often ameliorated quickly, but bulk symptoms with larger fibroids may take many months to resolve. Reduction in the size of the fibroids is achieved in the majority of cases. Failure to resolve symptoms may be owing to many factors, but if incomplete embolisation is suspected this is best assessed by contrast-enhanced MRI, which will clearly record the size, vascularity and position of fibroids.

Figure 6. Embolisation of incompetent LOV for treatment of pelvic congestion and vulval varicose veins.
Postoperative haemorrhage
Haemorrhagic complications of pelvic surgery are uncommon, but can be difficult to manage. Like many other types of intra-abdominal surgery, there is potential for delayed bleeding and management of women with a significant haemoperitoneum following procedures such as hysterectomy can be challenging. More recently, the use of mesh support in pelvic floor reconstruction and prolapse surgery has added an element of complexity to control of postoperative bleeding. Bleeding is this setting commonly has a large extraperitoneal component and even at laparotomy it can be very difficult to identify points of haemorrhage. As well, the repeat anaesthesia and surgery exposes a compromised patient to further risk. CT and angiography have allowed precise identification of bleeding vessels with embolisation of arterial bleeding providing a non-invasive approach for control.
CT is an essential tool for pre-intervention assessment of the bleeding postoperative patient, establishing that active bleeding is still occurring and in detailing the anatomy of the vessels involved. Angiography from a femoral approach will identify the bleeding vessel by the extravasation of contrast material. Using coaxial guiding and microcatheters the bleeding vessel is catheterised and then occluded with microcoils, glue or other embolic material. Embolisation aims to stop or reduce the rate of extravasation, allowing the normal physiologic haemostatic mechanisms – vasospasm and clotting – to come into play. Endovascular techniques can stop bleeding and help reduce tissue ischaemia and, in many cases, prevent secondary exploratory laparotomy. Complications are uncommon, but include non-target embolisation, for example gluteal ischaemia from the embolic material moving into the posterior division of the internal iliac artery. Pain and transient fever may also occur, but these are often difficult to distinguish from the postoperative course of the operation itself. The femoral access site can also bruise and requires pressure and avoidance of leg flexion for a few hours.
Conclusion
In obstetrics and gynaecology, endovascular procedures are well-established and safe, offering minimally-invasive management options in obstetric settings such as peri-operative care during caesarean section for placenta accreta and postpartum haemorrhage. The gynaecologist may also consider uterine artery embolisation for women with symptomatic uterine fibroids or in management of post-operative haemorrhage. A good working relationship with your interventional radiologist can yield great advantages for women.
Further reading
Dubois J, Garel L, Grignon A, et al. Placenta percreta: balloon occlusion and embolization of the internal iliac arteries to reduce intraoperative blood losses. Am J Obstet Gynecol. 1997; 176: 723-6.
Teixidor Vinas M, Chandraharan E, Moneta MV, Belli AM. The role of interventional radiology in reducing haehorrhage and hysterectomy following caesarean section for morbidly adherent placenta. Clin Radiol. 2014; 69: e345-51.
Lopera J, Suri R, Kroma GM. Role of interventional procedures in obstetrics and gynaecology. Radiol Clin N Amer. 2013; 51: 1049-66.
Muffly TM, Paraiso M, Gill AS, et al. Interventional radiologic treatment of pelvic haemorrhage after placement of mesh for reconstructive pelvic surgery. Obstet Gynecol. 2012; 119: 459-62.
Ananthakrishnan G, Murray L, Ritchie M, et al. Randomized comparison of uterine artery embolization (UAE) with surgical treatment in patients with symptomatic uterine fibroids (REST trial): subanalysis of 5-year MRI findings. Cardiovasc Intervent Radiol. 2013; 36: 676-681.







Leave a Reply