A brief history of the College’s Provincial Fellows shows the value of coming together for mutual support and learning opportunities.
The development of specialist obstetrics and gynaecology practice is a relatively recent one. The parent body, the Royal College of Obstetricians and Gynaecologists, the organisation from which the Australian and New Zealand Colleges (later amalgamated) budded, was founded in 1929. Previously, there had been societies formed by those who saw obstetrics and gynaecology as a specialist area in its own right. Specialist practice brought with it the establishment of standards of care, specifically targeted research, a training program and eventually a program for continuing education.
Like many advances in medicine, the benefits are felt firstly in the cities, only filtering into the countryside sometime later. So it was that in the 1970s and 80s, specialist obstetrics and gynaecology practice came to the provinces. Prior to this time, the workforce was almost exclusively GPs, many of whom held diplomas from the RCOG, as a considerable proportion would have had postgraduate experience in UK hospital maternity units. These doctors were often cradle-to-grave practitioners who were held in high esteem by their communities and were given credit for doing the best they could in the presence of unfavourable outcomes. Their isolation was often compounded by poor road access and lack of any emergency aerial transport.
The result of the specialisation of the workforce brought with it a decreased reliance on the general practitioner and the impact of an increased litigation threat and reduced remuneration caused a rapid fall off in the number of GPs doing obstetrics. The consequence of this, as well as other factors such as reduced midwife numbers and rural economic decline, was the subsequent closure of many small maternity units throughout Australia. Deliveries became concentrated into regional units in larger provincial towns, making the role of the Provincial Fellow essential. The initial cohort of Provincial Fellows was largely Australian trained from Australian medical schools, predominately Australian born and male.
This group recognised that they shared similar problems. They were relatively isolated, were less well-resourced and supported than metropolitan colleagues, and needed to be self-reliant and to be prepared for any eventuality. The difficulties of obtaining ongoing training and education were well recognised. As a result, the Provincial Fellows Committee was formed, in 1989, to address the concerns specific to rural practice. Initially, rurality was defined as being more than 100km from a capital city, but subsequently this was changed as the Australian Standard Geographical Classification Remoteness Areas (ASGC-RA) tool, created by the Australian Bureau of Statistics, was adopted. Positions were created on Regional Committees and, subsequently, on the College Council for Provincial Fellows.
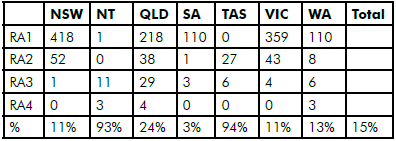
Table 1. Numbers of Fellows, by state and ASGC classification.
The priorities for this newly formed group were establishing a forum for exchanging of ideas and concerns, access to recognised CPD programs and obtaining affordable locum cover to attend meetings and have holidays.
The first Provincial Annual Scientific Meeting (ASM) was held in 1999, in Warrnambool, Victoria, and has been a regular fixture ever since. The meetings have been as much about developing camaraderie among Provincial Fellows and exchanging information as an educational event. The meeting has been structured to give Fellows an opportunity to present papers in areas of their own research or personal interest and, in later years, a forum for engaging with our GP obstetrician colleagues.
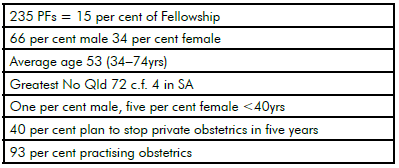
Table 2. Summary of characteristics of PFs in 2012.
The most recent meeting – in Port Lincoln, South Australia, in March 2014 – while well attended by GP obstetricians, Trainees and medical students, was not well supported by Provincial Fellows. To determine why this occurred and to get guidance for the organisation of future meetings, a survey was sent to all Provincial Fellows. A different covering letter accompanied the survey, depending on whether the recipient was a regular attendee or not. The response rate from regular attendees was 53 per cent whereas for the non-attenders it was 39 per cent, with an overall response of 39 per cent. The most significant response from the survey was that there is still strong support for an annual meeting, but that the venue, format and timing will need to be refined in order to attract more delegates.
One other possible conclusion from the survey is that the Provincial Fellowship has also changed remarkably from the time of its inception and that newer Provincial Fellows have a different perception of their position. It is clear that a greater proportion of the workforce is Specialist International Medical Graduates (SIMGs): 33 per cent. Without this group, many of the rural sites would have ceased to function and would have had to close or employ a locum workforce. The result is a greater heterogeneity than the group who originally established the Provincial Fellows Committee.
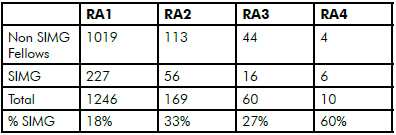
Table 3. Proportion of SIMGs by RA.
As the older group of Provincial Fellows retires from practice, it may be more difficult to maintain the sense of identity that made them such an effective force for improving the conditions of their comrades in the past. Only by fostering and supporting our most recent colleagues and acknowledging their contribution to the welfare of the families of rural Australia, are we going to continue with the spirit that developed within the Provincial Fellowship in the past. To that end, it is vital that those remaining from the initial cohort of Provincial Fellows engage with the newer Fellows, act as advisors and mentors and give encouragement to them to get involved in College activities, including the ASM.
The organisers of the ASM have a responsibility to make the meeting of acceptable academic standard, relevant to rural practice, affordable and at a venue that ensures something for all attending, especially families. After all, for them it may be their only annual holiday.
Honours awards
The following RANZCOG Fellow recently received a New Zealand Honours award:
- Member of the New Zealand Order of Merit
Rev Dr Vincent Jonathan Hartfield, of Whanganui. For services to health.






Leave a Reply