A tool is as safe as the person using it. To use a medical tool properly, the practitioner should be able to appreciate the principles that influenced the way the tool is designed, the reasons for its design features and safe guidelines for its use. This article will outline the use and design of the obstetric vacuum extractor over the past 300 years.
After Malmström publicised his design of a vacuum extractor in 19571, its popularity grew.2 Despite being promoted as safer and less complicated to use than forceps, reports in the English language literature3 soon began to be published suggesting that fetal injury was more common and more significant than with forceps. In the UK, the USA and Australia, forceps were seen as the tool of first choice in instrumental vaginal delivery in the second half of the 20th century. Vacuum extraction developed a reputation for poor obstetric outcomes and an examination of contemporaneous literature reveals why.
As an obstetric registrar, Chamberlain (a future RCOG president) reported in the Lancet4 an account of contemporary vacuum practice in 1965. Applying a vacuum extractor at 4cm dilatation to an occipito-transverse presenting fetal head in a multiparous woman, the cervix was stretched to full dilatation after 12 minutes of traction with delivery ‘affected in a further three minutes’.
In another article in the Lancet5, Huntingford described using vacuum to treat first stage delay. He describes the use of up to 75 minutes of traction, although five of his 11 reported cases were delivered with less than 30 minutes of traction. Another contemporary paper in the precursor journal to BJOG by Inman6 suggests that the total traction time (not time to delivery) in vacuum extraction should be limited to ‘not more than 40 minutes’. This paper states that in St Thomas’s Hospital ‘vacuum extraction is reserved almost entirely for use before full dilatation of the cervix’.
The Australian literature reported similar practices. In a 1967 article in ANZJOG, Fahmy7 suggested that if the fetal head was high, the cup should only be applied if the cervix was ‘at least two-thirds dilated’ and if the head was engaged, applied when the cervix was ‘at least half dilated’. In the 1 500 cases he reported, 236 were in the first stage of labour. To put this practice into context, the caesarean section rate when these cases were managed was only 2.2 per cent. As recently as 1997, a US study in Obstetrics and Gynaecology8 reported results of continuous vacuum time of between less than five minutes to 30 minutes, with poorer outcomes with more than ten minutes of vacuum.
None of these practices would be acceptable today. It is difficult for practitioners in 2015 to appreciate what great lengths obstetricians would go to in the past in order to avoid undertaking caesarean section. The use of vacuum, when forceps was considered to be contraindicated (such as through an incompletely dilated cervix or markedly high head), and excessive periods of vacuum application and traction contributed to the reputation of vacuum as being inherently dangerous. Now, evidence-based guidelines9 limit the use of vacuum to the same clinical preconditions as forceps.
Evolution of design
The earliest report of the use of vacuum extraction was by James Yonge, a naval surgeon, diarist and medical writer. He was the author of several papers published in the ‘Philosophical Transactions of the Royal Society’, including the first report in 1702 of the use of vacuum extraction in obstetrics using ‘cupping’. The next recorded report was by the renowned Scottish obstetrician James Young Simpson. He reported the design and use of a vacuum extraction device to an 1848 meeting of the Edinburgh Obstetric Society, using design features that are similar to some contemporary instruments.
The Simpson10 ‘air tractor’ (1848) had a brass body incorporating a vacuum pump and a leather ‘skirt’ (showing that combining the air pump with the vacuum device is not a new idea). This device (as displayed in the University of Edinburgh medical collection) would not have allowed any flexion or oblique traction (see Figure 1). Simpson abandoned further development of this vacuum device, and three years later demonstrated his forceps design, still used today (basically unchanged) by many obstetricians.
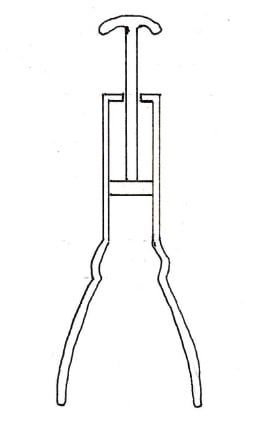
Figure 1. The Simpson air tractor, this design was abandoned in favour of forceps by its designer, James Young Simpson.

Figure 2. The Mälstrom vacuum cup design.
The original Malmström vacuum cup design (1957)11 allowed any oblique direction of traction to create a vector that resulted in rotational forces that tilted the device and lifted the edge of the cup, resulting in loss of suction, and hence detachment (see Figure 2).
The Bird vacuum cup design (1969)12 lowers the traction point on the cup, reducing rotational forces, and allowing better placement over the fetal head flexion point, but still creates a vector that may lift the edge of the cup (see Figure 3).
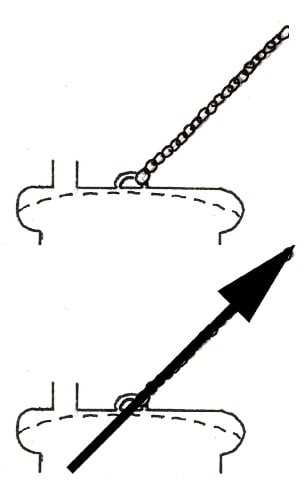
Figure 3. The Bird vacuum cup design.
The O’Neil vacuum cup design (1981)13 modified the Bird design further, with a rotating ring creating a vector that will direct a traction point at the centre of the base of the cup in all but the most acute angles. This reduces rotational forces that may cause detachment (see Figure 4).
As shown in Figure 5, the Kiwi Omnicup (2001)14 has a recessed channel that further lowers the traction point of the vacuum tube (which also supplies traction). Although this facilitates the placement of the cup over the flexion point in a deflexed fetal head, the vector of the traction point, unlike the O’Neil cup15, is still not at the centre of the base of the vacuum cup (but is still closer to the centre and less likely to cause rotational vectors) than the Bird16 or Malmström17 designs).
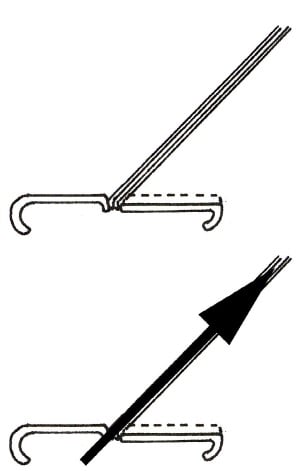
Figure 5. The Kiwi Omnicup vacuum cup design.
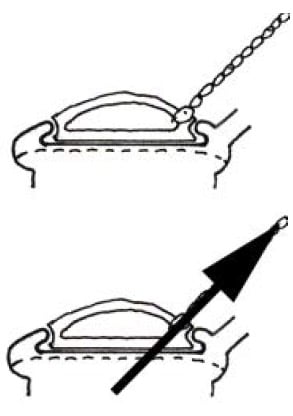
Figure 4. The O’Neil vacuum cup design.
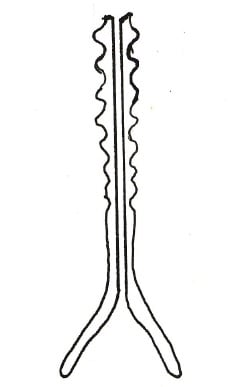
Figure 6. The Kobayashi vacuum cup design.
Soft cups, although claimed to be less traumatic to the fetal scalp, such as the Kobayashi cup18 from 1973 (see Figure 6) or bell cups, are unable to be placed on the flexion point of the fetal head unless flexion is already present. Any oblique traction is more likely to result in detachment. The soft mushroom cup (see Figure 7) has many of the limitations of the Malmström19 design with a high traction point and vector that is more likely to rotate the cup and lose suction.
Conclusion
The adage that a poor craftsman blames his tools is particularly relevant to vacuum extractors. If a vacuum extractor is used when instrumental delivery should not be attempted – or in ways that the instrument was not designed for (such as using a Bell cup to attempt rotation) – then the instrument may fail to achieve its intended use and potentially cause harm. Used by a practitioner with an understanding of its design and limitations, the vacuum extractor is a safe and effective instrument.
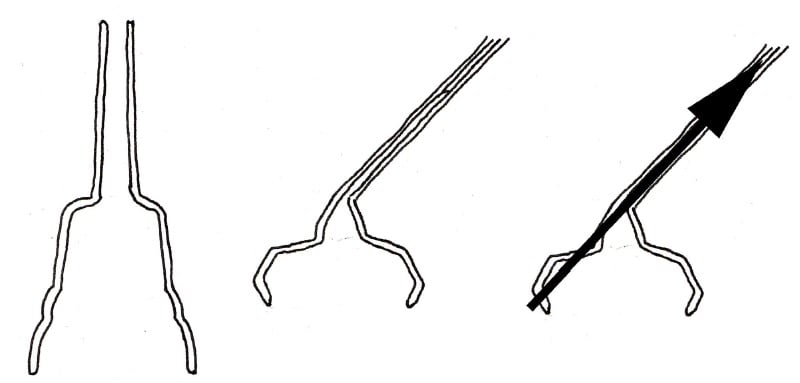
Figure 7. Bell cups are soft and it has been claimed that they are less traumatic to the fetal scalp; however, they have many limitations.
References
- Malmstrom T. The Vacuum Extractor an Obstetrical Instrument and the Parturiometer a Tokographic Device. Acta Obst Gynec Scandinav. 1957;36(S3).
- Berggren O. Experience with Malmstrom’s Vacuum Extractor. Acta Obst Gynec Scandinav. 1959;35:315.
- Aguero O, Alvarez H. Fetal injury due to the vacuum extractor. Obstet Gynecol. 1962;19(2):212-7.
- Chamberlain G. The Vacuum Extractor: A possible danger. Lancet. 1965;285(7386):632.
- Huntingford P. The vacuum extractor in the treatment of delay in the first stage of labour. Lancet. 1961;278(7211):1054-7.
- Inman S. The use of the vacuum extractor in the first stage of labour. J Obstet Gynaec Brit Cwlth. 1969;76:354-8.
- Fahmy K. The Place of the Vacuum Extractor in Obstetric Practice. ANZJOG. 1967;7:114-21.
- Teng F, Sayre J. Vacuum Extraction: Does Duration Predict Scalp Injury? Obstet Gynecol. 1997;89:281-5.
- Vacca A. Reducing the Risks of a Vacuum Delivery. Fetal and Maternal Medicine Review. 2007;17(04):301.
- Simpson J. The air tractor. Edinburgh Obstetric Society. 1848.
- Malmstrom T. The Vacuum Extractor an Obstetrical Instrument and the Parturiometer a Tokographic Device. Acta Obst Gynec Scandinav. 1957;36(S3).
- Bird G. Modification of Malmstrom’s Vacuum Extractor. BMJ. 1969;3(5669):526.
- O’Neil AGB, Skull E, Michael C. A New Method of Traction for the Vacuum Cup. ANZJOG. 1981;21(1):24-5
- Vacca A. Operative vaginal delivery: clinical appraisal of a new vacuum extraction device. ANZJOG. 2001;41(2):156-60.
- O’Neil AGB, Skull E, Michael C. A New Method of Traction for the Vacuum Cup. ANZJOG. 1981;21(1):24-5
- Bird G. Modification of Malmstrom’s Vacuum Extractor. BMJ. 1969;3(5669):526.
- Malmstrom T. The Vacuum Extractor an Obstetrical Instrument and the Parturiometer a Tokographic Device. Acta Obst Gynec Scandinav. 1957;36(S3).
- Maryniak G, Frank J. Clinical Assessment of the Kobayashi Vacuum extractor. Obstet Gynecol. 1984;64:431-5.
- Malmstrom T. The Vacuum Extractor an Obstetrical Instrument and the Parturiometer a Tokographic Device. Acta Obst Gynec Scandinav. 1957;36(S3).





Leave a Reply