The incidence of primary lung cancer in young women in Australia is extremely low, with only 42 cases in women aged less than 40 years diagnosed nationally during 2007, an age-specific rate of less than 0.7 per 100 000.1 Concerns have been expressed that the combination of smoking in young women, increased maternal age during pregnancy and increasing incidence of lung cancer worldwide may cause an increase in pregnancy-associated lung cancers.2
Case report
During a routine screening medical examination before an overseas posting, at age 29, the otherwise asymptomatic female patient was noted to have a left lung mass on her chest radiograph (see Figure 1). The patient had no previous history of respiratory disease and was a lifetime non-smoker, with no other significant illness and no contributory family history. Subsequent computed tomography (CT) showed a 42mm lobulated mass in the left lower lobe of the lung.
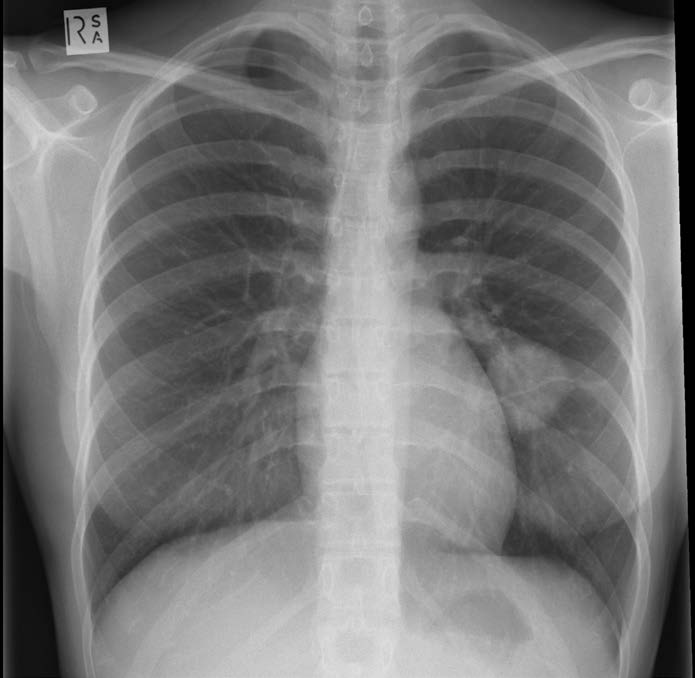
Figure 1. Chest radiograph revealing left lower lobe lung tumour.
After bronchoscopy and biopsy, a diagnosis of lung poorly differentiated adenocarcinoma was made. A positron emission tomography (PET) scan showed uptake in the primary in the left lower lobe and equivocal uptake in the ipsilateral hilar nodes. A left pneumonectomy was performed. The tumour was a 42mm poorly differentiated adenocarcinoma with perineural and lymphovascular space invasion. Three hilar nodes and one mediastinal node contained metastatic disease. The pathological stage was IIIA (see Figure 2).
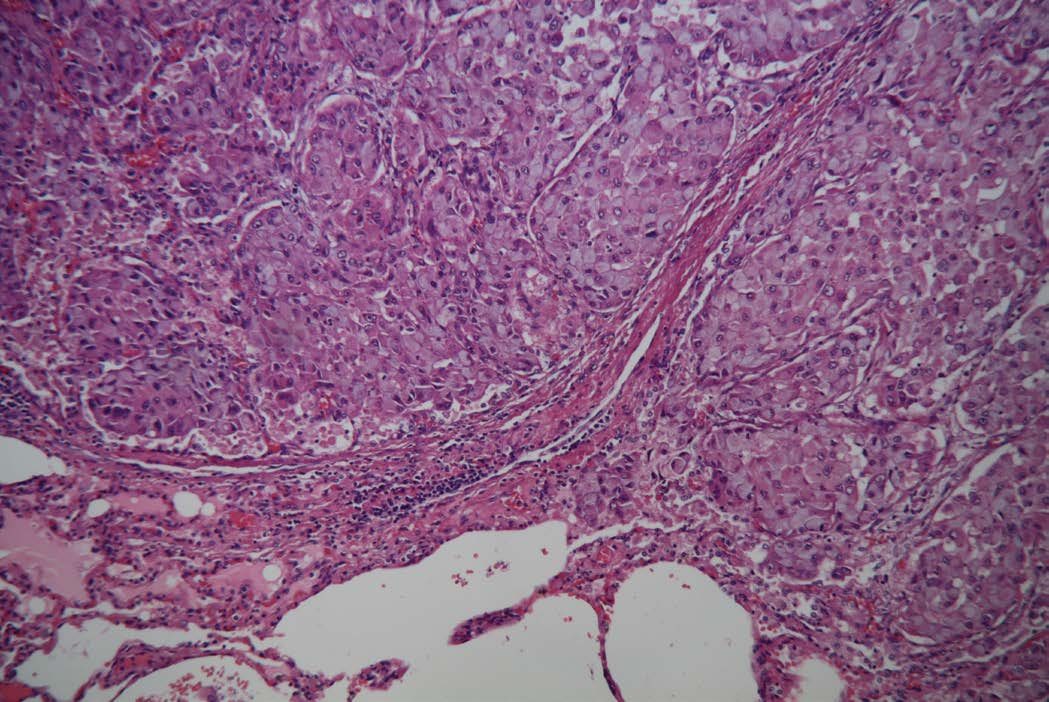
Figure 2. Tumour histology revealing poorly differentiated adenocarcinoma with perineural and lymphovascular space invasion. (H&E staining, 40x).
Subsequent testing revealed the tumour was epidermal growth factor receptor (EGFR) negative and anaplastic lymphoma kinase (ALK) mutation positive. The patient was managed with adjuvant chemotherapy and radiotherapy. In consultation with the treating team, she did not undergo fertility treatment to cryopreserve either oocytes or embryos.
Adjuvant radiotherapy was delivered to the mediastinum in order to reduce the risk of local recurrence. A conformal beam arranged was employed given a dose of 50.4 Gray in 28# over six weeks. The mean lung dose to the right lung was 4.6 Gray and the V20 was seven per cent. The risk of radiation pneumonitis therefore was low as was the risk of significant pulmonary fibrosis.
The patient did not recall disruptions to her menstrual cyclicity subsequent to the chemotherapy. She and her husband began actively trying for pregnancy and menstruation was regular in the lead up to pregnancy. There were no delays in achieving an ongoing pregnancy by which time the patient was 32 years old. During the first trimester, the patient was found to have a resting pulse of 100 per minute, oxygen saturation on room air of 98 per cent and blood pressure of 98/68 mmHg. There was tracheal deviation to the left.
By the second half of pregnancy, the patient had a six-minute walk distance 80 per cent of the predicted value for age and significant oxygen desaturation with exercise. Echocardiography was difficult post-pneumonectomy. At one point, she developed an upper respiratory tract infection and became very breathless. By 26 weeks of gestation, oxygen saturation was 98 per cent on room air, pulse 92/minute and she had no clinical features of right ventricular strain, with the chest clear to auscultation. Obstetric progress was normal, with no maternal hypertensive, diabetic or other complications. Fetal ultrasound surveillance revealed growth on the 26th centile, but normal umbilical Doppler signatures.
After a multidisciplinary discussion between the treating team, the patient was delivered by elective caesarean section under general anaesthesia at 36 weeks of gestation. The choice of general aesthetic over a regional approach was made on the basis that the patient had a reasonable exercise tolerance and the availability of Sugammadex meant that muscle relaxation could be completely reversed at the end of the procedure. Potential intraoperative and postoperative disturbance of respiratory muscle function with a regional anaesthetic was thought to be associated with greater risk.
The patient had an unremarkable postnatal recovery and the baby, a boy weighing 2.57kg (just above the 25th centile for gestation) was in good condition and normal, and subsequent development to six months has been unremarkable.
Discussion
A review of all cases of lung cancer during pregnancy registered in the international Cancer in Pregnancy registration study (CIP study: www.cancerinpregnancy.org) reported only nine cases in total.3 The reports originated from four European centres, with patients having a median age of 33 years (range, 26–42). The median gestational age at diagnosis was 17 weeks, but ranged from six to 28 weeks. All of the nine patients presented with distant metastases to sites including bone, lung, brain, spinal cord, pleura, lymph nodes, adrenals and liver. Histopathology was compatible with adenocarcinoma in four patients, non-small cell lung cancer with unidentified subtype in two patients, and squamous-cell, large-cell undifferentiated and poorly differentiated carcinoma in the remaining three patients. The maternal postpartum outcomes were poor, with less than one year survival following delivery. One of the patients experienced a miscarriage, and three of the pregnancies were terminated. Of the five remaining babies, all were delivered preterm by caesarean section because of poor maternal status, with the median gestational age at 30 weeks (range 26–33). The authors concluded that ‘lung cancer in pregnancy has a dismal maternal outcome in our series.’
One subsequent case report from Portugal described that case of a 36-year-old woman, a known smoker, diagnosed with metastatic lung adenocarcinoma of the left lung at 27 weeks of gestation.4 She was delivered by caesarean section at 29 weeks gestation, then received a combination of chemo- and radiotherapy. The authors reported a progression-free survival of nine months, but the patient died 19 months after first diagnosis.
The only case report similar to our patient is from Japan and was published in 1994.5 That patient was 25 years old, and underwent right middle lobectomy for well-differentiated papillary adenocarcinoma followed by adjuvant radiotherapy. Five years after treatment, she conceived and delivered a healthy child, then had another child two years later.
Pregnancy management for a woman with previous stage III primary lung adenocarcinoma, managed by pneumonectomy has not been reported in the literature. There are reports of successful pregnancy in women with only one lung following treatment for benign conditions, such as tuberculosis and bronchiectasis; however, they do not have the burden of postoperative radiotherapy. A study of 80 women who had undergone pneumonectomy for benign disease during the period 1947–54 reported: pneumonectomy for a nonprogressive disease of one lung in a woman of childbearing age is associated with a nearly normal obstetric history and life expectancy.’6 A similar study of 47 women who had lost a lung to benign disease, published in 1967, concluded ‘all reports of pregnancy after pneumonectomy have confirmed the prediction that this added burden does not prove troublesome either during pregnancy or at the time of delivery.’7
Conclusion
Lung cancer in women of reproductive age is extremely uncommon, with only 11 other cases reported in the literature. When the diagnosis is made during pregnancy, the prognosis is uniformly poor. For cases of primary lung cancer diagnosed and treated successfully before pregnancy, the outlook for the mother and baby appears good.
References
- Australian Institute of Health and Welfare, and Cancer Australia 2011. Lung cancer in Australia: an overview. Cancer series no. 64. Cat. no. CAN 58. Canberra: AIHW.
- Boussios S, Han SN, Fruscio R, et al. Lung cancer in pregnancy: report of nine cases from an international collaborative study. Lung Cancer. 2013; 82(3): 499-505.
- Boussios S, Han SN, Fruscio R, et al. Lung cancer in pregnancy: report of nine cases from an international collaborative study. Lung Cancer. 2013; 82(3): 499-505.
- Neves I, Mota PC, Hespanhol VP. Lung cancer during pregnancy: an unusual case. Rev Port Pneumol. 2014; 20(1): 46-9.
- Satoh H, Yano H, Yazawa T, Hasegawa S. Successful pregnancy after curative therapy for advanced lung cancer. Chest. 1994; 105 (1): 307-8.
- Laros K. The postpneumonectomy mother. Respiration. 1980; 39 (4): 185-7
- Gaensler E, Strieder J. Pregnancy following pneumonectomy. Ann Thorac Surg. 1967; 4 (6): 581-97.






Leave a Reply