Among the crimes of Agnes Sampson, a midwife and the first woman to be burned at the stake for witchcraft in Scotland, in 1591, was that she had used her supernatural skills to relieve the pain of labour. The dominant (in other words, male) view throughout Europe was that such interventions were potentially dangerous – pain was physiologically important for the normal progress of labour and to prepare the fetus for birth. More importantly, pain relief in labour was sinful. God had decreed that women should bear children in pain as punishment for Eve’s surrender to temptation; how dare anyone presume to interfere with His will?
These attitudes were of little practical importance for most of human history. Apart from opium, which had been used for pain relief for hundreds of years, there were few effective treatments. Moreover, until the 16th century, opium could only be administered effectively by smoking. It was the Renaissance physician and alchemist, Paracelsus, who recognised that opium was soluble in alcohol, resulting in an orally effective form, which became known as laudanum, a mainstay of classical medicine. It was not until 1885 that Alexander Wood described the use of the hypodermic needle and syringe to further enhance the usefulness of opium alkaloids.
However, the mid-19th century also saw the discovery of two other potent forms of pain relief, diethyl ether and chloroform. Chloroform initially gained popularity in Europe as a ‘party drug’ and it was only after the Scottish obstetrician James Young Simpson and a group of his friends had been rendered unconscious in that context that Simpson recognised its potential for use in his patients. He is credited with giving the first general anaesthetic for childbirth, in 1847, and soon became a strident advocate.
The popularity of chloroform-assisted childbirth grew rapidly, despite the usual quasi-medical and religious objections, mainly as a result of the demand by women. The reported use of chloroform by prominent women helped the cause. One of the most notable was Emma Darwin, who was administered the drug by her famous husband, Charles, and who went on to demand chloroform for subsequent births.
Undoubtedly, the ultimate endorsement should have come from Queen Victoria herself, and so it is often stated, but it was not to be. Despite ultimately giving birth to nine children, it was well-known that the Queen disliked pregnancy, describing it as ‘wretched’. She had also suffered mild postpartum depression after her first two pregnancies. It was therefore not surprising that, after receiving a pamphlet from the Duchess of Sutherland during her sixth pregnancy, both the Queen and Prince Albert developed a keen interest in the potential of chloroform.
Unfortunately, the first death from chloroform, in a 15-year-old girl, had recently been reported (chloroform was ultimately abandoned owing to its tendency to cause dangerous cardiac arrhythmias) and the royal physicians expressed their strong opposition. However, by Victoria’s eighth pregnancy, in 1853 (with Prince Leopold), confidence in its use had grown. Prince Albert, a long-standing champion of the sciences, had become an advocate and had discussed the subject with London’s foremost exponent of chloroform, the brilliant Dr John Snow, who would, the following year, cement his place in medical history when he correctly identified the Broad Street pump as the source of London’s cholera epidemic.
So it was, that on 7 April 1853, Dr Snow was summoned to administer chloroform to the labouring monarch. Dr Snow’s notes recorded ‘…her Majesty expressed great relief from the application, the pains being trifling during the uterine contractions…’

John Snow originally described his inhaler in
1847. One canister was used for cold water and
the other for chloroform. The brass face mask
was attached to the end of the flexible tube so
the patient could inhale the anaesthetic vapours.
(Science Museum, London, Wellcome Images
reproduced under licence CC BY 4.0.)
Surprisingly, in the medical bulletins immediately following the birth and in the newspapers, no mention was made of the use of anaesthesia. A report was eventually published in an editorial in the Association Medical Journal, the forerunner of the BMJ. It has been suggested that the information in the editorial came from the vocal and ardent James Simpson, who obtained it from the royal obstetrician, Sir James Clark. The Lancet treated the information as mere rumour, advising that ‘the Queen was not rendered insensible by chloroform or any other anaesthetic agent’. This was true as far as it went – Snow had administered chloroform on a handkerchief and successfully maintained light sedation only.
None of the British lay newspapers made much of these reports, though a couple did reproduce the facts, without comment. These included the London Globe, but neither the Times nor the Morning Chronicle, London’s biggest papers, picked up the story. Indeed, it was not until 1869, in John Snow’s obituary, that the Times alluded to the fact at all.
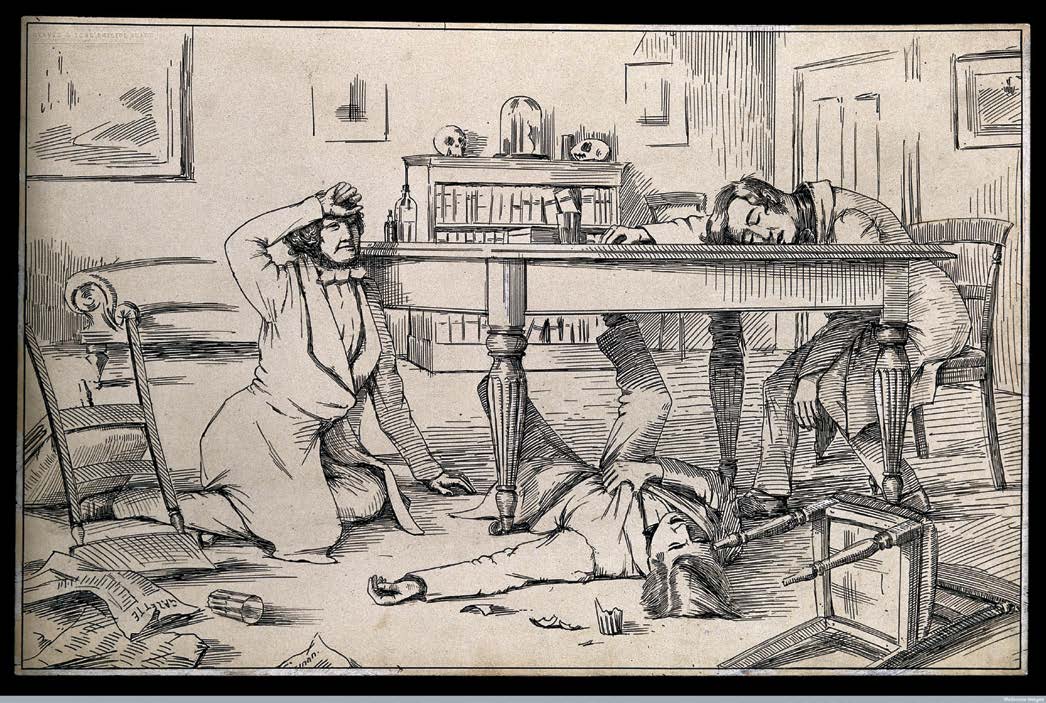
The effects of chloroform on Simpson and his friends (pen and ink 1840s). (Wellcome Library, London, reproduced under licence CC BY 4.0.)
Although there was a gradual increase in the use of chloroform during labour in the ten years or so following Queen Victoria’s experience, the real push for routine pain relief during labour had to await the ‘first wave’ of feminism early in the 20th century. Early feminists supported the relief of pain during labour as a liberating influence, allowing women choice and control. They linked the availability of effective analgesia with improved maternity care in general. They demanded that childbirth be taken more seriously, including the ‘right’ to bear children in hospital, where responsive, respectful medical care could be expected.
So why did the revolutionary use of chloroform during childbirth by Queen Victoria pass with barely a whimper? Was there some kind of conspiracy to keep it secret? There is no evidence of an overt conspiracy, but it is clear that both the medical and religious establishments retained their disapproval of ‘interference’ in the natural and sacred process of labour. Though one could not openly disapprove of the choices made by the Queen, it seems to have been tacitly understood that such activities should not be promoted to the masses.
By the time the early feminists came on the scene around 1900, chloroform was already on the wane and the feminist campaign for pain relief in labour ultimately coalesced around a technique, subsequently also discredited and abandoned, called ‘twilight sleep’, which involved the use of morphine and scopolamine (hyoscine) in combination. Despite improving technologies, such as epidural analgesia, the second wave of the feminist movement, in the 1960s, held views diametrically opposed to those of their predecessors and rejected pain relief as part of the male medicalisation of childbirth in favour of ‘natural birth’. They drew support from other pseudo-scientific promoters of natural childbirth, such as Lamaze and Dick-Read. For the second-wave zealots, a woman who ‘gave in’ to pain relief had fallen under the spell of the male doctors and was considered something of a turncoat.
Fortunately for women everywhere, there is now a growing third wave among academic feminists, which again favours the use of pain relief as a valid feminist choice for the labouring woman. Queen Victoria may yet be vindicated!
Further reading
Skowronski GA. Pain relief in childbirth: changing historical and feminist perspectives. Anaesth
Intensive Care. 2015; 43 Suppl: 25-8.
Connor H, Connor T. Did the use of chloroform by Queen Victoria influence its acceptance in obstetric practice? Anaesthesia. 1996; 51: 955-957. Beckett K. Choosing Cesarean. Feminism and the politics of childbirth in the United States. Feminist Theory. 2005; 6:251-275.





Leave a Reply