Qui Tacet Consentire Videtur – She who is silent appears to consent.
We all appreciate consultations where the patient is accepting of the advice offered and has few questions. However, silence during the process of consent may be no longer as ‘golden’ as it once was. It may be a dangerous prelude to a medicolegal action which was, in retrospect, totally preventable.
Autonomy in law means the right to self-determination. Even when a patient refuses valid life-saving measures, their right to do so must be respected. Consent to a surgical procedure requires that the recipient understands the nature of the procedure and its ramifications. Fully informed consent may seem like an unrealistic ideal, however, risks relevant to a particular patient must be ascertained and discussed; these are the ‘material risks’. To reflect this, the term ‘valid consent’ is replacing ‘informed consent’. Obtaining valid consent requires time and patience; one consultation may not be sufficient. Handing the patient a treatment information pamphlet and recording its receipt does not constitute adequate explanation and patient understanding.
Medical negligence
For a successful claim of negligence against a doctor, the plaintiff must establish the following:
- the doctor owed the plaintiff a duty of care;
- the doctor owed the plaintiff a duty of care;
- the doctor breached the duty of care, that is, failed to meet the required standard of care;
- the breach of duty caused the plaintiff to suffer injury;
- the injury was foreseeable; and
- the injury is of a kind that is compensable at law.
Issues of inadequate consent go to the standard of care provided. The legal test relating to the provision of information differs from the test regarding reasonable diagnosis and treatment, which is in the practitioner’s domain. The key difference is that the patient decides what is reasonable information about a proposed procedure based on her ‘needs, concerns and circumstances’.1 Reasonable diagnosis and treatment, on the other hand, is determined by the practitioner whose standard must meet that of an ordinary competent peer professional practising in that field. The High Court has held that ‘no special medical skill’ is required to disclose medical information to a patient and therefore it is the Court who will decide if the provision of information met the needs of the plaintiff.2
Disclosure of risk
Under the common law of trespass, patients have a right not be subjected to an invasive procedure without consent, unless an urgent life-saving intervention is required3 Trespass is a legal term meaning a deliberate physical interference with a person or their property without permission. Ethical medical practice also requires that consent to a procedure is obtained as part of the duty of care. The prerequisites are that the patient has sufficient mental capacity to understand the explanation and that the explanation is sufficiently comprehensive to enable voluntary consent to be given or refused.
Material risks are those that for a particular patient are relevant and important and that a practitioner knows or should know would influence a patient’s decision to consent before proceeding. For example, if a patient wants to ensure that no damage is sustained to a functional eye by a procedure to the other blind eye, then that is ‘material’4 even if the risk is remote.
In the UK, the standard of risk disclosure is to conform to the professional standard of one’s peers.5 Australia has chosen a slightly different path with the introduction of the Civil Liabilities Act 2002, whereby the practitioner cannot be held liable if it can be established that they acted in a manner that was accepted by a body of peer professional opinion as competent professional practice. That need not be a widely accepted opinion, but must be rational (NSW, Qld, SA, Tas) or reasonable (Vic) or not so unreasonable that a reasonable health professional would have rejected it (WA).6
Understanding risk
Informed consent means legally that ‘an individual has been given full or adequate disclosure’.7 If ‘full’ was interpreted to mean that every conceivable risk was canvassed with the patient, then that would be impractical. Valid consent infers that the patient has been informed of the nature and purpose of any proposed treatment, as well as the likely outcome(s).This includes any significant potential adverse outcomes, and the likely result of not proceeding with the proposed treatment. All this is necessary so that an individual can make an informed decision. Alternative treatments should be discussed. The operative experience of the proceduralist for the proposed operation might also be relevant to the patient.8
An oft-neglected part of the consent process is whether the patient truly appreciates the risks explained. Even if these are correctly appreciated, there may be a false assumption by the patient that if these risks eventuate, they can always be quickly and completely rectified. In doing so they may be underestimating their significance. For example, the patient who is told that a cut ureter sustained at hysterectomy can be re-joined, may not appreciate the long process of recovery, the prolonged use of ureteric stents or the subsequent bladder dysfunction and urinary tract infections that may follow. Similarly, the catastrophic risks of a rubella embryopathy are not simply solved by the supply of a ‘glass eye, an artificial heart valve and a bionic ear’ to the affected infant, as one pro-life obstetrician once claimed.
The National Health and Medical Research Council Guidelines for Medical Practitioners on Providing Information to Patients9 emphasise the importance of patient comprehension of the information provided. This may require repeated explanations that are free from jargon, giving the patient sufficient time to digest the information provided. Supplementary diagrams and written information may aid understanding and several patient encounters may be necessary.
Obstetric risk
Claims of negligence may arise when an obstetric patient asserts that her obstetrician failed to provide her with sufficient information to make an informed decision regarding management. This might occur where the obstetrician chose not to reveal information received in an ultrasound report describing suspicious ‘soft signs’ of aneuploidy and decided not to undertake further investigations. The test of disclosure of obstetric risk is the degree of detail that would be required by a reasonable person. Obstetricians need to determine what each ‘reasonable’ mother expects. What is reasonable to one mother may be completely inadequate to another patient who perhaps has a personal or family history of fetal anomalies. The test in Rogers10 is relevant when risks that the doctor knew or ought to have known would influence the patient’s decision.
Presenting information on risk
In the UK, the RCOG11 has offered a rule-of-thumb for interpreting risk (see Table 1). This may make risk meaningful to some patients who struggle to interpret absolute numbers; however, material risk is the real issue and may not be quantifiable.12
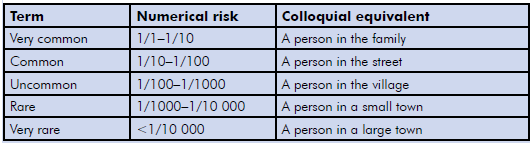
Table 1. The RCOG guidelines for interpreting risk.
Consent in special circumstances
The Guardianship Tribunal
For minors or other patients who lack mental capacity, consent for certain procedures cannot be given by parents or guardians. This particularly applies for procedures that might produce permanent sterility, such as tubal ligation or hysterectomy, or even reversible sterility, such as the administration of Depo-Provera. For such decisions, a Guardianship Tribunal is the necessary decision-maker. This follows the judgement in Marion’s case13 where parents sought to have a hysterectomy performed on their disabled child.
When a fetus may suffer
The fetus has few legal entitlements until birth. Until a fetus is born, it is not considered a ‘person’ in Australian law.14 This follows the sentinel UK case in which Sir George Baker held that: ‘The fetus cannot in English law, in my view, have any right on its own until it is born and has a separate existence from its mother.’15 The principle of respecting a mother’s autonomy may mean that the fetal interests are overridden.
Female sterilisation
Consent for female sterilisation in Australia previously required the consent of the husband, but this was omitted because of human rights considerations. Spousal consent is still required in countries such as Brazil, Chile, Ecuador, Guatemala, Honduras, Japan, Niger, Taiwan, Rwanda and Turkey. In Finland, Hungary and Switzerland, the spouse is required to be informed of the proposed female sterilisation by the applicant.16
There has been recent controversy over the patient’s right to choose tubal ligation, even in their early 20s.17 Many gynaecologists would adhere to previous advice that sterilisation not be done until the patientis at least 30 years of age. Twice the expected rates of requests for reversal were made when sterilisation was performed in younger patients.18 However, the expected rates are only approximately six percent.19 Controversy has arisen because it challenges patient autonomy.
The Federation of International Gynecology and Obstetrics recommends that: ‘No woman may be sterilized without her own, previously-given informed consent, with no coercion, pressure or undue inducement by healthcare providers or institutions.’20
Two important considerations that should be discussed are the failure rate of the proposed procedure and the relative difficulty of tubal reversal. Alternatives to female sterilisation that are availableto the couple, including vasectomy and other reliable long-term methods of contraception, should be discussed with the patient. 21
Cosmetic vaginal surgery
The Medical Board of Australia (MBA) has recently expressed concern regarding the validity of a young person’s consent for cosmetic surgery, including genital surgery. The worry is that such individuals may be motivated by unrealistic expectations of their appearance or attribute social problemsto cosmetic defects. In other words, some young women can be subtly coerced into undergoing cosmetic procedures by the influence of their peers or by their surgeon. The MBA has proposed three-month ‘cooling off’ periods for patients less than 18 years of age, as well as mandatory counselling by a psychologist, psychiatrist or GP.22
Forensic gynaecological exams
Consent for forensic gynaecological examinations is of particular importance as it helps to permit a violated victim to re-establish her autonomy. The consent needs to be comprehensive and should cover general physical examination, abdominal examination, pelvic examination, the forensic and microbiological sampling from the genital organs and the use of any photography, including the release of data to approved recipients. Consent for photo documentation must be obtained.23 Valid consent reflects a legal and moral principle whereby the victim has the right to decide what is appropriate for them. This includes the right to accept or decline a forensic examination and also to change that decision.24
Electronic consent documentation
An electronic signature is not viewed to be as secure as a physical signature because, as an image, it can be copied and used by another individual.25 It is also seen as a less-ideal method for signing documents as it is more difficult to prove the intent of the person to sign. The practitioner needs to
- show that one can identify the person signing and be able to indicate that they knew and agreed to the document or the information they were signing; and
- show that the method used to attach/affix signature was reliable. In other words, you need to be able to establish that the method of electronic signature was reliable, kept secure and was appropriate to be used for that type of document.
Digital signatures, on the other hand, are seen as a more advanced method of signing and have a higher level of integrity. They are seen essentially as an electronic fingerprint; a coded message that is unique to the document and the signer. Digital signatures ensure the authenticity of the signer. They are more widely accepted and a signer cannot later deny they signed after their digital signature is affixed. These consent formats are increasing in frequency, but for the time being a hard copy of the written consent should be retained for use when electronic signatures are not acceptable.
Consent by illiterate patients
It is permissible and valid for an illiterate patient to sign a consent form using a mark such as ‘X’ and the witnessing to such a consent needs to be detailed. The witness must be able to testify as to the validity of the signature. Similarly, patients without language skills or patients who are hearing or vision impaired are potentially capable of giving valid consent; however, the appropriate communication methods or support must be employed and documented in the patient’s medical record. The use of family interpreters is not ideal because of potential conflicts of interest and may be open to later challenge.
Proxy consent
A proxy consent is based on the power of attorney (POA) where, for example, the right of an incompetent patient to consent to treatment is delegated to another adult. About one per cent of people aged 60–64 years and 12 per cent of patients aged 80–84 display signs of dementia, so alternative decision makers for those people are invaluable. The ACT, NSW, Qld, SA and Tas have enacted legislation that allows patients to appoint attorneys with explicit powers to be involved in their medical treatment either to consent to or refuse medical treatment on their behalf. WA may follow. A POA refers to the ‘unilateral grant of authority by a donor for someone else to act on their behalf’. The POA may be general or enduring. The enduring POA continues after the principal has lost mental capacity.
Concluding remarks
When procedures go wrong and litigation follows, the issue of consent looms large in the minds of lawyers. Obtaining valid consent should not be motivated by a defensive mentality, but as an essential part of the therapeutic process. It is simply ‘good medicine’.
Acknowledgements
The advice of Prof Roy Beran AM and Prof Cameron Stewart is gratefully acknowledged.
References
- Rogers v. Whitaker (1992) 175 CLR 479 at 493.
- Rogers v. Whitaker (1992) 175 CLR 479 at 493.
- www.alrc.gov.au/publications/10-review-state-and-territory-legislation/informed-consent-medical-treatment retrieved 24 May 2016.
- Rogers v. Whitaker (1992) 175 CLR 479 at 493.
- Bolam principle-Bolam v Friern Hospital Management Committee (1957) 1 WLR 582.
- Stewart C, Kerridge I, Parker M. The Australian Medico-Legal Handbook
(Sydney, Churchill Livingstone, 2008) at 38. - Australian Legal Dictionary (ed Peter Butt) 3rd edition (Chatswood, LexisNexis Butterworths, 2004).
- Chappel v Hart – [1998] HCA 55.
- National Health and Medical Research Council 1993, General Guidelines for Medical Practitioners on Providing Information to Patients (prepared by the Health Care Committee of the NHMRC), NHMRC, Canberra.
- Rogers v. Whitaker (1992) 175 CLR 479 at 493.
- www.rcog.org.uk/globalassets/documents/guidelines/clinical-governance-advice/cga7-15072010.pdf retrieved 27 July 2016.
- Chappel v Hart – [1998] HCA 55.
- Marion’s Case (1992) 175 CLR 218.
- Attorney-General (Qld) (Ex rel Kerr) v T.
- Paton v British Pregnancy Advisory Service [1979] QB 276.
- Law and Policy Ch. 4 in Contraceptive Sterilization: Global Issues and Trends ( EngenderHealth https://www. engenderhealth.org/files/pubs/family-planning/factbook_chapter_4.pdf retrieved 25 May 2016.
- www.abc.net.au/news/2016-07-21/pregnant-mother-of-two-’too-young-to-be-sterilised’/7649556 retrieved 27 July 2016.
- Curtis KM, Mohllajee AP, Peterson HB. Regret following female sterilization at a young age: a systematic review. Contraception. 73(2):205-10. Epub 2005 Oct 21.
- Wilcox LS, Chu SY, Peterson HB (1990) Characteristics of women who considered or obtained tubal reanastomosis: Results from a prospective study of tubal sterilization. Obstet Gynecol. 75: 661-665.
- FIGO Guidelines on Female Contraceptiveterilization, March 2011, Goa. www.figo.org/sites/default/files/uploads/wg-publications/ethics/English%20 Ethical%20Issues%20in%20Obstetrics%20 and%20Gynecology.pdf retrieved 27 July 2016.
- RANZCOG Female Sterilisation byFilshie clip tubal occlusion C-Gyn22.www.ranzcog.edu.au/documents/doc_ details/930-c-gyn-22-filshie-clip-tubal-occlusion.html retrieved 25 May 2016.
- Sophie Scott, Rebecca Armitage. ‘Cosmetic surgery crackdown: Cooling off period for patients among tough new industry guidelines’ ABC News 11 May 2016 www. abc.net.au/news/2016-05-09/crackdown-on-cosmetic-surgery-includes-cooling-off-periods/7394774.
- Royal Australian College of Physicians. Genital Examinations in Girls and Young Women: A Clinical Practice Guideline. 2009. www.ranzcog.edu.au/editions/doc_ view/458-racp-paediatric-policy-vaginal-examination-in-children-and-young-women. html retrieved 25 May 2016.
- Queensland Government Response to sexual assault: Interagency Guidelines for Responding to People who have Experienced Sexual Assault 2014 https://publications.qld.gov.au/storage/f/2014-09-12T03%3A43%3A29.165Z/qld-govt-guidelines-for-responding-to-sexual-assualt. pdf retrieved 25 May 2016.
- www.startupsmart.com.au/adviceleadership-advice/leadership/are-e-signatures-legal-in-australia/ retrieved 30 May 2016.






Leave a Reply