‘…Wine maketh merry: but money answereth all things…’ Ecclesiastes 10:19 .
While it may seem uncouth to speak of money when considering healthcare decisions, it is important to note that rational, equitable and efficient allocation of scarce healthcare resources is required to maintain a functional healthcare system.
Caesarean section (CS) rates have been rising in Australia and debate rages over the best method of delivery, with significantly higher rates of CS in the private sector than in the public sector.1 It is generally considered self-evident that a CS is more expensive than a vaginal birth (VB), with the add-on costs from presumed additional staff input and longer postnatal stays.
However, this simplistic dichotomy between modes of delivery to explain a comparative economic analysis is severely limited by:
- A failure to adopt an intention-to-treat analysis when comparing groups. The need for instrumental VB and emergency CS in complicated vaginal deliveries, with their heightened rates of maternal and neonatal morbidities and costs, must be accounted for in the planned VB inventory.
- Charges for a birth episode need to include all aspects of antenatal care, the maternal and child length of stay, the neonatal intensive care unit (NICU) use, any repeat postpartum attendances to hospital and long-term sequelae, such as pelvic floor disorders and psychological wellbeing.
- A failure to recognise the inconsistent way that ‘elective CS’ may be defined. It is a heterogeneous group made up of multiple medical indications. Pre-existing obstetric and fetal conditions confound the results. Additionally CS for ‘maternal request’ have been known to be coded by other indications for insurance and liability concerns.2
- Different standards of practice environment for alternative modes of delivery. The risks and benefits to women and their babies will depend on the clinical protocols and expertise on the frontline.
This article aims to review the published evidence for economic differences with regard to mode of delivery for the following three situations:
- Planned VB compared to planned CS
- Planned VB versus planned elective CS in term breech presentation
- Trial of labour (TOL) after CS versus elective repeat CS.
Comparing planned VB to elective CS
Petrou et al published a meta-analysis in 2001, comparing various costs in relation to mode of delivery.3 They reviewed 49 studies that examined the economic aspects of CS and alternative modes of delivery that contained useful economic cost data in regards to the costs of duration of labour, requirement of staff, costs of equipment as well as the long-term costs. These costs were then converted to UK sterling and inflated to 1998 prices using the National Health Service (NHS) Hospital and Community Health Services Pay and Prices Inflation Index.4
Duration of delivery was shortest in the group having spontaneous VB when compared with emergency CS.5 It was hypothesised that a longer duration of labour would lead to larger costs, owing to overhead running costs and staff costs. However, this was largely dependent on the size of the obstetric service, with smaller obstetric services incurring a relatively larger cost with longer duration of labour compared with large academic centres.6
The number of staff – midwifery, nursing and medical – attending an emergency CS compared with a spontaneous VB is larger, though dependent on local practices.7 Consequently, an almost doubling of staff fees has been reported when comparing spontaneous VB to emergency CS.8 9
As women having emergency CS routinely have a longer postnatal stay; unsurprisingly, there is an almost four-fold increase in cost when comparing the postnatal costs of emergency CS to spontaneous VB.10 The long-term risks of CS are well known, including delayed conception, increased risk of ectopic pregnancy, placental adhesive disorder, postpartum depression and difficulties with breastfeeding.11 12 However, few studies compare the long-term healthcare costs of women who have had an emergency CS with those who have had a spontaneous VB. Women undergoing an emergency CS were more likely to incur healthcare costs secondary to increased rehospitalisation rates in the first 60 days postpartum,largely secondary to uterine infections, wound complications and venous thromboembolic complications.13
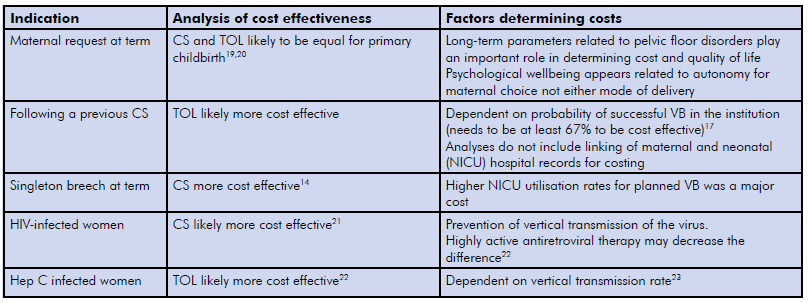
Table 1. Economic analysis of elective CS versus TOL.14
Petrou et al asserted in 2013 on an updated meta-analysis that having an ‘elective CS’ was 1.1–4.1 times the cost of a VB in low-risk pregnancies.2 Kazandjian et al15 rejected the assumption that CS is always costlier that VB. The authors linked maternal and child health records to extract economic data with regard to maternal co-morbidities, mode of delivery and transfer to NICU. They concluded that average total charges for VB (maternal plus baby charges including NICU use) were higher than the equivalent CS cohort by ~$US4000 in 2005. The presence of maternal comorbidities (hypertension and diabetes mellitus) was the major economic influence, owing to the higher necessity for a transfer to NICU.
Mode of delivery and breech presentation
The Term Breech Trial, a multicentre, multinational randomised controlled trial comparing planned VB with planned CS, concluded that composite perinatal and neonatal outcome was significantly lower in the planned CS group when compared to the planned VB group in an intention-to-treat analysis.16 A cost-analysis was undertaken on this data to determine the economic implications of mode of delivery.17
The economic analysis was only carried out on cases from countries with low rates of perinatal death (<20/1000) and included Australia, Canada, Chile, Denmark, Finland, Germany, Israel, Netherlands, New Zealand, Poland, Portugal, Romania, Switzerland, the UK, USA and Yugoslovia.18 The groups were comparable with 515 mothers and 514 infants in the planned caesarean group and 512 mothers and 511 infants in the planned VB group.
Women in the planned VB group had a larger number of antenatal visits, inductions/augmentations of labour, epidural anaesthesia and a longer stay in the antenatal/labour wards. Women in the planned CS group had greater use of spinal anaesthesia, CS and a longer stay on the postnatal ward.19 Infants in the planned CS group had less NICU time and more normal newborn examinations than those in the planned VB group.20
Women in the planned CS group had statistically significantly lower overall costs compared to those in the planned VB (median cost for planned CS $7165 versus median cost for planned VB $8042) largely secondary to increased healthcare worker and hospital fees incurred, as well as higher costs associated with infant stay in NICU.13 The slightly greater cost of performing an emergency CS in the planned VB group did not majorly contribute to the overall differences in costs.21
TOL after CS versus elective repeat CS
Due to rising CS rates, women and clinicians are faced with the decision of trial of labour (TOL) after CS versus an elective repeat caesarean delivery in their subsequent pregnancies.22 Short- and long-term implications of each mode of delivery have been well documented.23 The economic implications, however, have not been well explored.
Fawsitt et al performed a ‘bottom-up’ cost-effectiveness analysis, employing a decision analytic model comparing outcomes of TOL after CS with elective caesarean delivery in a hypothetical cohort of 10 000 low-risk women using outcome data from Ireland and the USA.24 They concluded that the lowest costs were associated with a successful VBAC and that the highest costs were associated with an emergency CS following TOL, due to extended duration of labour and the necessity for the presence of specialised medical staff at delivery. Overall, the study concluded that TOL was more cost effective than elective CS, despite a small increase in maternal morbidity in the TOL group, when the probability of success was greater than 67 per cent.17 Significant limitations to this study included its hypothetical nature, as well as the inability of the study to consider long-term maternal and fetal outcomes.
Further hypothetical cost-effectiveness analyses have confirmed the aforementioned findings;25 however, there is a need for prospective trials to further determine the cost effectiveness of TOL versus elective CS.
Conclusion
The economic differences related to mode of delivery remain specific to clinical circumstances. There remains scarce evidence comparing the costs of planned VB with planned CS. For women attempting a spontaneous VB, an emergency CS is likely to be the greatest economic burden for their care. On hypothetical data, this is also the case for low-risk women attempting a TOL after CS. In women with breech presentation at term, the economics clearly favour an elective CS over an attempted VB.
Money may ‘answereth all things’ but only when supported by robust, prospective evidence. Costs of healthcare remain difficult to define, due to the inability to measure intangible costs and the long-term outcomes associated with healthcare decisions. There is a paucity of economic knowledge with regard to the cost-effectiveness of mode of delivery. Future directions need to include consistent coding of elective CS by indication and the linkage of maternity costs to any ensuing neonatal care costs.
References
- Australia’s mothers and babies reports 1991-2011. Available from: www.aihw.gov.au/WorkArea/DownloadAsset. aspx?id=60129545698.
- Petrou S, Khan K. An Overview of the Health Economic Implications of Elective Caesarean Section. Appl Health Economic Policy. 2013;11:561-576. doi 10.1007/ s40258-013-0063-8.
- Petrou S, Henderson and Glazener. Economic aspects of caesarean section and alternative modes of delivery. Best Prac Res Clin Obstet Gynaecol. 2001;15(1):145-63.
- Hospital and Community Health Care Service Index. Department of Health. Available from: www.gov.uk/government/ organisations/department-of-health.
- Petrou S, Henderson and Glazener. Economic aspects of caesarean section and alternative modes of delivery. Best Prac Res Clin Obstet Gynaecol. 2001;15(1):145-63.
- Hein H, Ferguson N, et al. The cost of maternity care in rural hospitals. JAMA. 1978;240:2051-2.
- Petrou S, Henderson and Glazener. Economic aspects of caesarean section and alternative modes of delivery. Best Prac Res Clin Obstet Gynaecol. 2001;15(1):145-63.
- Fuchs V, Perreault L, et al. Expenditures for reproduction related health care. JAMA. 1986;255(1):76-81.
- Gold R, Kenney A, et al. Paying for maternity care in the United States. Fam Plann Perspec. 1987;19(5):190-206.
- Clark L, Mugord M, et al. How does mode of delivery affect the cost of maternity care? BJOG. 1991;98(6):519-23.
- Allen V, O’Connell C, et al. Maternal morbidity associated with caesarean delivery without labour compared with spontaneous onset of labour at term. Obstet Gynecol. 2003;102(3):1113-35.
- Prior E, Santhakumaran S, et al. Breastfeeding after caesarean delivery: a systematic review and meta-analysis of world literature.
- Lydon-Rochelle M, Holt V, et al. Association between mode of delivery and maternal rehospitalisation. JAMA. 2000;238(18):2411-2416.
- Petrou S, Khan K. An Overview of the Health Economic Implications of Elective Caesarean Section. Appl Health Economic Policy. 2013;11:561-576. doi 10.1007/ s40258-013-0063-8.
- Kazandjian VA, Chaulk CP, Ogunbo S, Wicker K. Does a Cesarean section delivery always cost more than a vaginal delivery? J Eval Clin Pract. 2007;13(1):16-20.
- Hannah M, Hannah W, et al. Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomized multicenter trial. Lancet. 2000;356:1375-83.
- Palencia R, Gafni A, et al. The costs of planned caesarean versus planned vaginal birth in the Term Breech Trial. CMAJ. 2006;174(8):1-11.
- Palencia R, Gafni A, et al. The costs of planned caesarean versus planned vaginal birth in the Term Breech Trial. CMAJ. 2006;174(8):1-11.
- Palencia R, Gafni A, et al. The costs of planned caesarean versus planned vaginal birth in the Term Breech Trial. CMAJ. 2006;174(8):1-11.
- Palencia R, Gafni A, et al. The costs of planned caesarean versus planned vaginal birth in the Term Breech Trial. CMAJ. 2006;174(8):1-11.
- Palencia R, Gafni A, et al. The costs of planned caesarean versus planned vaginal birth in the Term Breech Trial. CMAJ. 2006;174(8):1-11.
- MacDorman M, Declerq E, et al. Recent trends and patterns in vaginal birth after caesarean (VBAC) deliveries in the United States. Clin Perinatol. 2011;38:179-92.
- Lydon-Rochelle M, Cahill A, et al. Birth after previous caesarean delivery: short term maternal outcomes. Sem Perinatol. 2010;34:249-257.
- Fawsitt C, Bourke J, et al. At what price? A cost-effectiveness analysis comparing trial of labour after previous caesarean versus elective repeat caesarean delivery. PLOS ONE. 2013;8(3):e58577
- Gilbert S, Grobman W, et al. Lifetime cost-effectiveness of trial of labour after caesarean section in the United States. Value in Health. 2013;16:953-964.







Leave a Reply