Since pelvic floor trauma, such as levator ani avulsion, is a possible injury sustained at vaginal delivery and is associated with chronic pelvic floor dysfunction (PFD), should informed consent be routinely obtained in women attempting vaginal birth?
In O&G Magazine, Autumn 2014,1 we reviewed epidemiological evidence (Table 1) on partial protection of caesarean section (CS) on aspects of PFD, especially for pelvic organ prolapse (POP). POP is a particularly significant problem with lifetime risk for surgery of up to 20 per cent and high re-operation rate of up to 30 per cent.2 3, In the USA, it has been estimated that approximately 200 000 prolapse procedures are performed annually4 with a direct cost of over US$1 billion.5 With the ageing population, prevalence of surgery for PFD is likely to increase substantially. The aetiology of PFD is multifactorial and still not well understood, but includes childbirth, changes in collagen metabolism,6 7 obesity,8 ageing9 10 and menopause.11 Evidence from epidemiological and observational cohort studies suggests that vaginal birth (VB) is the main aetiological factor.12 13 14 15 Levator ani muscle (LAM) injury has been postulated as the missing link between VB and POP.16 17
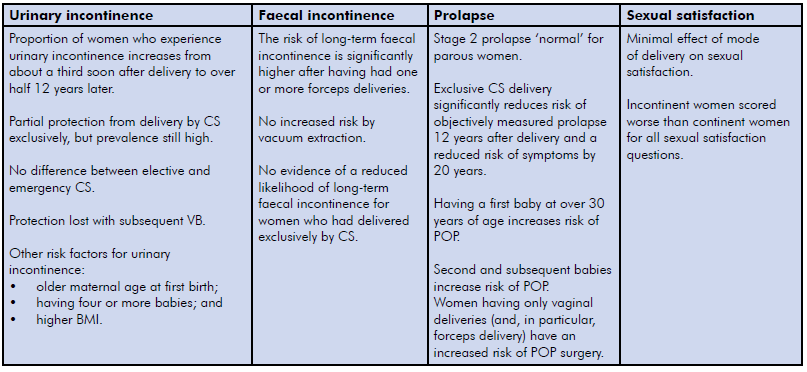
Table 1. ProLong and other epidemiological studies – conclusions to date.
Obstetric demographics have also changed in many ways in recent years, such as increasing BMI and maternal age at first delivery, along with additional factors, such as allowance of long second stage and pressure to lower CS rates as a clinical indicator;18 19 20 21 22 23 24 these may further increase the likelihood of PFD. In the current era of increasing public expectations from birth care providers and evolving information seeking behaviour, birth care providers should be able to impart accurate information to women in constructing their delivery plans.
We recently conducted a 20-year follow up on the Dunedin, New Zealand arm of the collaborative longitudinal study ProLong (PROlapse and incontinence LONG-term research study). While we await data from Birmingham and Aberdeen; on the Dunedin cohort alone, we found significant associations between mode of delivery, evidence of persistent pelvic floor trauma and development of aspects of PFD. 25 26 We will highlight some of our findings to emphasise the urgent need for ongoing research and refinement of risk-predicting tools to better counsel women regarding PFD risks and its prevention.
Pelvic floor trauma at childbirth
Pelvic floor trauma sustained during vaginal childbirth is not limited to the apparent perineal trauma alone. It also includes LAM avulsion, levator hiatal overdistension and obstetric anal sphincter (OASIS) injuries. Damage to the pudendal nerve and endopelvic fascia has also been described.27 These are associated with long-term morbidities affecting women’s quality of life.
During VB, the LAM undergoes tremendous stretch, ranging from 25 per cent to 250 per cent of its original length.28 It has been shown that skeletal muscle will not stretch to greater than twice its length without tearing.29 Substantial macro- and microscopic muscular injuries may occur when a skeletal muscle fibre is stretched to more than 1.5 times its original length.30 It is thus surprising that more than half of women suffer no discernible change in the distensibility or morphological appearance after VB, which may be attributed to hormonal influence.31 This sudden and excessive stretching of the LAM during VB may result in two forms of LAM injury: LAM avulsion (macrotrauma) or levator hiatal overdistension (microtrauma). LAM avulsion with a reported incidence and prevalence of 14–36 per cent, remains relatively unknown on the labour floor and is frequently not recognised or not clinically apparent at the time of delivery.32 33 34 It may result in levator hiatal overdistension in 28 per cent of cases.35 36 37 38 Both forms of LAM injury are associated with POP and its recurrence after a reconstructive surgery.39 40 41 42 Apart from PFD in general and POP, LAM injury is also associated sexual dysfunction,43 44 45 46 47, making its diagnosis essential.
LAM avulsion may be diagnosed clinically by digital palpation at vaginal examination.48 However, this involves a longer learning curve.49 50 In the advent of medical imaging, diagnosis of LAM avulsion may be achieved by a translabial pelvic floor ultrasound (PFUS), endovaginal ultrasound and MRI.51 52 PFUS is the imaging of choice though, as it is more accessible, less costly and more patient friendly.
Obstetric factors and levator trauma
Established risk factors for these traumas include advanced maternal age at first delivery, prolonged second stage of labour, macrosomic infant, episiotomy, major perineal tears and forceps-assisted delivery.53 54 55 56 Elective CS is protective of LAM avulsion. In a series of 157 women on day two to three postpartum PFUS,46 none of the elective CS group had evidence of LAM avulsion (0/55), compared with 38.5 per cent after spontaneous VB (27/70). Levator abnormalities have been reported in exclusive CS; however, they are rare, attributed to inclusion of partial LAM defect or preceding undisclosed vaginal trauma.57
Forceps delivery is a main risk factor for LAM avulsion.58 In a series of 160 primiparous women at nine to 12 months postpartum, a majority of the forceps delivery (66%) sustained identifiable major levator defect on MRI.59 A prospective observational cohort of 367 nulliparous women who were scanned antenatally and at three to four months postnatally, found similar association with forceps delivery on PFUS (OR 3.83, 95% CI 1.34–10.94).60 Our Dunedin 20-year result also confirmed this association (Table 2).
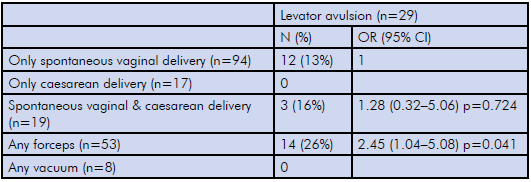
Table 2. Dunedin 20-year follow up – mode of delivery and LAM avulsion. 61
Ventouse delivery, on the other hand, does not appear to be a risk factor. 62 Prolonged second stage of labour is associated with LAM avulsion. One study reported women with LAM avulsion have a 78 minutes longer second stage of labour.63 Another study reported an odds ratio of 2.27 for LAM avulsion with a second stage of less than 110 minutes.64 Fetal head circumference may be an independent risk factor; when head circumference was greater than 35.5 cm, the odds radio for levator injury increased to 3.34.47 In contrast, another study found no association between fetal head circumference and levator injuries.65 66
Early evidence suggests epidural analgesia may be protective of levator hiatal overdistension (OR 0.33, 95% CI 0.12–0.88).67 Increased maternal age at first delivery was found to be associated with levator injury.68 69 The role of maternal BMI remains unclear. Shek et al reported a greater risk for levator injury in women with a lower BMI, but the clinical significance may be questionable as BMI was 27.9 versus 30.70
LAM avulsion and PFD
Avulsion injury is more common in women with underactive pelvic floor muscle strength (PFMS), found in 53.8 per cent, compared to 16.1 per cent with a normal PFMS, in retrospective series of 352 women on PFUS. A similar finding of significant reduction in Oxford grading was associated with avulsion defects in another retrospective series of 1112 women.71
The relationship between urinary incontinence (UI) and levator defects remains controversial. In contrast, the puborectalis component of the LAM seems important in anal continence, likely by maintaining the anorectal angle.72 LAM avulsion appears to be a risk factor for faecal incontinence, particularly later in life,73 thus highlighting the importance of an adequately functioning anal sphincter as well as the suprasphincteric mechanism via LAM.
Perhaps the most established is the relationship between LAM avulsion with POP and POP recurrence after surgery.74 75 LAM appears to double the risk of significant anterior and central compartment prolapse with less effect on the posterior compartment. In a retrospective review of imaging data and examination findings of 781 women at a tertiary urogynaecology centre (mean age 53 years), POP-Q Stage 2 or higher prolapse was found in 150/181 (83%) women with avulsion and in 265/600 (44%) women without avulsion (OR 1.9, 95% CI 1.7–2.1).76 The size of the defect correlates with the symptoms and signs of prolapse.77 A case-control study of 151 women with POP and 135 controls with normal support, DeLancey et al found an adjusted OR of 7.3 for those with major LAM avulsion, but no significant association with minor levator defect.78 This was further supported by Pilzek et al.79
Both short-term operative results and risks of prolapse recurrence (cystocoele), even with mesh use, are worse in women with LAM avulsion.80 Dietz et al demonstrated an objective recurrence rate (Stage 2+) of 40 per cent,81 while Weemhoff et al found an overall objective recurrence rate of 51 per cent with average follow up of 31 months after anterior colporrhaphy.82
Our Dunedin 20-year follow-up cohort confirmed similar findings of LAM avulsion association with objectively measured clinical POP and sonographically determined pelvic organ descent.83
Research on the long-term impact of LAM avulsion on sexual dysfunction is still lacking. Two studies with postpartum follow up in the first year demonstrated worse sexual function outcome in women with LAM avulsion, with fewer of them resuming sexual intercourse within three months postnatally. 84 85
Prediction, prevention and repair
Prediction of LAM injury is difficult, if not impossible.86 87 However, it has been shown that it’s the first birth that does the damage in regards to LAM avulsion, hiatal overdistension and anal sphincter defects. Subsequent births do not seem to have substantial additional effect.88 89 90 Attempts at prevention should be made prior to the first delivery. To this date, no proven prevention strategy has been found. Study on the antenatal use of Epi-No® birth trainer has shown that the device is unlikely to be clinically beneficial in the prevention of intrapartum levator ani, anal sphincter and perineal trauma.91
Previous studies have shown that LAM trauma does not heal.92 A longitudinal study of 488 women found no evidence of regression or healing of changes to levator distensibility.93 Another prospective longitudinal study showed less common appearance of improvement on scan in women with major LAM injury.94 Women with persistent LAM injury at one year follow-up reported more bothersome symptoms, reduced PFMS and enlarged hiatus.95
Surgical repair of LAM avulsion has been described.96 97 A prospective surgical pilot study of mesh reinforcement for levator repair at time of concurrent standard prolapse repair has returned high prolapse recurrence rate in 5/17 women at mean follow up of 1.3 years.,98 Stem cell and extracellular scaffolding technology99 remains a tantalising prospect for future treatment; however, much of this remains in the preclinical research phase and it will likely be many years before mature technology becomes available for clinical application.
It is only a matter of time before the healthcare consumer, medicolegal and professional bodies inevitably converge to demand full antenatal disclosure on the overall risks involved with various delivery modes. Presently we need to actively pursue ongoing research to better understand the long-term functional sequelae, modifiable risk factors and overall burden of these very common pelvic floor injuries. Risk-predicting tools such as the one proposed by UR-CHOICE100 on long-term PFD may foreseeably become a routine utility in empowering expectant women with information to make informed decisions and best prepare them for the tremendous changes to take place in their life, their body and their family.
References
- Lin S, Wilson D. Unintended benefits. O&G Magazine. 2014 Autumn: p. 21-23.
- Wu J, Matthews C, Conover M, Pate V, Jonsson F. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201-6.
- Olsen A, Smith V, Bergstrom J, Colling J, Clark A. Epidmiology of Surgically Managed Pelvc Organ Prolapse and Urinary Incontinence. Obstetrics & Gynecology. 1997;89(4):501-506.
- Boyles S, Weber A, Meyn L. Procedures for pelvic organ prolapse in the United States, 1979-1997. Am J Obstet Gynecol. 2003;188(1).
- Subak L, Waetjen L, van den Eeden S, et al. Cost of pelvic organ prolapse surgery in the United States. Obstet Gynecol. 2001;98(4).
- Kerkhof M, Hendriks L, Brölmann H. Changes in connective tissue in patients with pelvic organ prolapse – a review of the current literature. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(4).
- Jackson S, Avery N, Tarlton J, et al. Changes in metabolism of collagen in genitourinary prolapse. Lancet.1996;347(9016).
- Gyhagen M, Bullarbo M, Nielsen T, Milsom Prevalence and risk factors for pelvic organ prolapse 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG. 2013;120:152-160.
- MacLennan A, Taylor A, Wilson D, Wilson D.The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG. 2000;107(12):1460-70
- Weemhoff M, Shek K, Dietz H. Effects of age on levator function and morphometry of the levator hiatus in women with pelvic floor disorders. Int Urogynecol J.2010;21(9):1137-1142.
- Hendrix S, Clark A, Nygaard I, et al. Pelvic organ prolapse in the Women’s Health Initiative: gravity and gravidity. Am J Obstet Gynecol. 2002;186(6):1160-6.
- Glazener C, Elders A, MacArthur C, et al. Childbirth and prolapse: long-term associations with the symptoms and objective measurement of pelvic organ prolapse. BJOG. 2013;120:161-168.
- Kamisan Atan I, Lin S, Herbison P, et al. Levator avulsion is associated with pelvic organ prolapse 20-30 years after the first birth. In ICS 2015; 2015; Montreal, Canada. p. Podium Short Oral Session.
- Andrews V, Sultan AH, Thakar R, Jones PW. Occult anal sphincter injuries – myth or reality? BJOG. 2006;113(2):195-200.
- Guzman R, Shek K, Langer S, Dietz H. Prevalence of anal sphincter injury in primiparous women. Ultrasound Obstet Gynecol. 2013;42(4):461-466.
- Kamisan Atan I, Lin S, Herbison P, et al. Levator avulsion is associated with pelvic organ prolapse 20-30 years after the first birth. In ICS 2015; 2015; Montreal, Canada. p. Podium Short Oral Session.
- Dietz H, Simpson J. Levator trauma is associated with pelvic organ prolapse. BJOG. 2008;115(8):979-84.
- Gyhagen M, Bullarbo M, Nielsen T, Milsom,I. Prevalence and risk factors for pelvic organ prolapse 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG. 2013;120:152-160.
- Glazener C, Elders A, MacArthur C, et al. Childbirth and prolapse: long-term associations with the symptoms and objective measurement of pelvic organ prolapse. BJOG. 2013;120:161-168.
- Kamisan Atan I, Lin S, Herbison P, et al. Levator avulsion is associated with pelvic organ prolapse 20-30 years after the first birth. In ICS 2015; 2015; Montreal, Canada. p. Podium Short Oral Session.
- Gyhagen M, Bullarbo M, Nielsen T, Milsom I. The prevalence of urinary incontinence 20 years after childbirth: a national cohort. BJOG. 2013;120(2):144- 151.
- ACOG. Safe Prevention of the Primary Cesarean Delivery. Obstetric Care Consensus. March 2014. Number 1. Reaffirmed 2016.
- Rahmanou P, Caudwell-Hall J, Kamisan Atan I, Dietz H. The association between maternal age at first delivery and risk of obstetric trauma. Am J Obstet Gynecol. 2016;215(4).
- Health Mo. New Zealand Maternity Clinical Indicator 2014. 2016. Available from: health.govt.nz.
- Kamisan Atan I, Lin S, Herbison P, et al. Levator avulsion is associated with pelvic organ prolapse 20-30 years after the first birth. In ICS 2015; 2015; Montreal, Canada. p. Podium Short Oral Session.
- Lin S, Kamisan Atan I, Herbison P, et al. Delivery mode, levator avulsion and obstetric anal sphincter injury twenty-years after childbirth. Int Urogynecol J. 2015;26(1(Suppl 1)).
- Freeman R. Can we prevent childbirth-related pelvic floor dysfunction? BJOG. 2013;120:137-140.
- Svabík K, Shek K, Dietz H. How much does the levator hiatus have to stretch during childbirth? BJOG. 2009;116(12):1657-62.
- Schwertner-Tieplmann N, Thakar R, Sultan A, Tunn R. Obstetric levator ani muscle injuries: current status. Ultrasound in Obstet Gynecol. 2012;39(4):372-383.
- Brooks S, Zerba E, Faulkner J. Injury to muscle fibres after single stretches of passive and maximally stimulated muscles in mice. J Physiol. 1995;15(488).
- Dietz HP. Pelvic floor trauma in childbirth. ANZJOG. 2013;53:220-230.
- Andrews V, Sultan AH, Thakar R, Jones PW. Occult anal sphincter injuries – myth or reality? BJOG. 2006;113(2):195-200.
- Guzman R, Shek K, Langer S, Dietz H. Prevalence of anal sphincter injury in primiparous women. Ultrasound Obstet Gynecol. 2013;42(4):461-466.
- Dietz HP. Pelvic floor trauma in childbirth. ANZJOG. 2013;53:220-230.
- Shek K, Dietz H. Can levator avulsion be predicted antenatally. Am J Obstet Gynecol. 2010;202(586):e1-6.
- Dietz H, Lanzarone V. Levator trauma after vaginal delivery. Obstet Gynecol. 2005;106(4).
- Kearney R, Miller J, Ashton-Miller J, DeLancey J. Obstetric factors associated with levator ani muscle injury after vaginal birth. Obstet Gynecol. 2006;107:144-149.
- Dietz H, Steensma A. The prevalence of major abnormalities of the levator ani in urogynaecological patients. BJOG. 2006;113(2):225-30.
- Kamisan Atan I, Lin S, Herbison P, et al. Levator avulsion is associated with pelvic organ prolapse 20-30 years after the first birth. In ICS 2015; 2015; Montreal, Canada. p. Podium Short Oral Session.
- Caudwell-Hall J, Kamisan Atan I, Rojas R, Dietz H. Levator avulsion is associated with prolapse 3–6 months after a first vaginal delivery. Int Urogynecol J. 2015;26 (S148-149).
- Wong V, Shek K, Rane A, et al. Is levator avulsion a predictor of cystocele recurrence following anterior vaginal mesh placement. Ultrasound Obstet Gynecol. 2013;42(2):230-4.
- Model A, Shek K, Dietz H. Levator defects are associated with prolapse after pelvic floor surgery. Eur J Obstet Gynecol Reprod Biol. 2010;153(2):220-3.
- Thibault-Gagnon S, Yusuf S, Langer S, et al. Do women notice the impact of childbirth-related levator trauma on pelvic floor and sexual function? Results of an observational ultrasound study. Int Urogynecol J. 2014;25(10):1389-1398.
- van Delft K, Sultan A, Thakar R, et al. The relationship between postpartum levator ani muscle avulsion and signs and symptoms of pelvic floor dysfunction. BJOG. 2014;121(9):1167-71.
- Signorello L, Harlow B, Chekos A, Repke J. Postpartum sexual functioning and its relationship to perineal trauma: a retrospective cohort study of primiparous women. Am J Obstet Gynecol. 2001; 184(5):881-8.
- Thompson J, Roberts C, Currie M, Ellwood D. Prevalence and persistence of health problems after childbirth: associations with parity and method of birth. Birth. 2002;29(2):83-94.
- Skinner E, Dietz H. Psychological and somatic sequelae of traumatic vaginal delivery: A literature review. ANZJOG. 2015 55(4):309-14.
- van Delft K, Sultan A, Thakar R, et al. Agreement between palpation and transperineal and endovaginal ultrasound in the diagnosis of levator ani avulsion. Int Urogynecol J. 2015;26(1):33-9.
- Kamisan Atan I, Lin S, Herbison P, et al. Assessment of levator avulsion: digital palpation versus tomographic ultrasound imaging. In 2015; Nice, France. p. Non-Discussed Posters – E Poster.
- Dietz H, Shek C. Validity and reproducibility of the digital detection of levator trauma. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(8):1097-101.
- Schwertner-Tieplmann N, Thakar R, Sultan A, Tunn R. Obstetric levator ani muscle injuries: current status. Ultrasound in Obstet Gynecol. 2012;39(4):372-383.
- Dietz HP. Pelvic floor trauma in childbirth. ANZJOG. 2013;53:220-230.
- Shek K, Dietz H. Intrapartum risk factors for levator trauma. BJOG. 2010;117(12).
- Caudwell-Hall J, Kamisan Atan I, Martin A, et al. Intrapartum predictors of pelvic floor trauma. Ultrasound in Obstetrics and Gynecology. 2014;44(Supplement S1).
- Hehir M, O’Connor H, Higgins S, et al. Obstetric anal sphincter injury, risk factors and method of delivery – an 8-year analysis across two tertiary referral centers. J Matern Fetal Neonatal Med. 2013;26(15):1514-6.
- Smith L, Price N, Simonite V, Burns E. Incidence of and risk factors for perineal trauma: a prospective observational study. BMC Pregnancy Childbirth. 2013;13(25).
- Albrich S, Laterza R, Skala C, et al. Impact of mode of delivery on levator morphology: a prospective observational study with three-dimensional ultrasound early in the postpartum period. BJOG. 2011; 119(1):1-11.
- Schwertner-Tieplmann N, Thakar R, Sultan A, Tunn R. Obstetric levator ani muscle injuries: current status. Ultrasound in Obstet Gynecol. 2012;39(4):372-383.
- Kearney R, Miller J, Ashton-Miller J, DeLancey J. Obstetric factors associated with levator ani muscle injury after vaginal birth. Obstet Gynecol. 2006;107:144-149
- Shek K, Dietz H. Intrapartum risk factors for levator trauma. BJOG. 2010;117(12).
- Lin S, Kamisan Atan I, Herbison P, et al. Delivery mode, levator avulsion and obstetric anal sphincter injury twenty-years after childbirth. Int Urogynecol J. 2015;26(1(Suppl 1)).
- Schwertner-Tieplmann N, Thakar R, Sultan A, Tunn R. Obstetric levator ani muscle injuries: current status. Ultrasound in Obstet Gynecol. 2012;39(4):372-383.
- Kearney R, Miller J, Ashton-Miller J, DeLancey J. Obstetric factors associated with levator ani muscle injury after vaginal birth. Obstet Gynecol. 2006;107:144-149.
- Valsky D, Lipschuetz M, Bord A, et al. Fetal head circumference and length of second stage of labor are risk factors for levator ani muscle injury, diagnosed by 3-dimensional transperineal ultrasound in primiparous women. Am J Obstet Gynecol. 2009;201(1):91. e1-7.
- Kearney R, Miller J, Ashton-Miller J, DeLancey J. Obstetric factors associated with levator ani muscle injury after vaginal birth. Obstet Gynecol. 2006;107:144-149.
- Schwertner-Tieplmann N, Thakar R, Sultan A, Tunn R. Obstetric levator ani muscle injuries: current status. Ultrasound in Obstet Gynecol. 2012;39(4):372-383.
- Shek K, Dietz H. Intrapartum risk factors for levator trauma. BJOG. 2010;117(12).
- Rahmanou P, Caudwell-Hall J, Kamisan Atan I, Dietz H. The association between maternal age at first delivery and risk of obstetric trauma. Am J Obstet Gynecol. 2016;215(4).
- Schwertner-Tieplmann N, Thakar R, Sultan A, Tunn R. Obstetric levator ani muscle injuries: current status. Ultrasound in Obstet Gynecol. 2012;39(4):372-383.
- Shek K, Dietz H. Can levator avulsion be predicted antenatally. Am J Obstet Gynecol. 2010;202(586):e1-6.
- Dietz H, Shek C. Levator avulsion and grading of pelvic floor muscle strength. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(5):633-6.
- Lembo A, Camilleri M. Chronic constipation. N Engl J Med. 2003;349(14):1360-8.
- Lewicky-Gaupp C, Brincat C, Yousuf A, et al. Fecal incontinence in older women: are levator ani defects a factor? Am J Obstet Gynecol. 2010;202(491):e1-6.
- Dietz H, Simpson J. Levator trauma is associated with pelvic organ prolapse. BJOG. 2008;115(8):979-84.
- Schwertner-Tieplmann N, Thakar R, Sultan A, Tunn R. Obstetric levator ani muscle injuries: current status. Ultrasound in Obstet Gynecol. 2012;39(4):372-383.
- Dietz H, Simpson J. Levator trauma is associated with pelvic organ prolapse. BJOG. 2008;115(8):979-84.
- Dietz H. Quantification of major morphological abnormalities of the levator ani. Ultrasound Obstet Gynecol. 2007;29(3):329-34.
- DeLancey J, Morgan DM, Fenner D, et al. Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol. 2007;109(2 Pt 1):295-302.
- Pilzek A, Havard L, Guzman Rojas R, Dietz, H. Recurrence after prolapse surgery: does partial avulsion of the levator ani muscle matter? In ICS; 2013; Bacelona, Spain.
- Dietz H. Mesh in prolapse surgery: an imaging perspective. Ultrasound Obstet Gynecol. 2012;40(5):495-503.
- Dietz H, Chantarasorn V, Shek K. Levator avulsion is a risk factor for cystocele recurrence. Ultrasound Obstet Gynecol. 2010;36(1):76-80.
- Weemhoff M, Vergeldt T, Notten K, et al. Avulsion of puborectalis muscle and other risk factors for cystocele recurrence: a 2-year follow-up study. Int Urogynecol J. 2012;23(1):65-71.
- Kamisan Atan I, Lin S, Herbison P, et al. Levator avulsion is associated with pelvic organ prolapse 20-30 years after the first birth. In ICS 2015; 2015; Montreal, Canada. p. Podium Short Oral Session.
- Thibault-Gagnon S, Yusuf S, Langer S, et al. Do women notice the impact of childbirth-related levator trauma on pelvic floor and sexual function? Results of an observational ultrasound study. Int Urogynecol J. 2014;25(10):1389-1398.
- van Delft K, Sultan A, Thakar R, et al. The relationship between postpartum levator ani muscle avulsion and signs and symptoms of pelvic floor dysfunction. BJOG. 2014;121(9):1167-71.
- Shek K, Dietz H. Can levator avulsion be predicted antenatally. Am J Obstet Gynecol. 2010;202(586):e1-6.
- Caudwell-Hall J, Kamisan Atan I, Martin A, et al. Intrapartum predictors of pelvic floor trauma. Ultrasound in Obstetrics and Gynecology. 2014;44(Supplement S1).
- Kamisan Atan I, Lin S, Herbison P, et ak. It’s the First Vaginal Birth That Does Most of the Damage. Int Urogynecol J. 2015;26(Suppl 1).
- Kamisan Atan I, Gerges B, Shek K, Dietz H. The association between vaginal parity and hiatal dimensions: a retrospective observational study in a tertiary urogynaecological centre. BJOG. 2015;122(6):867-72.
- Horak T, Guzman-Rojas R, Shek K, Dietz,H.Pelvic floor trauma: does the second baby matter. Ultrasound Obstet Gynecol. 2014;44(1).
- Kamisan Atan I, Shek K, Langer S, et al. Does the Epi-No birth trainer prevent vaginal birth-related pelvic floor trauma?A multicentre prospective randomised controlled trial. BJOG. 2016;123(6).
- Shek K, Chantarasorn V, Langer S, Dietz H.Does levator trauma ‘heal’? Ultrasound Obstet Gynecol. 2012;40(5):570-575.
- Shek K, Chantarasorn V, Langer S, Dietz H.Does levator trauma ‘heal’? Ultrasound Obstet Gynecol. 2012;40(5):570-575.
- van Delft K, Thakar R, Sultan A, et al. The natural history of levator avulsion one year following childbirth: a prospective study.BJOG. 2015;122(9):1266-73.
- van Delft K, Thakar R, Sultan A, et al. The natural history of levator avulsion one year following childbirth: a prospective study.BJOG. 2015;122(9):1266-73.
- Rostaminia G, Shobeiri SQL. Surgical repair of bilateral levator ani muscles with ultrasound guidance. Int Urogynecol J. 2013;24(7):1237-9.
- Dietz H, Shek K, Daly O, Korda A. Can levator avulsion be repaired surgically? A prospective surgical pilot study. Int Urogynecol J. 2013;24(6):1011-5.
- Dietz H, Shek K, Daly O, Korda A. Can levator avulsion be repaired surgically? A prospective surgical pilot study. Int Urogynecol J. 2013;24(6):1011-5.
- Weiss M, Rao M, Deans R, Czermak P. Manufacturing Cells for Clinical Use. Stem Cells Int. 2016 Jun.
- Wilson D, Dornan J, Milson I, Freeman R. UR-CHOICE: can we provide mothers-to-be with information about the risk of future pelvic floor dysfunction? Int Urogynecol J. 2014;25(11):1449-52.







Leave a Reply