A 46-year-old multiparous woman presented to the emergency department of a large metropolitan hospital that did not have an onsite gynaecology service. She was known to have a fibroid uterus and presented with severe abdominal pain. She was of Vietnamese ethnicity and spoke limited English. On examination, she was found to be pale and hypotensive, with a blood pressure of 60/40mmHg. Her abdomen was distended and generally tender. Resuscitative measures were instituted and a bedside scan was performed, which showed free fluid in the abdomen.
An urgent computed tomography (CT) scan of her abdomen and pelvis confirmed free fluid in all four quadrants, consistent with haemoperitoneum (Figures 1a and b). The known fibroid uterus was noted to have increased in size from 80mm (anterior-posterior) x81mm (transverse) x90mm (craniocaudal) a year ago, to 120x96x160mm. Her initial haemoglobin came back at 90g/dl and she was transfused two units of packed red cells.
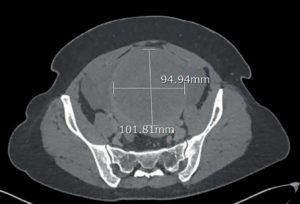
Figure 1a. CT scan. Enlarged fibroid uterus and haemoperitoneum concentrated around the uterus.

Figure 1b. CT scan. Enlarged fibroid uterus.
In view of her hypotensive status, with suspected continuing intra-abdominal bleeding, the on-call gynaecology team from a linked hospital was called in. A midline laparotomy was performed that revealed approximately one litre haemoperitoneum and a 20-week-size fibroid uterus. The source of bleeding was found to be a centimetre-long tear in the uterine serosa at the fundus, with surrounding ectatic blood vessels (Figure 2). A total abdominal hysterectomy was performed without event. Postoperatively, haemoglobin was found to have dropped to 66gm/dl and another two units of packed red cells were transfused. She recovered well and was discharged home on the fourth postoperative day.

Figure 2. Gross pathology specimen of uterus with serosal tear at fundus.
At gross pathological examination, a large fibroid uterus measuring 100mm anterior-posterior, 93mm transverse, 166mm cranio-caudal and weighing 921g was noted. Histopathological examination reported moderate adenomyosis and multiple fibroids, with no features of malignancy.
Discussion
Fibroids are the most common tumours in women. 1However, they are rarely associated with acute life-threatening complications. Haemoperitoneum due to spontaneous bleeding from a fibroid uterus is exceedingly rare with fewer than 100 cases reported in the literature.2
The acute abdomen in a woman with known fibroids raises the possibility of torsion of a pedunculated subserosal fibroid, red degeneration, sarcomatous change or acute haemorrhage. Rupture of, or haemorrhage from, an ovarian cyst or adnexal torsion needs to be considered. A ruptured ectopic pregnancy is the most important differential in any woman of childbearing age and needs exclusion.
In this case, a CT scan confirmed a large haemoperitoneum and suspected haemorrhage from the fibroid uterus as blood seemed to be concentrated around the uterus. No evidence of active bleeding was evident on CT scan, despite use of multiphased intravenous contrast.
The possibility of bleeding from sources outside the genital tract was taken into consideration while planning her laparotomy. Similar to previous reports, the source of bleeding in our patient was from blood vessels overlying the fibroid. It has been postulated that rupture of serosal veins over a fibroid uterus can occur due to increase in intra-abdominal pressure, rapid increase in size of fibroid or pelvic congestion due to menstruation or pregnancy.3 Most reports of haemoperitoneum due to bleeding fibroid uterus are in women in the reproductive age group.4
Management considerations should include future fertility plans. Some cases have been successfully managed with myomectomy.5 Uterine artery embolisation has also been used to avoid an emergency hysterectomy.6 Where future childbearing is not a consideration or in case of a multi-fibroid uterus, hysterectomy is often the best option. Our decision to perform a total abdominal hysterectomy for our patient took into consideration her perimenopausal status and the possibility of a sarcomatous change in the fibroid.
Conclusion
In the practice of medicine, to be aware is to be prepared. This case highlights an uncommon, yet potentially catastrophic, complication of a common condition.
References
- Lumsden MA, Hamoodi I, Gupta J, et al.
Fibroids: diagnosis and management. BMJ.2015;351:h4887. - Gupta S, Manyonda IT. Acute complications of fibroids. Best Pract Res Clin Obstet Gynaecol. 2009;23(5):609-17.
- Gupta S, Manyonda IT. Acute complications of fibroids. Best Pract Res Clin Obstet Gynaecol. 2009;23(5):609-17.
- Gupta S, Manyonda IT. Acute complications of fibroids. Best Pract Res Clin Obstet Gynaecol. 2009;23(5):609-17.
- Gulati N, Raman S, Srinivasan M, Bakour S. Rare gynaecological emergency: massive intraperitoneal haemorrhage from spontaneous rupture of a superficial vessel
on a large leiomyoma. BMJ Case Rep. 2016;2016. doi: 10.1136/bcr-2015-212576. - Fontarensky M, Cassagnes L, Bouchet P, et al. Acute complications of benign uterine leiomyomas: treatment of intraperitoneal haemorrhage by embolisation of the uterine arteries. Diagn Interv Imaging. 2013;94(9):885-90.





Leave a Reply