Progressive increases in life expectancy have resulted in a steady climb in low trauma fractures among the elderly. Fracture risk can be estimated from clinical risk factors and bone density, and a formal assessment is indicated in most women in their early 60s, earlier in those with specific risk factors. A 10-year hip fracture risk of more than 3 per cent is an arbitrary, but widely used, threshold for pharmaceutical intervention. Bisphosphonates remain the most widely used pharmaceuticals, with denosumab, teriparatide and agents acting on the oestrogen receptor also having roles. Calcium requirements can usually be met from a balanced diet, but low-dose vitamin D replacement is important for osteomalacia prevention in those with inadequate sunlight exposure (for example, the frail elderly). Maintaining BMI higher than 20 is an important community-wide measure for fracture prevention, along with smoking cessation and regular safe exercise.
Bone loss is an inevitable consequence of living past middle age and, in women, is substantially dependent on the lower circulating oestrogen level postmenopause; postmenopausal bone loss can be deferred indefinitely by the use of oestrogen replacement. Low oestrogen levels lead to increases in osteoclast numbers and activity, resulting in a sustained excess of bone resorption over bone formation. The consequent fall in bone mass is mirrored by a progressive rise in fracture risk, resulting in more than 50 per cent of postmenopausal women having a fracture of some sort between menopause and death. Forearm and hip fractures occur in about 20 per cent of older women and vertebral deformities progressively increase with age, affecting more than two-thirds of women in their 80s. Individuals of Polynesian or African descent have higher bone density and lower fracture risk than those of European or Asian ancestry. Since not all postmenopausal women fracture, the first task in osteoporosis management is to assess fracture risk so that interventions can be targeted to those most likely to benefit.
Osteoporosis risk assessment
The last three decades have seen an evolution in our operational definition of osteoporosis. Prior to the advent of bone densitometry, osteoporosis was defined as the occurrence of fractures after minimal trauma. In the 1990s, it was redefined in terms of bone density (a value more than 2.5 standard deviations below the young normal mean). More recent epidemiology studies have indicated that, while bone density is an important risk factor, clinical risk factors (such as age, weight, personal and family history of fractures, smoking, glucocorticoid use, falls) are also important. This has resulted in the development of fracture risk calculators that facilitate the integration of all risk factors to produce a global assessment of risk. FRAX is probably the most widely used calculator, but the Garvan calculator appears to be better calibrated for Australasian populations and has the important advantage of incorporating recent falls history as a risk factor. In patients with borderline fracture risk, using both calculators can optimise fracture prediction.
Cost-effectiveness analyses have suggested that a 10-year risk of hip fracture of about 3 per cent, or of major osteoporotic fracture of 15−20 per cent, are appropriate thresholds for intervention. This is dependent on the cost of interventions − a lower threshold is cost-effective when using generic medications, but a much higher threshold should apply to expensive interventions such as teriparatide. Hip fracture risk in women doubles every six years, which guides intervals between assessments in women not taking anti-osteoporotic medication.
Non-pharmacological interventions
Some interventions can be advocated across the population because of their low cost and their contribution to both skeletal and non-skeletal health. These interventions include underweight avoidance (hip fracture risk increases steeply when BMI is less than 20), not smoking, moderating alcohol intake and remaining physically active. In the frail elderly, falls prevention is particularly important and may entail removal of fall hazards, optimisation of vision correction, minimisation of sedative use and appropriately designed exercise programs. Hip protectors may have some value in frequent fallers, but the evidence is mixed.
Pharmacological interventions
Pharmacological interventions that have been demonstrated to be safe and effective should be targeted to individuals according to their fracture risk. Figure 1 provides an overview of the anti-fracture efficacy of available therapies.
Calcium supplements
There is scant evidence that calcium intake influences fracture risk,1 and it is not included in any of the major fracture risk calculators. Supplements modestly reduce bone turnover, resulting in a non-cumulative bone density benefit of about 1 per cent.2 In the major community-based studies published in the last decade, this has not translated into a fracture reduction, and there is even some suggestion that calcium may increase hip fracture risk. In contrast, the use of calcium plus vitamin D in frail elderly women with severe vitamin D deficiency has been shown to reduce fracture risk, probably representing the efficacy of treating subclinical osteomalacia. Possibly, a similar effect could be achieved with a balanced diet and vitamin D supplementation, but this has not been formally assessed. Calcium supplements commonly cause gastrointestinal side effects, increase the risk of kidney stones and may increase cardiovascular risk, though this remains subject to controversy. In the absence of evidence of fracture prevention, there seems to be little indication for their general use in the postmenopausal population.
Vitamin D
Vitamin D is a substrate, manufactured in the skin with ultraviolet light exposure, for an endocrine system that regulates intestinal calcium absorption. Tissue-specific knockout studies of the vitamin D receptor (VDR) indicate that it has no clinically significant direct effects on bone and that the presence of VDR in the gut is both necessary and adequate for normal skeletal mineralisation. Indeed, high levels of vitamin D metabolites can increase bone resorption, some studies demonstrating increases in the risks of fractures and falls with high vitamin D doses.3
Severe vitamin D deficiency (less than 20nmol/L) results in osteomalacia. Therefore, in those not receiving regular sunlight exposure (for example, frail elderly, veiled women, or those with dark skin living at high latitudes), supplementation with 400IU/day is a sensible measure for osteomalacia prevention. Vitamin D supplements in populations with levels greater than 40nmol/L have not been shown to increase bone density or reduce fracture risk.4 Vitamin D is not a tonic for bone, but it is critical for normal bone mineralisation and osteomalacia prevention.
Bisphosphonates
Bisphosphonates are the most widely used agents for osteoporosis management. They bind avidly to bone surfaces where they potently inhibit the activity of bone-resorbing osteoclasts. Whether administered orally or intravenously, their efficacy is comparable, reducing vertebral fractures by 50–70 per cent, hip fractures by about 40 per cent and total fracture numbers by one-quarter. Their long residence time in bone permits intermittent administration. Tablets are typically given weekly and may cause gastrointestinal intolerance in 20–30 per cent of individuals. Intravenous amino-bisphosphonates can be given as infrequently as every one to two years. On first administration of intravenous bisphosphonates, about 30 per cent of people develop a flu-like illness, typically mild and lasting only a day or two. Intravenous bisphosphonates are contraindicated in patients with renal failure (GFR less than 35ml/min), and these drugs can precipitate symptomatic hypocalcaemia if given to patients with severe vitamin D deficiency.
There are two other safety concerns often raised with bisphosphonate use. Intravenous bisphosphonates, when dosed monthly in patients with metastatic cancer, sometimes impair healing of tooth extraction sites, resulting in necrotic infected lesions referred to as osteonecrosis of the jaw (ONJ). While clearly a problem in cancer patients, there is little evidence that the frequency of this problem is increased in osteoporosis patients receiving bisphosphonates, when compared with osteoporosis patients not receiving bisphosphonates. The adverse event of greater concern is the occurrence of atypical femoral fractures. These lesions develop initially as stress fractures in the lateral cortex of the femoral shaft, which sometimes progress to full transverse fractures. They are not unique to bisphosphonate users but appear to increase in frequency with duration of use of oral bisphosphonates, particularly alendronate. Their frequency appears to reduce rapidly following discontinuation of bisphosphonates.5 For this reason, drug holidays of 6–24 months are frequently instituted in patients whose underlying fracture risk requires treatment for more than five years with these agents. Most studies indicate that if bisphosphonates are targeted to those with elevated fracture risk, the number of fractures prevented will almost always greatly outweigh the small absolute risk of atypical femoral fractures.6
Oestrogens and selective oestrogen receptor modulators
Oestrogen prevents postmenopausal bone loss and fractures, and its introduction late in postmenopausal life results in a 24 per cent decrease in total fracture numbers.7 Its non-skeletal effects (cardiovascular, breast) have greatly reduced its use outside the decade immediately after menopause. Some selective oestrogen receptor modulators (SERMs) are, like oestrogen, inhibitors of bone resorption, and have been shown to reduce vertebral fracture risk, but not the risk of non-vertebral fractures and hip fractures. This limitation greatly reduces their utility in osteoporosis management.
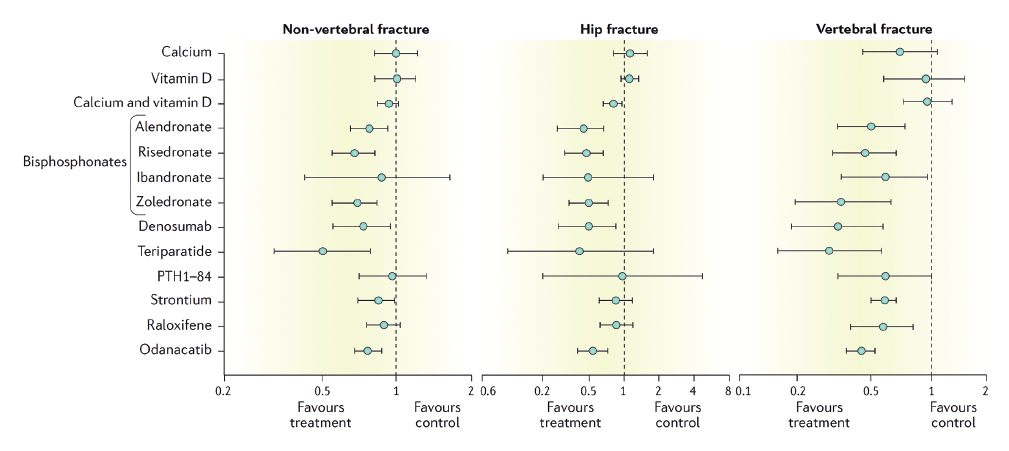
Figure 1. Summary of trial data documenting the efficacy of treatments for the prevention of fractures. Data for strontium, odanacatib and parathyroid hormone (PTH) 1–84 are relative risks, other data are odds ratios. Results are shown with 95 per cent confidence intervals. From Eastell et al, used with permission.
Denosumab
Denosumab is a monoclonal antibody targeted at the principal regulator of osteoclastogenesis. It is administered as six-monthly subcutaneous injections. It profoundly inhibits bone resorption and produces anti-fracture effects comparable to those of intravenous zoledronate. The incidences of ONJ and of atypical femoral fractures with denosumab appear to be comparable to those with bisphosphonates. In contrast to the bisphosphonates, cessation of denosumab results in a rapid increase in bone resorption, resulting in bone loss and increased fracture risk in the first six months after a denosumab injection is missed. Therefore, it is probably preferable to transition denosumab-treated patients on to a bisphosphonate, if denosumab needs to be discontinued.
Anabolic agents
Teriparatide is a fragment of parathyroid hormone and stimulates both bone formation and bone resorption, the former predominating when it is given as daily injections. Its anti-fracture efficacy is broadly comparable to that of the potent bisphosphonates. Newer, related analogues, such as abaloparatide, are currently in clinical development. A new family of anabolic treatments that act by blocking the inhibitory actions on osteoblasts of the osteocyte protein, sclerostin, is under development, of which romosozumab is the furthest advanced.
Conclusions
With the ageing of our population, the number of older postmenopausal women has substantially increased and so have fracture numbers. Therefore, fracture risk assessment in the 60s is now a routine part of the care of postmenopausal women, with the provision of lifestyle advice (weight maintenance, smoking cessation, regular safe exercise) to all, and the targeting of pharmaceuticals to those at higher risk. Maintenance of serum 25-hydroxyvitamin D greater than 40nmol/L is important for osteomalacia prevention so vitamin D supplements have an important role in the frail elderly.
References
- Bolland MJ, Leung W, Tai V, et al. Calcium intake and risk of fracture: systematic review. BMJ. 2015;351:h4580.
- Tai V, Leung W, Grey A, Reid IR, Bolland MJ. Calcium intake and bone mineral density: systematic review and meta-analysis. BMJ. 2015;351:h4183.
- Reid IR, Bolland MJ. Skeletal and nonskeletal effects of vitamin D: is vitamin D a tonic for bone and other tissues? Osteoporos Int. 2014;25:2347-2357.
- Reid IR, Bolland MJ, Grey A. Effects of vitamin D supplements on bone mineral density: a systematic review and meta-analysis. Lancet. 2014;383:146-155.
- Schilcher J, Michaelsson K, Aspenberg P. Bisphosphonate Use and Atypical Fractures of the Femoral Shaft. N Engl J Med. 2011;364:1728-1737.
- Abrahamsen B, Eiken P, Prieto-Alhambra D, Eastell R. Risk of hip, subtrochanteric, and femoral shaft fractures among mid and long term users of alendronate: nationwide cohort and nested case-control study. BMJ. 2016;353:i3365. dx.doi.org/3310.1136/bmj.i3365.
- Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women – Principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.





Leave a Reply