Advanced Life Support in Obstetrics (ALSO) is a multidisciplinary, maternity emergency course first introduced in Australia in 2001, managed by a not-for-profit organisation, Advanced Maternal and Reproductive Education (AMaRE). ALSO provides a safe and supportive environment for clinicians to learn advanced skills in the management of maternity emergencies, learning with other disciplines. Such multidisciplinary or interprofessional education is an effective way to promote teamwork and collaborative practice, both of which are essential for effective patient care and reducing risks in the complex environment of health services.1 Many hospitals across Australia are targeting maternity education strategies towards team training for maternity emergencies in order to improve the quality of care provided to women and newborns.
It has been shown that ordinarily, without targeted training, health professionals do not collaborate well together and learning together in a safe and supportive environment offers a possible way to improve collaboration and patient care.2 Working together effectively often means breaking down traditional hierarchies, and training together is one useful way to achieve team engagement and functionality.3 Learning together also helps effective collaboration and teamwork.4 5 6 ALSO provides this opportunity for doctors, midwives and other relevant healthcare professionals within a team outside of the hospital setting, and without the pressures of the clinical environment. In order for team training to be effective, clinicians also need to feel confident in the application of the required clinical skills to actually manage the emergency. ALSO teaches a systematic way to clinically manage a number of maternity emergencies, promoting a consistent and structured clinical approach to management through the use of easy-to-remember mnemonics.
Research undertaken in Australia demonstrated that completion of the original Australian ALSO course had a positive effect on the confidence and perceived knowledge of doctors and midwives to manage maternity emergencies. 7
In 2014, AMaRE introduced a new course for early maternity trainees, Preparation in Maternity Safety (PIMS), now known as ALSO Part 1. ALSO Part 1 supports beginning practitioners (medical students or interns interested in obstetrics; PGY1 trainees, midwifery students, first year midwifery graduates) by providing supported hands-on learning in a team environment. PIMS uses simulation mannequins and skilled instructors to teach:
- Abdominal palpation, learning the skills to identify presentations and positions and how these relate to gestation and labour progress
- Vaginal examination and how to identify the station, position and cervical dilation as anticipated throughout the various stages
of labour - Speculum examinations for visualisation of
the cervix, identification of liquor, how to collect specimens and performance of cervical smear testing - Alternative birthing positions that support and facilitate normal birth
- Recognition and early management of hypertension in pregnancy with an aim of early identification and escalation
- Discussions regarding the early identification and management of maternal sepsis
- Practical maternal resuscitation using the defibrillator and learning teamwork and communication skills to manage the emergency
- Neonatal resuscitation skills and training to identify those babies requiring more advanced resuscitation skills, using both bag and mask and CPAP resuscitation
- Postpartum haemorrhage (PPH) management using a team approach to prevent, evaluate and manage a PPH
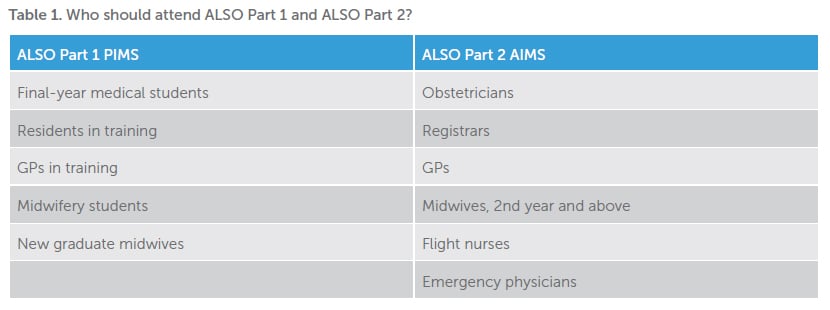
ALSO Part 1 is devised to be first-stage training in maternity emergency care with a risk identification and preventative approach to the management of maternity emergencies.
In 2018, AMaRE will be launching ALSO Part 2, an updated second-stage maternity emergency course Advancing In Maternity Safety (AIMS). ALSO Part 2 will provide education for those situations where early identification and prevention have proved unsuccessful and a team of maternity clinicians need to come together to manage the emergency. ALSO Part 2 will provide a team-based management approach for experienced maternity clinicians to use simulation equipment to manage maternity emergencies. The course will include:
- Facilitating forceps and vacuum birth and identifying the appropriate timing for use
- Managing PPH, including advanced approaches such as balloon tamponade, bimanual compression and new drug managements
- Managing shoulder dystocia, including axial traction and Zavanelli manoeuvre
- Resuscitating women after eclampsia, maternal collapse, emboli and aneurysm
- Assessing fetal welfare, including growth restriction, placental insufficiency, recognition and management of abnormal fetal heart rate patterns
- Case discussion of severe sepsis
- Labour care for challenging labour and birth cases with a team approach to management and clinical decision-making
If you are beginning your career as a maternity care provider ALSO Part 1 (PIMS) offers the opportunity to perform hands-on practice in a simulated, well-supported environment. For the more experienced practitioner (PGY2 and above), ALSO Part 2 (AIMS) will bring together a team of clinicians to manage extreme maternity emergencies within the simulated environment. ALSO Part 1 has been approved for 16 PD points in the Clinical Expertise category, in the RANZCOG CPD Program.
Registration and further information on both the ALSO Stage1 (PIMS) and ALSO Stage2 (AIMS) are available on the AMaRE website, www.amare.org.au.
References
- Barr H, Koppel I, Reeves S, et al. Effective Interprofessional Education: Argument, assumption and Evidence. 2005. Blackwell Publishing, Oxford.
- Lees A, Meyer E. Theoretically speaking: use of a communities of practice framework to describe and evaluate interprofessional education. Journal of Interprofessional Care. 2011;25(2):84-90.
- Reeves S, Zwarenstein M, Goldman J, et al. Interprofessional education: effects on professional practice and health care outcomes. Cochrane Database Systematic Reviews. 2008;1:CD002213.
- Lees A, Meyer E. Theoretically speaking: use of a communities of practice framework to describe and evaluate interprofessional education. Journal of Interprofessional Care. 2011;25(2):84-90.
- Baker L, Egan-Lee E, Martimianakis MA, Reeves S. Relationships of power: implications for interprofessional education. Journal of Interprofessional Care. 2011;25(2):98-104..
- Whitehead C. The doctor dilemma in interprofessional education and care: how and why will physicians collaborate? Medical Education. 2007;41(10):1010-6.
- Walker L, Fetherston C, McMurray A. Perceptions of interprofessional education in the Australian Advanced Life Support in Obstetrics (ALSO) course. Family Medicine. 2015;47(6):435-44.






Leave a Reply