In a well-regarded textbook published in 1925, the London obstetrician Aleck William Bourne described the methods used at the time to diagnose early pregnancy.1 Only vaginal examination was thought to be reliable: bimanual palpation of the uterus was used to detect enlargement and also Hegar’s sign – softening of the lower segment while the fundus and cervix remained firm. Added to this was speculum examination of the cervix to demonstrate a bluish colour, owing to the increased vascularity of that organ. External signs helped, such as increased skin pigmentation, especially the linea nigra running vertically below the umbilicus (in Caucasian women), and darkening of the nipples and the development of Montgomery’s follicles. Symptoms such as amenorrhoea, nausea and vomiting, breast tenderness and food cravings were confirmatory. This had all been the standard teaching for medical students for decades when Bourne published his book.
But change was in the air. In 1928, German gynaecologists Aschheim and Zondek discovered ‘a luteininsing gonadotrophic hormone’ in the urine of pregnant women. Though the hormone itself, ß-human chorionic gonadotrophin (ßhCG), would not be isolated until the 1950s, they postulated that detection of this substance in the urine of a woman with just a few weeks of amenorrhoea might provide a definite diagnosis of pregnancy. They were right, and together they developed the Aschheim-Zondek test, using immature female mice. The test was as follows:
‘Five mice 3–4 weeks old and weighing 5–8 grams each are injected subcutaneously twice daily for three days with slightly acidified morning urine in the following amounts:
- Mouse 1 0.2ml at each injection
- Mouse 2 0.25ml “ “
- Mouse 3 0.3ml “ “
- Mouse 4 0.3ml “ “
- Mouse 5 0.4ml “ “
‘One hundred hours after the first injection the mice are killed and the ovaries inspected. The presence of one blood point easily visible to the naked eye or with a hand lens and about the size of the head of a small pin is diagnostic of pregnancy and the test is 99 per cent accurate.2 3 This was certainly progress, but still a long way off a simple strip from the chemist showing one or two blue lines in the privacy of a woman’s own bathroom.
Soon after the discoveries of Aschheim and Zondek, Friedman and Lapham at the University of Pennsylvania experimented with and developed a test using ‘virgin female rabbits’ aged 12 weeks or more.4 What ultimately became known as Friedman’s Test required that the woman had missed a period by at least seven days. Friedman wrote that the test depended on the presence of large amounts of ‘a gonadotrophic substance in the urine, both follicle-stimulating and luteinising’ and early morning urine was most likely to have higher concentrations of this substance. One of the authors (CdC) remembers how, as a medical student in Dublin, it was common to see women furtively clutching jars of urine wrapped in brown paper approaching doctors’ surgeries just before 9am – there was always a table just inside the foyer of every surgery where the specimen could be discreetly placed. Later that morning the urine was injected into the ear vein of a rabbit; after 36 hours the rabbit was killed and the ovaries examined. Haemorrhage into follicles or the development of corpora lutea were diagnostic of pregnancy5 For many years ‘the rabbit died’ was a euphemism for saying that a woman was pregnant, despite the fact that the rabbit died regardless of whether the test was positive or negative.
In 2016 Louis Tuttle, biochemist at Cairns Base Hospital from the 1950s through to the 1980s, explained to one of the authors (TK) how pregnancy testing developed in Cairns over that time. Louis and his colleague Bill Horsfall initially used the standard test involving female rabbits. The rabbits had to be bred and maintained so that they were ready for immediate testing and this took place in a large Queenslander on what is now the oval of Cairns High School, behind the original Cairns hospital. As the rabbits could only be used once, an ongoing supply was required (and rumours that the rabbits subsequently ended up in rabbit stew are probably correct; rabbit was a dietary staple in rural Australia at the time). The constant demand for rabbits led Louis and Bill to become interested in the possibility of using frogs or toads instead.
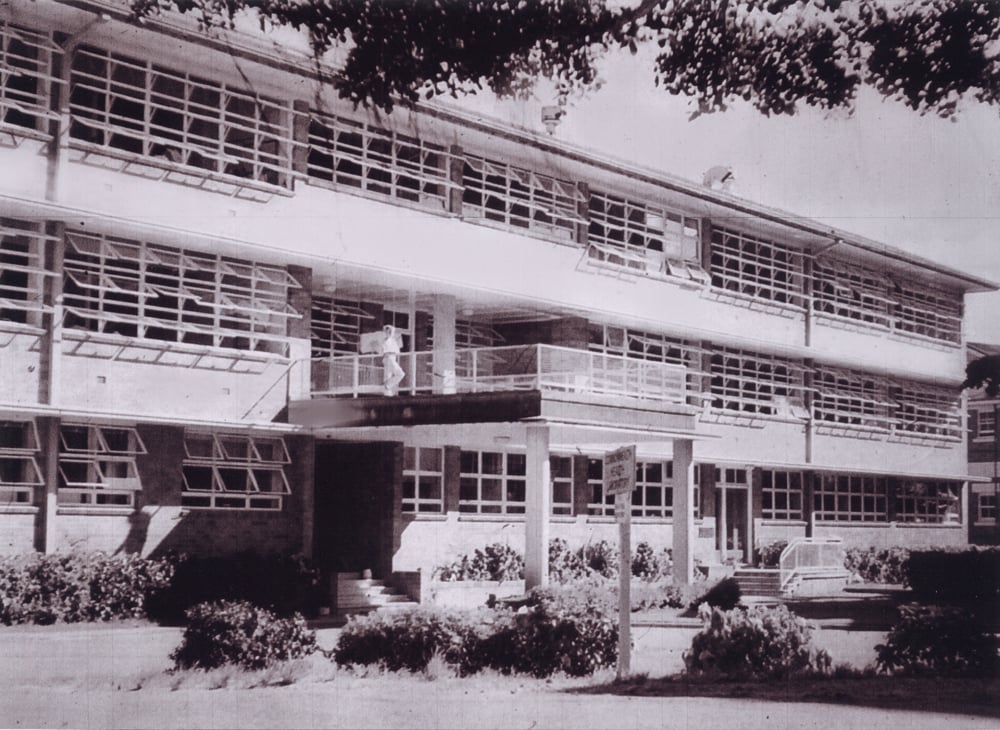
Figure 1. Cairns Base Hospital, 1955.
Female toads had first been used for pregnancy testing by Hogben in 1930. With Hogben’s method, the toads (specifically Xenopus laevis, the South African clawed toad), which were kept in water tanks at around 25°C separated from any male toads, were well fed on lean minced horsemeat until they reached a weight of 60–100g. Toads were less likely than mice to die before they could be used for testing and, unlike both mice and rabbits, they did not need to be killed and so could be used many times, provided they were given a few days rest and kept apart from male toads.6
The woman’s urine was injected into the dorsal lymph sac or the peritoneal cavity of the toad and 24 hours later, secretions were obtained from the cloaca and examined – even with the naked eye numerous black and white eggs 2mm in diameter could be seen. If the test proved negative it was repeated at least once with another toad.
A further refinement was the male toad test developed by Gailli-Mainini in 1947. In this test, 2ml of ‘clean morning urine’ was injected into the dorsal lymph sac of the male toad. Just 3–5 hours later a pipette was used to draw up secretions from the cloaca, which were then examined microscopically. If sperm were present, the test was positive. Gailli-Mainini stated that the toads required 10 days rest (segregated from female toads) and feeding on ‘worms and cockroaches, although they could be starved for quite long periods’ and they could be used many times.7 It was the male toad test that was ultimately used in the Cairns pathology department.
By the early 1950s, Cairns had an abundance of cane toads (Bufo marinus); the cane toad, a native of South and Central America, had been introduced to Australia in 1935 by the Bureau of Sugar Experiment Stations, now Sugar Research Australia, in an attempt to control sugar cane beetles. Louis and Bill decided to try using the male cane toads. They advertised their need for toads to the schoolboys of Cairns and received an enthusiastic response; initially they paid sixpence per toad but later this was raised to one shilling.
The male toads were kept isolated from any female toads for 2–3 weeks before being used for testing. This was found to be long enough for sperm production to cease in Bufo marinus. The patient delivered her early morning sample of urine direct to the lab by 9am. It was then spun down and approximately one-eighth of the sample mixed with pure alcohol. This was injected into the back of a male cane toad around 9.30am. The toads were then checked at 3pm and by 5pm a definite result would be obtained. In fact, Louis Tuttle stated that where pregnancy was more advanced and ßhCG levels higher, the result was clearly positive within an hour.
The male cane toad test for pregnancy proved so successful that a distribution network was established from the Cairns Hospital pathology department to other labs around the country. Special wooden boxes lined with straw were constructed; these housed up to a dozen toads that were transported out to Cairns airport for the regular 6.30pm flight south to Brisbane and then to destinations in hospital labs across Australia. It is worth noting that many of us now in the retiring generation of specialist obstetricians probably had the fact of our existence first communicated to our mothers thanks to the services of one of these laboratory toads!

Figure 2. Bill Horsfall and Louis Tuttle, Cairns Base Pathology Lab, 1955.
An immunological test for pregnancy was first described by Wide and Gemzell, in 1960, and several subsequent researchers demonstrated the accuracy of their method, which was a latex aggutination-inhibition slide test for ßhCG that could be read in three minutes and required no sacrifice of small animals.8 9 10 This, of course, is the basis for the much less interesting, but freely available and very accurate, measure of ßhCG in the urine that is the basis of the commercial strip pregnancy test so widely used today.
References
- Bourne A. Synopsis of Midwifery and Gynaecology. Bristol: John Wright and Sons, 1925.
- Finkel HS. The diagnosis of pregnancy by the Aschheim-Zondek test. NEJM. 1931;204:203-9.
- Adair FE ed. Obstetrics and Gynecology. Philadelphia: Lea and Febiger, 1940, vol i, p.246.
- Claye A, Bourne A eds. British Obstetric Practice. London: Heinemann, 1963, p.103-6.
- McNeile LC, Reynolds PA. The Friedman Test for Pregnancy. Cal West Med. 1933;38(1):4-8.
- Claye A, Bourne A eds. British Obstetric Practice. London: Heinemann, 1963, p.103-6.
- Claye A, Bourne A eds. British Obstetric Practice. London: Heinemann, 1963, p.103-6.
- Wide L, Gemzell CA. An immunological pregnancy test. Acta Endocrinol. 1960;35:261-7.
- Henry JB, Little W. Immunological Test for Pregnancy. JAMA. 1962;182(3):230-33.
- Waynforth HB, Jones H, Miller AL. Accuracy of an immunological test for the diagnosis of pregnancy, Lancet. 1964;1(7327):242-3.







Very interesting. I knew about the pregnancy testing, but not that Lou and Bill [my father] had developed it. BTW, the lab was a Commonwealth Health Laboratory, not a State one – even when they moved to the ground floor of the building in the article, on the Esplanade; upper floors were the TB wards.
I just wanted to know – what was the advantage of the rabbit test over the mouse test? I would imagine that mice would be more economical.
Thanks.