From humble beginnings using hessian dolls to practise delivery, simulation is now widely used in obstetrics and gynaecology. The applications of simulation are diverse, and perhaps simulation can be viewed as the Swiss Army knife of an educator’s tool kit. It is useful for training in procedural and teamwork skills, testing systems and processes, and enabling cultural change. However, keeping with the analogy, not every task requires a highly engineered and somewhat expensive 12-prong tool, there are potential dangers with misuse, and even the best Swiss Army knife can’t clear a forest. This article aims to provide a practical overview of the capabilities and effectiveness of simulation for improving care in obstetric emergencies.
Simulation for training procedural skills
Since Madame Du Coudray travelled the French countryside, obstetric providers have recognised the need for simulation training for obstetric procedures. In this regard, obstetrics (or, more correctly, midwifery) was well ahead of the rest of medicine. More than 200 years later, simulation training in obstetric manoeuvres continues to be of benefit with decreased rates of brachial plexus injury (BPI) in shoulder dystocia1 and, more recently demonstrated, reduction in severe perineal trauma with forceps births.2 Other obstetric procedures for less frequently performed manoeuvres, such as complicated vaginal breech, internal podalic version, management of uterine inversion and dis-impaction of fetal head at caesarean, are likely to benefit from simulation training. Improvements in objective patient outcome will prove difficult to demonstrate for these rarer events, but training in these procedures (for which appropriate simulation models are available) should be encouraged.
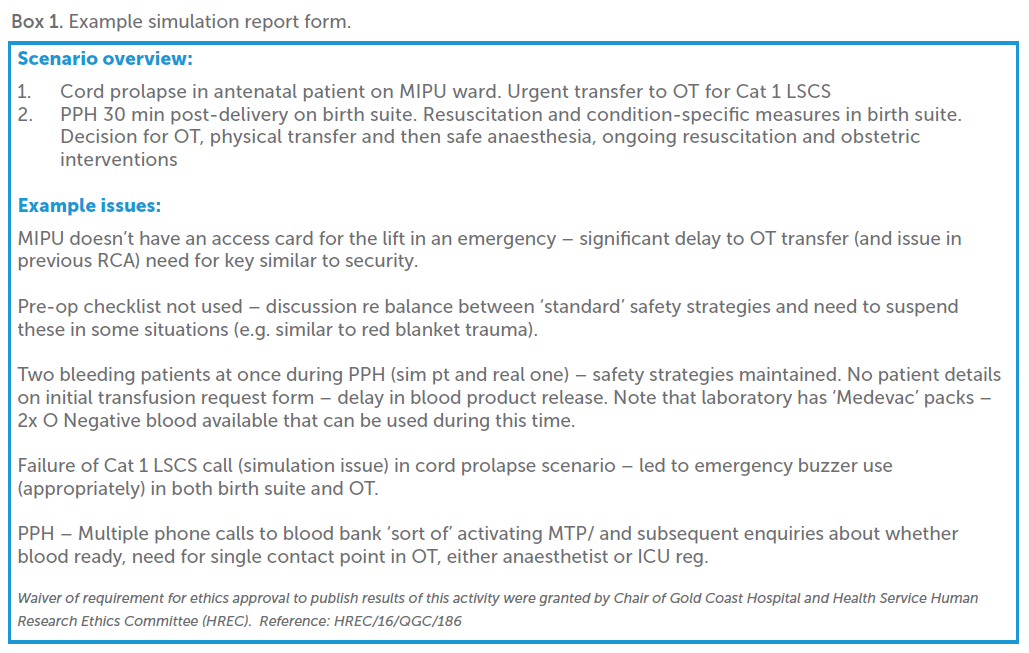

Figure 1. In situ simulation for systems and teams at Gold Coast University Hospital.
Obstetric simulators are becoming more technologically advanced, with newer devices incorporating virtual reality (VR) technology to provide objective feedback.3 Others in development are ‘delivering’ a total VR experience (for example, www.suzannebakkum.com/birthplay). The marginal benefits in laparoscopic simulation of VR over lower fidelity (and less expensive) simulation would suggest that the role of newer technologies should be delineated further prior to widespread adoption. Whatever the simulator or the task, curricula using simulation training for technical skills should be mindful to avoid simple substitution of ‘see one, do one, teach one’ to ‘sim one, do one, teach one’, which may add little to the learner’s expertise. Simulation training provides the opportunity for deliberate practice – defining progressive goals specific to the level of skill, immediate and specific feedback, and lots of repetition. When simulation training for procedural skills has been integrated into a Mastery Learning program, both the learning and clinical outcomes are superior to traditional medical training.4
Simulation for training teams
Technical skills, whether obtained in a simulation lab or on the job, are just one part of safe outcomes for patients. The recognition that a lack of effective teamwork and communication results in adverse outcomes has led to the introduction of simulation-based teamwork training courses across a variety of clinical environments and specialties.5 Maternity teams that demonstrate effective leadership, communication (specifically, use of closed-loop communication) and situational awareness perform better clinically than teams who lack these skills.6 Unlike procedural skills, we understand less about how we learn (and therefore how to teach) leadership and teamwork skills. What exactly ideal maternity teamwork and leadership looks like, and how to teach it most effectively, is an area for ongoing investigation. Despite this lack of understanding, simulation training in teams can improve outcomes in obstetrics. It is how these benefits accrue that is less clear, as there is literature demonstrating minimal impact of simulation training on some behaviours, for example, closed-loop communication.7 It may be that the clinical benefits seen following multidisciplinary training may not be wholly attributed to gains in technical or teamwork skills of the individuals, but rather the shared training experience.
Simulation for testing systems and processes
Even with highly trained individuals and teams, measurable improvements in clinical outcomes have been challenging to consistently demonstrate following simulation training.8 Ad hoc teams, unfamiliar equipment and environments, and institutional policies and procedures may be barriers to improving individual, team and system performance. In situ simulation provides a diagnostic modality by which latent threats and other workplace-specific issues/barriers to individual and team performance can be identified, including equipment issues, checklists, communication processes and ergonomics of clinical areas.9
Simulation educators can target specific areas for improvement (for example, decision-to-delivery interval, transfusion in postpartum haemorrhage [PPH]) with highly authentic scenarios that require participants to perform in their usual environments. Target outcomes should be informed by institutional quality and safety data and/or clinical audits, and educators are wise to rein in the temptation to only simulate exciting (or even outlandish) scenarios fuelled by their passion for simulation.
Processes for documentation, for example, a ‘simulation report form’ of the identified (and rectified) latent hazards, should be in place as this information is useful to demonstrate the contribution of simulation to patient safety when clinical outcomes are harder to quantify. Interdepartmental simulations involving midwifery, obstetrics, anaesthesia, OT and blood bank conducted at one institution identified a range of process issues related to communication, notification and departmental interfaces in time-critical emergencies (PPH and cord prolapse) (Figure 1).
Simulation also allows for testing and refining of new equipment, environments, processes and procedures prior to implementation. It is important to ensure involvement from all potential staff (including administrators, lab staff, porters) that may be involved in the final product or process.
Simulation for culture change
Institutional culture and departmental tribalism10 11 can also be barriers to improving individual, team and system performance in obstetric care. A maternity emergency always involves more than one discipline, each bringing their own perspectives and culture to the scene. While not a panacea for deep-rooted problems of organisational culture, simulation training across departmental interfaces can be a useful strategy for teams to develop a continuity of care perspective and a refocus on the superordinate goal of patient outcomes. Creating, scheduling and running simulations that engage four or more specialty disciplines at once is a challenge in any unit and support from departmental heads is vital. The rewards from this investment (even when only two or three disciplines train together) can be immense, with many ‘light bulb’ moments as clinicians gain vital insights into how the others specialties view themselves and others’ roles during an unfolding emergency.
Crucial to the success of interdisciplinary simulation is an effective debriefing process involving participants across departmental interfaces. The aim of the debriefing in this instance extends beyond the clinical, team and system lessons learned to providing an opportunity to get to know and understand cross-disciplinary teammates and to learn and rehearse giving and receiving feedback constructively. Exactly how to conduct this debrief and use this shared reflective experience requires further examination.12
Summary
Simulation is a multifaceted tool used to improve individual technical skills, teamwork, systems and processes and enhance workplace culture. These improvements combine to create better clinicians, teams and workplaces, positively influencing clinical outcomes for our patients. Expertise and discipline is required to match the simulation training modality appropriately to the desired clinical and organisational goals. A modern ‘must have’ for all birthing units, this metaphorical Swiss Army knife (consisting of the simulation equipment and appropriate expertise) will continue to expand in scope and effectiveness into the future.
References
- Crofts JF, Lenguerrand E, Bentham GL, et al. Prevention of brachial plexus injury—12 years of shoulder dystocia training: an interrupted time-series study. BJOG: 2016;123(1):111-8.
- Gossett DR, Gilchrist-Scott D, Wayne DB, Gerber SE. Simulation Training for Forceps-Assisted Vaginal Delivery and Rates of Maternal Perineal Trauma. Obstet Gynecol. 2016;128(3):429-35.
- Dupuis O, Moreau R, Pham MT, Redarce T. Assessment of forceps blade orientations during their placement using an instrumented childbirth simulator. BJOG: 2009;116(2):327-33.
- McGaghie WC. Mastery learning: it is time for medical education to join the 21st century. Acad Med. 2015;90(11):1438-41.
- Weaver SJ, Lyons R, DiazGranados D, et al. The anatomy of health care team training and the state of practice: a critical review. Acad Med. 2010;85(11):1746-60.
- Cornthwaite K, Edwards S, Siassakos D. Reducing risk in maternity by optimising teamwork and leadership: an evidence-based approach to save mothers and babies. Best Pract Res Clin Obstet Gynaecol. 2013;27(4):571-81.
- Härgestam M, Lindkvist M, Brulin C, et al. Communication in interdisciplinary teams: exploring closed-loop communication during in situ trauma team training. BMJ Open. 2013;3(10):e003525.
- Zendejas B, Brydges R, Wang AT, Cook DA. Patient outcomes in simulation-based medical education: a systematic review. J Gen Intern Med. 2013;28(8):1078-89.
- Weaver SJ, Lyons R, DiazGranados D, et al. The anatomy of health care team training and the state of practice: a critical review. Acad Med. 2010;85(11):1746-60.
- Hewett DG, Watson BM, Gallois C, et al. Intergroup communication between hospital doctors: implications for quality of patient care. Soc Sci Med. 2009;69(12):1732-40.
- Molleman E, Broekhuis M, Stoffels R, Jaspers F. Complexity of health care needs and interactions in multidisciplinary medical teams. Journal of Occupational and Organizational Psychology. 2010;83(1):55-76.
- Brazil V. Just another debrief? Recruiting for an in situ simulation study. 2017 Mar 17 [cited 2017 Apr 9]. In: Debrief2Learn [Internet]. Available from: https://debrief2learn.org/in-situ-simulation-study/..







Leave a Reply