The authors were fortunate enough to be awarded the Shan S Ratnam Young Gynaecologist Award (YGA) 2017 for New Zealand (NZ) and Australia respectively. This award, first initiated in 1991, was the brainchild of Prof Masahiko Mizuno, then President of Asia and Oceania Federation of Obstetricians and Gynaecologists (AOFOG) and was subsequently renamed the Shan S Ratnam YGA in memory of Emeritus Prof SS Ratnam, who was the President Elect of the AOFOG at the time of his death in 2001. The aim of the YGA was to help in the collaboration and development of the next generation of leaders in O&G in the Asia and Oceania region.
As YGA recipients, we were provided the opportunity to attend the 25th AOFOG congress in Hong Kong (HK), as well as be involved in a fabulous pre-congress program. This enabled us to experience a new health system, reflect on our own clinical practices and comprehend the differing obstetric and gynaecological needs of nations in the Asia and Oceania region. Our program in HK, attended by 22 YGAs from 18 countries, was brilliantly organised by Dr Vincent Cheung, with support from the Hong Kong College of Obstetricians and Gynaecologists (HKCOG).
During our eight-day pre-congress program, we had the opportunity to be immersed in various aspects of O&G care in HK, including undertaking clinical observerships in five HK hospitals – the Pamela Youde Memorial Hospital; Queen Mary Hospital; Prince of Wales Hospital; HK Sanatorium and Hospital; and the Kwong Wah Hospital. In general, HK has a very similar system of O&G practice to Australia and NZ, reflective of a common Commonwealth past and continued modelling of practice to the NICE and RCOG guidelines. Public care in O&G is the norm, with the vast majority of HK residents accessing this system. Private care is not as prevalent as in Australia, primarily due to the inability for specialists to be simultaneously involved in both public and private models of care. Clients in HK can also refer themselves directly to O&G services without the need for primary care referrals; a significant difference to our models of care, where primary care providers are the ‘gate keepers’ to specialist referrals. There are also no independent midwifery models of maternity care as are present in NZ.
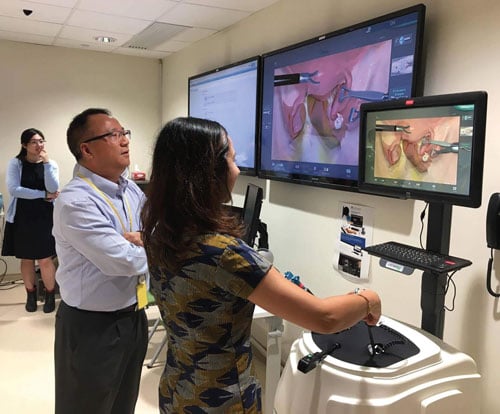
Simulation training at the HK Jockey Club Innovation Learning Centre for Medicine.
Within the hospital, O&G clinical practice and hierarchy is very similar to Australia and NZ, with all clinical levels of staff involved in duties, including daily ward rounds, antenatal and gynaecology clinics, operating lists, early pregnancy clinics and subspecialty-related care. Despite the many similarities, some differences in clinical practice were evident, such as the lack of routine HPV screening and HPV vaccination programs (additional cost to the patient of $HK50 per Pap smear and $HK1000 per vaccine), while robotic surgery was extensively used even in smaller hospital centres. However, two particular aspects of practice stood out as unique – first, the extensive use of simulation technology in training; and, secondly, the incorporation of Traditional Chinese Medicine (TCM) in the care of patients.
Our tour to the Pok Oi Chinese Medicine Hospital provided a fascinating insight into the world of TCM and the esteem in which it is held among the local populace in HK. The demand for and use of TCM has led to the formalised development of TCM institutes and university programs, with graduates of both Western and Chinese medicine trained in the provision of TCM. Some examples in O&G include the provision of acupuncture for chronic pelvic pain and pain relief in labour and the prescription of herbal remedies for menorrhagia and menopausal symptoms, among many others. As TCM is increasingly being incorporated into practice, there is also a greater emphasis on research, with TCM undergoing the rigours of Western evidence-based trials to conform to modern medical practice. Some of our more adventurous colleagues were lucky enough to experience different therapies, including acupuncture and cupping during our visit.
Another interesting aspect was the extensive use of a simulation centres for training and continued skill development. Our visit to the state-of-the-art HK Jockey Club Innovation Learning Centre for Medicine (HKJCILCM) was captivating. Equipped with skill-training simulators (such as laparoscopic trainers, TV ultrasound) and high-fidelity human patient simulators (Sim Mum) in a facility that can simulate different clinical settings (including operating theatres, clinical wards and obstetric labour room), provided the reality of simulation training in O&G. Additionally, the presence of a virtual reality room with a 360-degree panoramic screen allowed training for major medical emergencies and public relations management. Though simulation training is already present in certain facilities in Australia and NZ, the emphasis of simulation as part of O&G training and its use for regular drills by clinical staff is significantly more prevalent in HK and reflects a growing trend in developed clinical settings where stringent simulation training is mandated before involvement with clinical cases.
In addition to our visits around HK, we were given a rare opportunity to visit the recently built University of HK – Shenzen (HKU-Shenzen) hospital in Shenzen, China. This is a predominantly public hospital, with a private wing built from the collaboration between the University of HK and the local Shenzen Municipal government. This 3000 bed hospital, built to conform to international medical standards, is viewed in part as a push to reform the healthcare sector in China and provide patient-orientated care. From an obstetric perspective, maternity care for a public patient would cost approximately $A500 for a package comprising antenatal care, delivery and postnatal care. In contrast, private care is roughly $A5000 depending on the accommodation in the private wing, with costs of up to $30,000 per night for the use of the ‘presidential’ suite. Delivering here has become so popular that they now run a lottery to determine who will get the opportunity. The HKU-Shenzen hospital may be a glimpse of what is to come in China’s push to reform its healthcare sector to meet international standards and local demands for patient-centred care.
The penultimate aspect of the YGA program was the receipt of certificates at the President’s dinner and congratulations to the candidates involved. This was attended by many well-known figures, including Sir Sabaratnam Arulkumaran, Prof Purandare (President of FIGO), Prof Nam (President of AOFOG); the AOFOG committee and various prominent specialists from the many countries involved.
In addition to the immersion in the local health service, one of the main themes of the program was the interaction between the YGAs from various countries and the friendships and collegiality that developed during this time. This is in keeping with the 2017 theme of AOFOG Congress of ‘unity and sharing’ and will hopefully be continued for many years to come.
We now look forward to the next AOFOG meeting in Manila in 2019!

President’s dinner presentation to the YGA recipients.







Leave a Reply