There are approximately 25,000 preterm (less than 37 weeks gestational age) livebirths in Australia every year.1
(Figure 1).
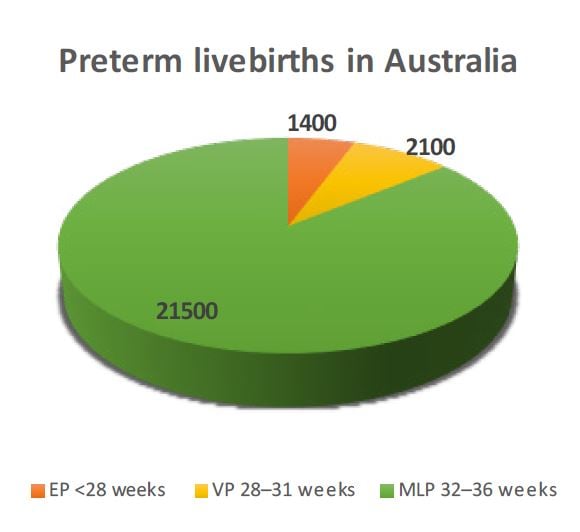
Figure 1. Approximate distribution of yearly preterm livebirths in Australia
Children born extremely preterm
Before neonatal intensive care nurseries were able to provide effective assisted ventilation, which started in Australia in the early 1970s, very few babies born extremely preterm (EP) survived. Antenatal corticosteroids were introduced in Australia in the late 1970s and further improved survival rates by accelerating pulmonary surfactant production and reducing the severity of hyaline membrane disease (also called respiratory distress syndrome), the commonest cause of death in babies born preterm. The next major advance was the ability to give replacement surfactant therapy to preterm babies after birth, which became available from 1991 in Australia. In conjunction with an increased willingness to provide treatment for babies born EP both before and after birth, long-term survival rates rose, from less than ten per cent in the 1960s, to approximately 70 per cent on a whole population basis for those born 22–27 weeks gestation by the late 1990s.2 Since the 90s there have been incremental improvements, but no major advances that have further affected survival rates.
The Victorian Infant Collaborative Study (VICS) group has been following cohorts of all babies born either below 1000g or before 28 weeks gestational age in the state of Victoria from the 1970s, 1980s, 1990s, and 2000s into school-age, and in some cases, into adulthood. At eight years of age, one-in-six survivors born EP have substantial neurosensory disability,3 such as problems with thinking, hearing, walking, talking or vision, which would represent up to 160 children born EP every year in Australia. In contrast, when we assess children born at term, one-in-60 also have substantial disability using the same criteria,4 which represents almost 5000 disabled children born at term every year in Australia. Thus, although the risk is higher in children born EP, a child in the classroom with substantial disability is at least 30 times more likely to have been born at term than born EP. In addition to substantial neurosensory disability, children born EP compared with those born at term have poorer school performance in reading, spelling and arithmetic, they have more problems with inattention, remembering things and organising themselves, and they are clumsier.
Considering other health problems, children born EP are disadvantaged as a group compared with children born at term in almost every area of health we have studied. They are a little shorter and lighter in body weight throughout childhood, but they narrow the gap in weight by adulthood.5 They remain shorter by several centimetres on average, although, their parents are shorter on average than the parents of children born at term.
Blood pressure is higher by 2–4 mmHg in childhood and early adulthood,6 7 which may not sound like an important difference; however, each 2 mmHg rise in blood pressure is associated with an increased risk of cardiovascular events, such as stroke or heart attack, in later life.8 Whether survivors born EP will have higher rates of cardiovascular disease in later adulthood remains to be determined.
The airways in the lungs grow through pregnancy and early life, peaking in the early 20s, after which there is a gradual decline with age. In most of us the decline with age is not a concern because we will die from something other than lung disease before our lung function declines to a level that cannot support life; though smokers are one obvious exception. Compared with the very low oxygen exposure of the lungs in utero, exposure to even air after birth is too much oxygen for the immature lungs of babies born EP. Also, most babies born EP need assisted ventilation and higher concentrations of oxygen than air after birth, sometimes for many weeks or months, both of which damage the lungs and interfere with lung growth and development. Consequently, it is not surprising that the breathing ability of children born EP is reduced when they have lung function tests later in life compared with children born at term.9 Of long-term concern, it is clear that adults born EP are not attaining the normal peak of lung growth that occurs in the early 20s, and more are destined to develop chronic obstructive pulmonary disease in adulthood, even if they do not smoke.
Despite the higher rates of problems described above, it is important to realise that most children and adults born EP are healthy and lead normal lives; they feel good about themselves, and report that their overall health is as good as people born at term.10 Some have even grown up to be obstetricians and paediatricians!
Children born very preterm
Almost all babies born 28–31 weeks gestation today will survive long-term, particularly if they are born with the benefit of antenatal corticosteroids and in a tertiary level maternity hospital. However, children born very preterm (VP) have more of the health problems listed above than do children born at term, but not at such high rates as in those who were born EP. Like children born EP, those born VP are at high enough risk of adverse health problems that routine health surveillance and follow-up is recommended, at least through early childhood.
Children born moderate-to-late preterm
Most babies born preterm will deliver closer to term than further away from it. Consequently, individual obstetricians will be dealing with livebirths who are moderate-to-late preterm (MLP) far more frequently than those born EP, at a ratio of approximately 15 to one. Children born MLP were previously thought to have an excellent long-term prognosis, akin to those born full-term, and were not considered high enough risk to warrant additional health surveillance in childhood. However, it is now clear that being born MLP is associated with substantial increases in long-term health problems compared with children born at term, including all those outlined for children born EP, but at lower rates.11 12 Compared with children born at term, those born MLP have higher rates of academic underperformance, lower IQ and more respiratory health problems. In childhood, they often require more hospitalisation than term children for a variety of health problems, most commonly respiratory illnesses including asthma and respiratory infections. In adulthood, they need more treatment for hypertension13 and diabetes,14 have more psychiatric problems,15 require more economic assistance for health problems16 and have lower academic achievement,17 which leads to lower paid work and more unemployment than do those born at term. It is important, however, to bear in mind that most children born MLP do well, but their higher risks of health and developmental problems compared with those born at term highlight the importance of considering the indications for non-urgent delivery carefully, as well as the need for closer developmental and health surveillance long term for those born MLP.
What can obstetricians do for preterm babies?
The long-term outcomes for EP and VP babies are substantially improved if they are born in a tertiary maternity hospital with an onsite neonatal intensive care unit. Obstetricians have a key role in identifying those most likely to deliver EP or VP and organising transfer of the pregnant mother before birth to an appropriate high-risk tertiary maternity hospital, which may involve travel over large distances in some instances. In addition, obstetricians need to remember to give antenatal corticosteroids for those likely to deliver before 35 completed weeks of gestation. For obstetricians working in high-risk maternity hospitals, magnesium sulphate given to the mother before birth will help to reduce the chance of later cerebral palsy in babies likely to deliver before 30 weeks gestation.18
For babies where delivery might be contemplated between 32–36 weeks, consider delaying delivery, if possible, and resist requests for earlier delivery for ‘social’ reasons.
Acknowledgements
This study was supported by Australia’s National Health & Medical Research Council (Centre for Clinical Research Excellence 546519; Centre for Research Excellence 1060733; Career Development Fellowship 1141354 to J.L.Y.C.), and the Victorian Government’s Operational Infrastructure Support Program.
References
- Australian Institute of Health and Welfare. Australia’s mothers and babies 2016—in brief. Perinatal statistics series no 34 Cat no PER 97 Canberra: AIHW2018.
- Doyle LW, Roberts G, Anderson PJ. Outcomes at age 2 years
of infants <28 weeks’ gestational age born in Victoria in 2005. J Pediatr. 2010;156:49-53. - Cheong JLY, Anderson PJ, Burnett AC, et al. Changing neurodevelopment at 8 years in children born extremely preterm since the 1990s. Pediatrics. 2017;139:e20164086.
- Cheong JLY, Anderson PJ, Burnett AC, et al. Changing neurodevelopment at 8 years in children born extremely preterm since the 1990s. Pediatrics. 2017;139:e20164086.
- Roberts G, Cheong J, Opie G, et al. Growth of extremely preterm survivors from birth to 18 years of age compared with term controls. Pediatrics. 2013;131:e439-45.
- Roberts G, Lee KJ, Cheong JL, et al. Higher ambulatory blood pressure at 18 years in adolescents born less than 28 weeks’ gestation in the 1990s compared with term controls. J Hypertens. 2014;32:620-6.
- Hovi P, Vohr B, Ment LR, et al. Blood pressure in young adults born at very low birth weight: Adults born Preterm International Collaboration. Hypertension. 2016;68:880-7.
- Cook NR, Cohen J, Hebert PR, et al. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Int Med. 1995;155:701-9.
- Cook NR, Cohen J, Hebert PR, et al. Implications of small reductions in diastolic blood pressure for primary prevention. Arch Int Med. 1995;155:701-9.
- Roberts G, Burnett AC, Lee KJ, et al. Quality of Life at Age 18 Years after Extremely Preterm Birth in the Post-Surfactant Era. J Pediatr. 2013;163:1008-13.
- Cheong JL, Doyle LW. Increasing rates of prematurity and epidemiology of late preterm birth. J Paediatr Child Health. 2012;48:784-8.
- Cheong JL, Doyle LW, Burnett AC, et al. Association between moderate and late preterm birth and neurodevelopment and social-emotional development at age 2 years. JAMA Pediatrics. 2017;171:e164805.
- Crump C, Winkleby MA, Sundquist K, et al. Risk of hypertension among young adults who were born preterm: a Swedish national study of 636,000 births. Am J Epidemiol. 2011;173:797-803.
- Crump C, Winkleby MA, Sundquist K, et al. Risk of diabetes among young adults born preterm in Sweden. Diabetes Care. 2011;34:1109-13.
- Lindstrom K, Lindblad F, Hjern A. Psychiatric morbidity in adolescents and young adults born preterm: a Swedish national cohort study. Pediatrics. 2009;123:e47-53.
- Moster D, Lie RT, Markestad T. Long-term medical and social consequences of preterm birth. N Engl J Med. 2008;359:262-73.
- Lindstrom K, Winbladh B, Haglund B, et al. Preterm infants as young adults: a Swedish national cohort study. Pediatrics. 2007;120:70-7.
- The Antenatal Magnesium Sulphate for Neuroprotection Guideline Development Panel. Antenatal magnesium sulphate prior to preterm birth for neuroprotection of the fetus, infant and child: National clinical practice guidelines. Available from: www.nhmrc.gov.au/guidelines/publications/cp128.






Leave a Reply