Preterm birth (PTB) occurs in five to 18 per cent of pregnancies and is the leading cause of neonatal morbidity and mortality, and infant death. Although a previous spontaneous preterm birth is an important risk factor for a recurrent preterm birth, nearly 70 per cent of PTBs occur for women without an identifiable risk factor.
There is good biological plausibility for the use of progesterone to prevent preterm birth. Progesterone insufficiency is considered to be one of the main contributors to the process that triggers uterine contractility. Progesterone reduces myometrial sensitivity to oxytocin, blocks adrenergic receptors and prostaglandin synthesis and stimulates lymphocyte-associated synthesis of progesterone induced blocking factor, all of which facilitate uterine quiescence during pregnancy.
Meis et al,1 in their landmark randomised trial in women with previous spontaneous preterm birth, reported a significant reduction in preterm birth with 250 mg weekly intramuscular injection of 17 hydroxy progesterone caproate. The study has been heavily criticised because of the very high rate of preterm birth in the control group and because the rate of preterm birth in the treatment group was similar to that in the general population. This study did, however, lead to a flurry of randomised controlled trials assessing the role of progesterone in reducing preterm birth.
There are two forms of progestogens available in Australia, 17 OH progesterone and the micronised progesterone as a 100 or 200 mg tablet. For the purpose of this article, we will only consider the use of the latter.
Although many randomised trials on progesterone for the prevention of preterm birth have been published, the results have been inconsistent owing to the selection of women randomised; with or without previous preterm birth, with or without known cervical length (CL) singleton and multiple pregnancies. As a result, the published systematic reviews have also been less informative and with possibly misleading conclusions. The 2013 Cochrane Review,2 for example, has a general conclusion that vaginal progesterone is of benefit in women with previous history of preterm birth. There was no mention made of the CL. Others have selected women with singleton pregnancy3 4 and with multiple pregnancy5 with a short cervix and noted that the benefit is limited to this group only.
Paramount to determining the success of progesterone to reduce risk of preterm birth is therefore to identify women who will benefit. It is not efficacious for all women. For this reason, we have used data from papers and reviews that have used individual patient data analysis so that there is clearer patient selection and thus hopefully make clearer recommendations.
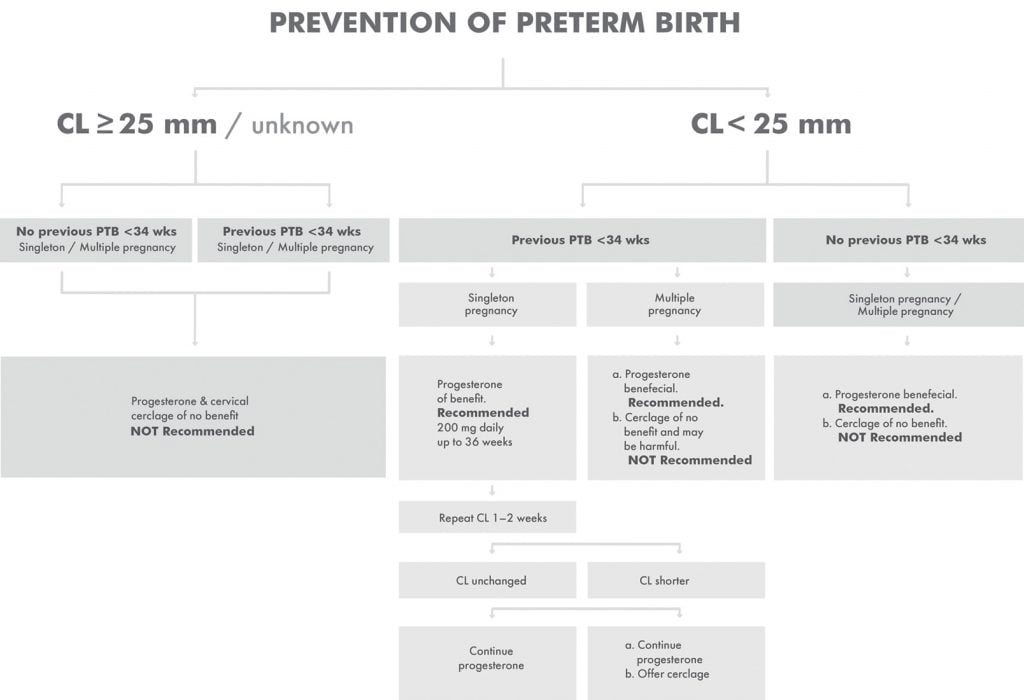
Figure 1. Flowchart for the use of progesterone to prevent preterm birth.
Efficacy of progesterone
Singleton or twin pregnancy with or without previous preterm birth and normal or unknown CL
Singleton pregnancies
O’Brien’s study6 excluded women with short CL, PROGRESS trial7 with CL unknown/unspecified and OPPTIMUM8 with mixed CL population, have all failed to show any beneficial effect of progesterone for the prevention of preterm birth.
Multiple pregnancies
In a review of non-selected twin pregnancies,9 progesterone did not significantly reduced the risk of preterm birth overall at <34 or <37 weeks of gestation, the relative risk of preterm birth <34 weeks of gestation was 0.82 (95% CI 0.64–1.05). Another metanalysis of three trials, including the PREDICT study, reported that there was no significant effect of progesterone on the risk of preterm birth; pooled odds ratio, 1.07 (95% CI, 0.52–2.19).10
Currently, the use of vaginal progesterone cannot be recommended for these women.
Singleton or twin pregnancy with CL ≤25 mm, with and without previous preterm birth
A subgroup analysis in the metanalysis of trials on women with singleton pregnancy and a short cervix that also included selective women from the OPPTIMUM study11 reported that the frequencies of preterm birth <36, <34 and <28 weeks of gestation were significantly lower in the vaginal progesterone group.
There was also a significant reduction in the risk of respiratory distress syndrome, composite neonatal morbidity and mortality and admission to the neonatal intensive care unit (NICU); frequency of neonatal death was 1.4% in the vaginal progesterone group and 3.2% in the placebo group.
A review that included women with twin pregnancy and a short cervix12 also concluded that vaginal progesterone significantly lowered the incidence of preterm labour before 34 weeks of gestation and another13showed a reduction in adverse perinatal outcome (15/56 versus 22/60; RR 0.57; 95% CI 0.47–0.70)
Currently, vaginal progesterone 100–200 mg daily is recommended from early pregnancy until 36 weeks gestation.
Singleton pregnancy with CL ≤25 mm and a previous spontaneous preterm birth
The beneficial effect of vaginal progesterone and cervical cerclage in this subgroup has been shown in a large systematic review.14 Vaginal progesterone, compared to placebo, significantly reduced the risk of preterm birth <35 and <32 weeks of gestation, composite perinatal morbidity/mortality, neonatal sepsis, composite neonatal morbidity, and admission to the NICU (RRs from 0.29 to 0.68). Cervical cerclage, compared to no cerclage, also significantly decreased the risk of preterm birth <37, <35, <32, and <28 weeks of gestation, composite perinatal morbidity/mortality, and birthweight <1500 g (RRs from 0.64 to 0.70). There was no significant difference between the two interventions
A Cochrane review15 also reported that there were no significant differences between the two interventions in the risk of preterm birth <37 weeks (RR, 1.16; 95% CI, 0.64–2.08), <34 weeks (RR, 1.01; 95% CI, 0.51–2.01), perinatal mortality (RR, 0.94; 95% CI, 0.36–2.48), and serious neonatal morbidity (RR, 0.49; 95% CI, 0.05–4.52).
Cervical cerclage placement is, however, associated with increased risk of rupture of membranes, chorioamnionitis, vaginal bleeding and cervical trauma, as well as the risks associated with the anaesthesia.
The choice of treatment therefore would be based on risk of adverse effects of an invasive procedure, cost-effectiveness as well as the woman’s preference. The following practical recommendation is thus suggested:
Currently, in this subgroup, continuing vaginal progesterone is recommended as first-line prevention as stated above and repeat CL in one to two week:
- if CL remains static continue progesterone only
- if CL shortens further, offer cervical cerclage in addition
Multiple pregnancy with CL ≤25 mm and a previous spontaneous preterm birth
A systematic review16 noted that although there were no significant differences between cervical cerclage and vaginal progesterone for this subgroup, in the risk of preterm birth, very low birthweight (aOR 2.22, 95% CI 1.07–5.73) and respiratory distress syndrome (aOR 3.88, 95% CI 1.09–21.03) were more frequent in the cerclage group.
Currently, in this subgroup, vaginal progesterone only is recommended. Cervical cerclage may be associated with harm.
Safety of progesterone
Regarding its safety, there is no evidence of any short- or long-term harm to either the mother or the newborn. The OPPTIMUM trial17 reported on childhood outcomes at age two years using the Bayley Score of Infant Development and Vedel et al.18 at an eight-year follow up; neither have noted any harmful effect of exposure to progesterone.
We should no longer consider the success of intervention only on birth before 37 or before 34 completed weeks of gestation. Studies need to address particularly on any effect on fetal neonatal short- and long-term morbidity.
References
- Meis PJ, Klebanoff M, Thom E, et al. Prevention of recurrent preterm delivery by 17 alpha-hydroxyprogesterone caproate. N Engl J Med. 2003;348(24):2379e85.
- Dodd JM, Jones L, Flenady V, et al. Prenatal administration of progesterone for preventing preterm birth in women considered to be at risk of preterm birth. Cochrane Database Syst Rev. 2013, Issue 7. Art. No.: CD004947.
- Romero R, Conde-Agudelo A, Da Fonseca E, et al. Vaginal progesterone for preventing preterm birth and adverse perinatal outcomes in singleton gestations with a short cervix: a meta-analysis of individual patient data. Amer J Obstet Gynecol. 2018;218(2):161-80.
- El-Refaie W, Abdelhafez MS, Badawy A. Vaginal progesterone for prevention of preterm labor in asymptomatic twin pregnancies with sonographic short cervix: a randomized clinical trial of efficacy and safety. Arch Gynecol Obstet. 2016;293(1):61-7.
- Jarde A, Lutsiv O, Park CK, et al. Preterm birth prevention in twin pregnancies with progesterone, pessary, or cerclage: a systematic review and meta-analysis. BJOG. 2017;124:1163-73.
- O’Brien JM, Adair CD, Lewis DF, et al. Progesterone vaginal gel for the reduction of recurrent preterm birth: primary results from a randomized, double-blind, placebo-controlled trial. Ultrasound Obstet Gynecol. 2007;30(5):687-96.
- Crowther CA, Ashwood P, McPhee AJ, et al. Vaginal progesterone pessaries for pregnant women with a previous preterm birth to prevent neonatal respiratory distress syndrome (the PROGRESS Study): A multicentre, randomised, placebo-controlled trial.
PLoS Med. 2017;14(9):e1002390. - Norman JE, Marlow N, Messow CM, et al. Vaginal progesterone prophylaxis for preterm birth (the OPPTIMUM study): a multicentre, randomised, double-blind trial. Lancet. 2016;387:2106-2116.
- Jarde A, Lutsiv O, Park CK, et al. Preterm birth prevention in twin pregnancies with progesterone, pessary, or cerclage: a systematic review and meta-analysis. BJOG. 2017;124:1163-73.
- Klein K, Rode L, Nicolaides KH, et al. Vaginal micronized progesterone and risk of preterm delivery in high-risk twin pregnancies: secondary analysis of a placebo-controlled randomized trial and meta-analysis. Ultrasound Obstet Gynecol. 2011;38(3):281-7.
- Romero R, Conde-Agudelo A, Da Fonseca E, et al. Vaginal progesterone for preventing preterm birth and adverse perinatal outcomes in singleton gestations with a short cervix: a meta-analysis of individual patient data. Amer J Obstet Gynecol. 2018;218(2):161-80.
- Crowther CA, Ashwood P, McPhee AJ, et al. Vaginal progesterone pessaries for pregnant women with a previous preterm birth to prevent neonatal respiratory distress syndrome (the PROGRESS Study): A multicentre, randomised, placebo-controlled trial.
PLoS Med. 2017;14(9):e1002390. - Schuit E, Stock S, Rode L, et al. Effectiveness of progestogens to improve perinatal outcome in twin pregnancies: an individual participant data meta-analysis. BJOG. 2015;122: 27-37.
- Conde-Agudelo A, Romero R, Da Fonseca E, et al. Vaginal progesterone is as effective as cervical cerclage to prevent preterm birth in women with a singleton gestation, previous spontaneous preterm birth, and a short cervix: updated indirect comparison meta-analysis. Amer J Obstet Gynecol. 2018;219(1):10-25.
- Alfirevic Z, Stampalija T, Medley N. Cervical stitch (cerclage) for preventing preterm birth in singleton pregnancy. Cochrane Database Syst Rev. 2017;6:CD00899.
- Saccone G, Rust O, Althuisius S, et al. Cerclage for short cervix in twin pregnancies: systematic review and meta-analysis of randomized trials using individual patient-level data. Acta Obstet Gynecol Scand. 2015,94:352-8.
- Norman JE, Marlow N, Messow CM, et al. Vaginal progesterone prophylaxis for preterm birth (the OPPTIMUM study): a multicentre, randomised, double-blind trial. Lancet. 2016;387:2106-2116.
- Vedel C, Larsen H, Holmskov A, et al. Long-term effects of prenatal progesterone exposure: neurophysiological development and hospital admissions in twins up at 8 years of age. Ultrasound Obstet Gynecol. 2016;48(3):382-89.






Leave a Reply