Close your eyes for a moment and let me take you on a journey – the scene is a regular elective operating list at your public hospital, the theatre at a bracing 20°C. The consultant, male and 185 cm, has a new senior registrar assisting, female and 158 cm. The patient, BMI of 55, is on the usual operating table with its usual range of adjustment, lying on 2cm of gel mat and HoverMatt®. Due to her BMI she also has a Trenguard® in place, adjusted so that the frame protrudes from the side of the table by 10 cm. The right arm is on an arm board because the anaesthetist had trouble getting IV access. Ports are inserted quite medially because of the pannus, instruments selected and Trendelenburg applied. The surgeon is reasonably well placed and can see the monitor near the patient’s right foot. The shorter assistant calls for a platform to stand on, but finds that because of natural shorter arm length she has trouble reaching. She stands too far forward because of the arm board and struggles with the difficult catches on the one-size-fits-all instrument handles. The surgeons must twist to reach and see the monitor, placed too high. Two hours later, this challenge in OH&S is over.
Sound familiar? Ergonomics derives from the Greek words ergon (work) and nomoi (natural laws). Combined, they create the modern concept of the science of work and a person’s relationship to it. In application, ergonomics is the discipline focused on making tasks and products comfortable and efficient for the user.
Laparoscopic surgery’s (LS) advantages to our patients are well documented. De Quervain published on the importance of operating table height in 19061 and over the past two decades the very different ergonomic implications of laparoscopic surgery have slowly been explored.

The great epidemic?
The exact prevalence of musculoskeletal disorders in surgeons is unknown due to reporting bias, study design and lack of a standardised assessment tool. Estimates of up to 73–88 per cent are common, or as little as 20 per cent if we assume survey non-responders have zero pain.2 In LS, surgeons face multiple physical issues that directly expose them to risk of developing musculoskeletal disorders. These include static body posture, repetitive upper extremity movements, overreaching and force exertion from adverse positions and inefficient instruments. This is exacerbated by duration of work, time pressures, 2D vison and limited range of instrument movement and demand for precision. LS also presents higher risk than open surgery.
Compared to all other occupations, these prevalence estimates can be considered excessive, with rates of 22–24 per cent average across other professions.3 We also have the unique situation of grossly disparate physical characteristics in our workers, as above, and a ‘one size fits all’ mentality in design of our equipment.
Factors linked to musculoskeletal disorders
Male versus female surgeons
The average male height in Australia is 175 cm, hand length 18.8 cm, and the female average is 161 cm and 16.8 cm. Female surgeons are significantly more likely to seek treatment for hand injuries and other musculoskeletal disorders and report more cases of shoulder discomfort when controlled for hand size. Surgeons with smaller hands report greater difficulty using laparoscopic instruments than those with medium to large hands (P<0.001).4 Specifically, instrument handle design was reported as a cause of physical complaints in up to 83 per cent of respondents5 with reports of pressure areas (36 per cent), neuropraxia (26 per cent) and uncomfortable posture (57 per cent). Instrument design was considered a significant factor in surgeon disc prolapse.6
Surgeon experience
Perhaps contrary to expectation, surface electromyography has demonstrated that assistants exhibit greater activation of biceps, triceps and trapezius muscle groups compared to primary surgeons and are therefore more likely to experience ergonomic stress.7 Similarly, several studies report surgeon experience as a highly relevant determinant of ergonomic stress, with more experienced surgeons less affected.8 It is not known whether this reflects technique or muscle conditioning.
Surgeon versus operating table and patient height
Guidelines for the height of work surfaces for standing workers in industry or offices who are performing precision, light or heavy work have existed9 for decades, but only recently has this work appeared in the LS ergonomic literature. It is increasingly apparent that operating tables cannot be adjusted sufficiently low to allow for the height of 95 per cent of surgeons in the context of LS, with most tables being too high.10 Modern operating tables adjust for a surface height of between 73 and 122 cm. On top of this, we need to add the patient’s abdomen and the often-considerable extra space created by pneumoperitoneum. Surgeons compensate for this by elevating their arms and shoulders with resultant muscle strain and tension with loss of dexterity, or by climbing on to a step. This limits their movement as well as access to foot switches required by most laparoscopic diathermy devices, resulting in a cluttered and potentially unsafe foot space and awkward posture.
So, what is the optimal table height? Matern et al’s elegant study11 considers the varied heights needed to activate four laparoscopic handles (shank, pistol, axial and rod) and assuming an insertion angle of 20 degrees and elbow angle of 90 degrees indicates a working height of 103 cm. However, the lowest operating table height (73 cm) added to the ‘average’ insufflated patient diameter of 40 cm gives a height of 113 cm. This will prove to be too high for 95 per cent of surgeons.
The importance of elbow angle
This dictates the eventual height of the operating table; the perfect height lies between 70–80 per cent of elbow height.12 This study determined that the most relaxed (electromyography neutral) posture for the upper limb lies with arms slightly abducted, retroverted, rotated inwards at the shoulder and with an elbow angle of 90–120 degrees. When the height of the operating table was set at less than 80 per cent of elbow height, significantly more neutral shoulder positions were recorded at 90 per cent and above (P<0.05).The most neutral wrist excursions were recorded with heights of 70–80 per cent, and heights in the lower range introduced back flexion of up to 25 degrees. This means an unachievable table height of between 29–69 cm.
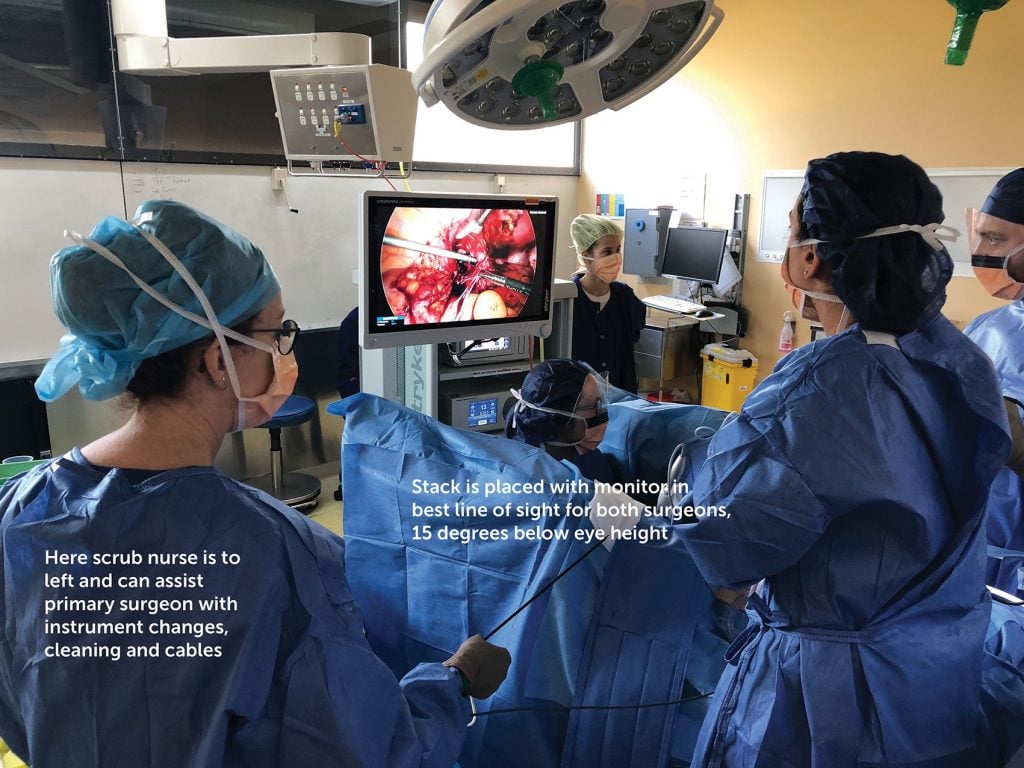
Monitor position
Ideally, the visual axis of the surgeons’ work should approximate their mechanical axis. Prospective studies indicate decreased operating time for moderate complexity LS procedures.13 The screen is preferably positioned in the surgeons’ direct line of sight, in line with their forearm–instrument motor axis. The screen height should be positioned below eye height to allow ‘gaze down viewing’, allowing alignment with the motor axis.
This research commenced with the advent of monitor-rich workplaces in the 1980s and suggests that eyestrain is influenced by monitor distance and vertical angle. The neutral orientation of the human eye in the orbit is at an angle of 15 degrees gaze down. In a relaxed state, the accommodation of the unrefracted human eye is approximately 1.3 dioptres, giving a focal length of 0.8 m and average convergence distance is 1 m. Here, the orbital and ciliary muscles are in their most relaxed state.14
These studies demonstrate strong correlation with observed personal preference and efficiency trial data, recommending a monitor distance of 0.8–1.2 m, although this may be increased for larger high-resolution screens.
Patient positioning
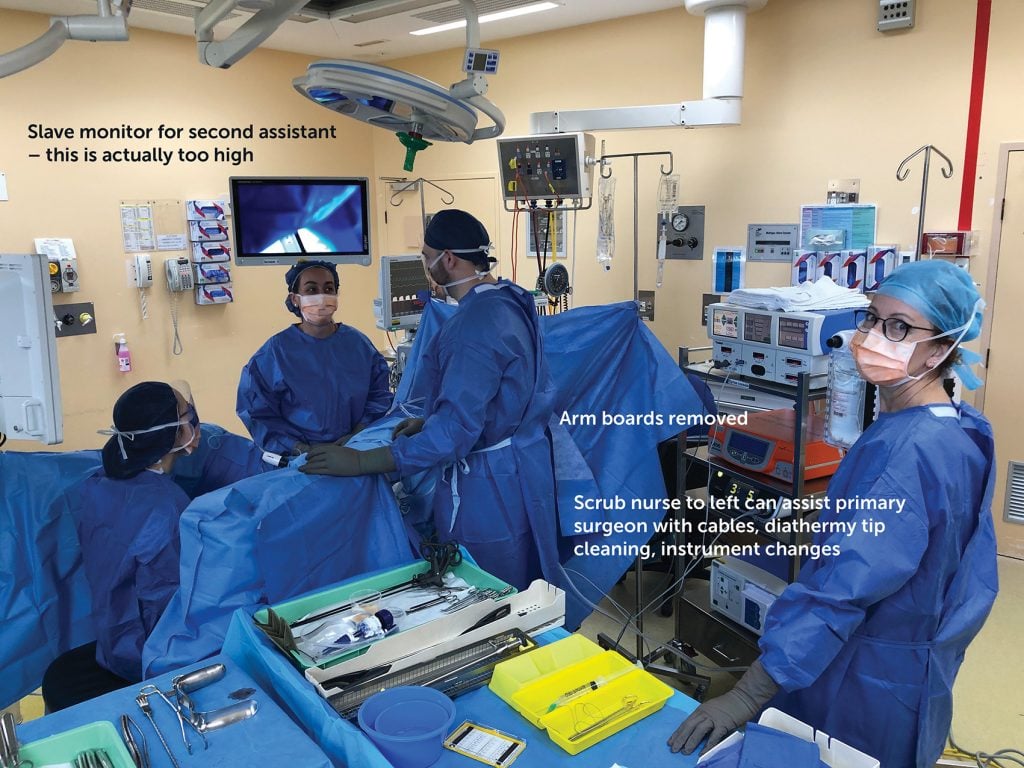
The importance of this cannot be overemphasised. I make it a point to always check positioning and safety of the patient, including pressure points, before scrubbing. The well described principles of patient positioning include the ability to sustain prolonged head down position, which in most cases cannot be accommodated by a standard operating table mat. Favourites include gel mats, bean bags and the Trenguard. The latter usually comes with an extended frame that protrudes from the lateral edge of the operating table, providing a sharp corner to lean on for the duration of the laparoscopy. The frame can easily be cut to just less than the width of the table without impairing its properties. Pronounced Trendelenburg renders it necessary for the surgeon to stand further towards the patient’s head, and so arm boards must, in every circumstance, be removed.
Position of scrub nurse and instrument table
Generally, the dynamics of LS are very different to open surgery – a smaller number of longer instruments that are usually a ‘set piece’ and once the place. For ease of access, I favour ‘saddle bags’ over the patient’s thighs, which allow the instruments to be spread out for easier access. This also avoids the possibility of delicate Maryland bipolar tips being damaged when dropped to the bottom of a quiver. Snarls and tangles with leads are common even when your operating space is immaculately organised, and the nurse can assist with this and the cleaning of diathermy tips if on the same side as the surgeon.
Diathermy pedals
Most cases will require the core unipolar pedal together with a bipolar button. The unipolar pedal should be positioned on the floor below the patient’s hip joint, as close as possible to the table without getting caught beneath. The bipolar button, however, should be against the unipolar pedal but on its lateral side, or it will be caught under the table when you need it most! Both pedals should be within natural, easy reach and should have sufficient tactile properties to be activated without needing to look.

Alertness, performance and body temperature
Body and ambient temperature are closely aligned to performance of cognitive and fine motor tasks.15 Performance is best with a body temperature just above 37, and an ambient temperature of 22°C.
Instrument design
Angle between instrument handle and shaft for complex laparoscopic suturing
Ahmed et al16 demonstrated that the optimal angle of handle to shaft for bowel suturing is 40 degrees. This outcome was determined through objective analysis of suture accuracy, together with leak pressure of bowel repairs. Bear in mind that we use a large variety of needles in gynaecology and, so, just as with open surgery, we will need a variety of needle drivers. Fine angled needle drivers as above are not suitable for closing a vaginal vault.
Handle design
The design of laparoscopic instruments over the last 10–20 years has invariably concentrated on the ringed, pistol grip handle with a round, rotating shaft and a single- or double-action grasping tip. Gutierrez Diez17 demonstrated that laparoscopic instruments require 3–5 times the muscle contraction force of open instruments, due to a 3–6 times less efficient transfer of energy. In addition, there is a decreased efficiency of grip due to wrist flexion and ulnar deviation imposed by pistol grip design. The rings themselves are, with few exceptions, not designed to accommodate the surgeon’s hands, leading to excessive pressure in use.
Where to from here?
Although the past two decades have seen enormous industry- and clinician-led strides in energy sources and particularly microprocessor technology, most mechanical laparoscopic instruments have developed little. We need to pursue instruments with contact surfaces of a design enabling light contact with optimal energy transmission, different sizes for different surgeons’ hands (both male and female) and, most importantly, operating tables designed for laparoscopic surgery. The most obvious improvement will be tables enabling a suitably low operating height so that we can discard the humble chequer plate step.
References
- U Matern, P Waller, K Giebmeyer, et al. Ergonomics: requirements for adjusting the height of laparoscopic operating tables. JSLS. 2001;5(1):7-12.
- C Alleblas, A De Man, L Van Den Haak, et al. Prevalence of musculoskeletal disorders among surgeons performing laparoscopic surgery. Ann Surg. 2017;266:905-20.
- European Agency for Safety and Health at Work. OSH in figures: work related musculoskeletal disorders in the EU – facts and figures. 2010. Available from: https://osha.europa.eu/en/tools-and-publications/publications/reports/TERO09009ENC.
- H Berguer, A Hreljac. The relationship between hand size and difficulty using surgical instruments: a survey of 726 laparoscopic surgeons. Surg Endosc. 2004;18:508-12.
- U Matern, P Waller, K Giebmeyer, et al. Ergonomics: requirements for adjusting the height of laparoscopic operating tables. JSLS. 2001;5(1):7-12.
- GK Cass, S Vyas, V Akande, et al. Prolonged laparoscopic surgery is associated with an increased risk of vertebral disc prolapse. J Obstet Gynecol. 2014;34:74-8.
- A Zihini, J Cavallo, S Ray, et al. Ergonomic analysis of primary and assistant surgical roles. J Surg Res. 2016;203(2):301-5.
- R Berguer, W Smith. An ergonomic comparison of robotic and laparoscopic technique: the influence of surgeon experience and task complexity. J Surg Res. 2006;134:87-92.
- M Ayoub. Workplace design and posture. Human Factors. 1973;15:265-68.
- U Matern, P Waller, K Giebmeyer, et al. Ergonomics: requirements for adjusting the height of laparoscopic operating tables. JSLS. 2001;5(1):7-12.
- U Matern, P Waller, K Giebmeyer, et al. Ergonomics: requirements for adjusting the height of laparoscopic operating tables. JSLS. 2001;5(1):7-12.
- MA Van Veelen, G Kazemeir, J Koopman, et al. Assessment of the ergonomically optimal operating surface height for laparoscopic surgery. J Laparoendosc Adv Surg Tech A. 2002;12(1): 47-52.
- M Van Det, H Meijerink, C Hoff, et al. Optimal ergonomics for laparoscopic surgery in minimally invasive surgery suites: a review and guidelines. Surg Endosc. 2009;23:1279-85.
- M Van Det, H Meijerink, C Hoff, et al. Optimal ergonomics for laparoscopic surgery in minimally invasive surgery suites: a review and guidelines. Surg Endosc. 2009;23:1279-85.
- KP Wright, JT Hull, CA Czeisler. Relationship between alertness, performance, and body temperature in humans. Am J Physiol Regul Integr Comp Physiol. 2002;283(6):R1370-7.
- S Ahmed, G Hanna, A Cuschieri. Optimal angle between instrument shaft and handle for laparoscopic bowel suturing. Arch Surg. 2004;139(1):89-92.
- MC Gutierrez-Diez, MA Benito Gonzalez, R Sacibrian, et al. A study of the prevalence of musculoskeletal disorders in surgeons performing minimally invasive surgery. Int J Occup Saf Ergon. 2018;24(1):111-7.





Leave a Reply