There is a saying that if you only have a hammer, every problem looks like a nail. While this is not true in most circumstances, when it comes to the issues that are problematic in the theatre environment, it might truly be said that for every problem that might arise, there is a simulation-based solution. From surgical rehearsal to demonstration of competence, from team communication to environmental hazard identification, simulation is playing an increasingly important role in both training and improving patient safety in theatre for procedures in gynaecology and in obstetric surgery.
Simulation and surgical skills training
The use of simulation as an education tool to assist in the gaining of surgical competency is very well established. In gynaecological laparoscopy, improvements in performance have been demonstrated with virtual reality simulators1 and with simple box trainers.2In addition to laparoscopic skills, simulation has been shown to improve confidence and performance in hysteroscopy,3 cervical surgery4 and even vaginal hysterectomy.5 The argument is no longer whether or not trainees need exposure to simulation trainers, it has become whether or not trainees must demonstrate competency on a simulator before being permitted to perform specific procedures on real patients. If training time is not mandated, trainees fail to complete simulation training programs, despite being aware of the likely benefits to their own skills and practice.6 This is possibly due to the pressure on trainees to complete other activities, and to prioritise clinical work over education time, with resource allocation and adequate funding a clear potential barrier. Preshaw et al interviewed patients and hospital managers in the UK and concluded that mandatory demonstration of competency using simulation was supported by these two groups of stakeholders, despite the identification by the managers of resource conflicts between clinical and educational equipment and time.7
In Australia and New Zealand there is not yet a standardised approach to surgical simulation training, although the picture is rapidly evolving. In 2016, 87 per cent of trainees had access to simulation, but few training programs had a simulation curriculum or adequate supervision.8 Reports to the RANZCOG Simulation Training Advisory Group (STAG) this year suggest that laparoscopic simulation curriculums are in use in Queensland, New Zealand and Western Australia. In some units, trainees are not permitted to perform laparoscopic surgery as the primary operator unless they are up to date with their laparoscopic simulation training competencies, and it is likely that this approach will become standard practice.
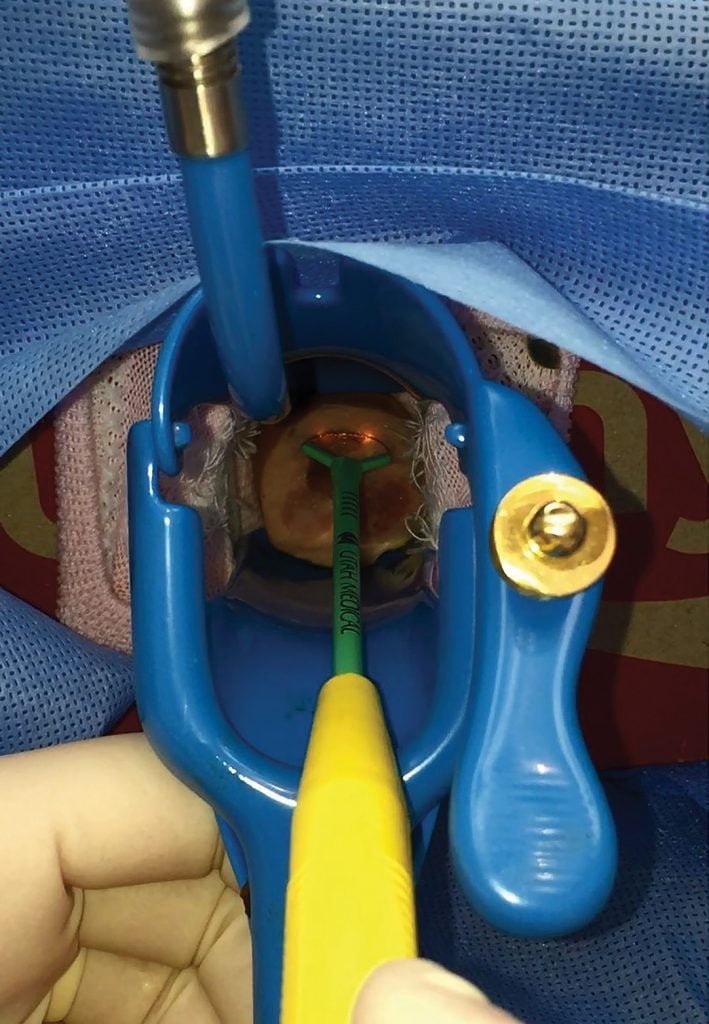
Figure 1. Surgical simulation for skills in LLETZ procedure.
Simulation can also be used to rehearse rare, or even unique, patient-specific procedures. In 2016, a team from the Mater Mother’s Hospital undertook Australia’s first full procedure simulation for in-utero spinal surgery on a 24-week-old in-utero baby with spina bifida.9The simulation included teams from the Vanderbilt University Hospital and the Mater, allowing the identification of differences in surgical terminology, including instrument names between the Australian and American teams, and improving procedural familiarity and safety prior to operating on a real patient. Simulation has also been used to create 3D patient-specific models for surgical rehearsal, allowing theatre warm-up and practice with no deficit in patient care,10 although this application has yet to become widespread in gynaecological surgery.
Simulation for communication skills in theatre
Non-technical skills are highly relevant to the theatre environment. Failure in communication leads directly to poor outcomes in theatre, and communication skills of theatre team members are directly related to speed of crisis resolution in the theatre environment.11 In a 2017 study, a team from Harvard used standardised ratings tools for non-technical skills to test the correlation between the nontechnical skills of surgeons and anaesthetists and time of resolution of two theatre emergencies: intraoperative haemorrhage causing haemodynamic instability and difficult airway resulting in hypoxia.12 Higher non-technical skill ratings resulted in significantly faster crisis resolution in both scenarios. The clinical relevance of both of these simulated situations to the obstetric surgical setting is obvious.
Simulation training has also been associated with improved empathy for patients in the theatre setting.13 The operating theatre is a highly technical environment, which patients can find distressing and anxiety-provoking. Simulation and roleplay are effective tools to increase the empathy scores of healthcare providers working in theatres. Again, the relevance to the theatre setting of obstetrics and gynaecology is obvious.

Figure 2. Testing new processes and team coordination in the operating room.
Teamwork and leadership skills are essential components of non-technical skills. Simulation has been shown to be a useful way to assess leadership in emergency situations that might arise in the theatre setting, including postpartum haemorrhage in obstetrics.14 A recent study of leadership utterances in this setting showed that leadership is commonly shared in this clinical scenario, in contrast to the commonly held perception of singular leadership by the senior surgeon or obstetrician.15 It may be that simulation will prove to be a useful way of improving teamwork and leadership skills in the specific arena of the operating theatre; the international ViSIOT (Video-Supported Simulation of Interactions in the Operating Theatre) currently underway will seek to address this exact question.16
Conclusion
Simulation can never truly be the answer to all the difficulties encountered in the complex, high-stress and rapidly expanding arena of the operating theatre. It can, and must, play a part in improving the training and skills of all members of the operating theatre team, and in the planning and execution of the complex pathways undertaken by patients journeying into that environment. Properly applied with due consideration, simulation has the potential to improve outcomes and enhance patient safety – a goal for all stakeholders in this space.
References
- C Burden, T Appleyard, J Angouri, et al. Implementation of laparoscopic virtual-reality simulation training in gynaecology: a mixed-methods design. Eur J Obstet Gynecol Reprod Biol. 2013;170(2):474-9.
- E Wilson, S Janssens, LA McLindon, et al. Improved laparoscopic skills in gynaecology trainees following a simulation-training program using take-home box trainers. ANZJOG. 2019;59(1):110-16.
- B Rackow, J Solnik, F Tu, et al. Deliberate Practice Improves Obstetrics and Gynaecology Residents’ Hysteroscpoy Skills. J Grad Med Educ. 2012;4(3):329-34.
- E Wilson, S Janssens, D Ng, et al. Trainee Performance in Loop Electrosurgical Excision Procedure (LEEP) After Simulation Training. Journal of Lower Genital Tract Disease. 2019;23;1:28-32.
- J Greer, S Segal, C Salva, L Arya. Development and Validation of Simulation Training for Vaginal Hysterectomy. J Minim Invasive Gynecol. 2014;21(1):74-82.
- C Burden, T Appleyard, J Angouri, et al. Implementation of laparoscopic virtual-reality simulation training in gynaecology: a mixed-methods design. Eur J Obstet Gynecol Reprod Biol. 2013;170(2):474-9.
- J Preshaw, D Siassakos, M James, et al. Patients and hospital managers want laparoscopic simulation training to become mandatory before live operating: a multicentre qualitative study of stakeholder perception. BMJ Stel. 2019;5:8-14.
- Mater Education. Mater Education leads Australian first surgery simulation. 2016. Available from: www.matereducation.qld.edu.au/News/Mater-Education-leads-Australian-first-surgery-sim.
- M Russon. Surgeons Use 3D Printing to Remove Previously Inoperable Tumour from Child. 2014. Available from: www.ibtimes.co.uk/surgeons-use-3d-printing-remove-previously-inoperable-tumour-child-1455181.
- E Wilson, S Janssens, DG Hewett, et al. Simulation training in obstetrics and gynaecology: What’s happening on the frontline? ANZJOG. 2016;56(5):496-502.
- N Nguyen, W Watson, E Dominguez. Simulation-Based Communication Training for General Surgery and Obstetrics and Gynecology Residents. Journal of Surgical Education. 2019;76(3):856-63.
- N Nguyen, W Watson, E Dominguez. Simulation-Based Communication Training for General Surgery and Obstetrics and Gynecology Residents. Journal of Surgical Education. 2019;76(3):856-63.
- N Larti, E Ashouri, A Aarabi. The effects of an empathy role-playing program for operating room nursing students. J Educ Eval Health Prof. 2018;15:29.
- S Janssens, R Simon, S Barwick, et al. Leadership sharing in maternity emergency teams: a retrospective cohort study in simulation. BMJ Stel. 2019. doi:10.1136/bmjstel.2018.000409.
- S Janssens, R Simon, S Barwick, et al. Leadership sharing in maternity emergency teams: a retrospective cohort study in simulation. BMJ Stel. 2019. doi:10.1136/bmjstel.2018.000409.
- S Weldon, T Korkiakangas, J Calzada, et al. A Surgical Team Simulation to Improve Teamwork and Communication across Two Continents: ViSIOT Proof-of-Concept Study. J Surg Educ. 2019. doi: 10.1016/j.jsurg.2019.03.016.







Leave a Reply