Mrs T, 24-year-old, G1P0 presented at 33+2 weeks with nausea, vomiting, hypertension, anxiety and intermittent oedema of the hands and feet. She denied headache, blurry vision and abdominal pain.
Her blood pressure was 206/90 mmHg (repeat measurements were 125–135/80–88 mmHg) and pulse was 113–131 bpm. She had no oedema, no clonus and reflexes were normal. Her blood investigations were normal but her protein creatinine ratio (PCR) was elevated at 134.9 mg/mol.
The working diagnosis was preeclampsia. She was started on labetalol 100 mg TDS. She required multiple stat doses of nifedipine for labile blood pressure and was eventually controlled on labetalol 200mg mane, midi and 300mg nocte. An oral glucose tolerance test later confirmed gestational diabetes and the fetus plotted above the 95th percentile.
The patient was discharged home on labetalol with a follow up appointment made to see in clinic.
Mrs T was re-admitted at 35+0 weeks with worsening blood pressure (175/101 mmHg) and symptoms of sweating and vomiting.
The patient had systolic blood pressures between 200–210 mmHg (unresponsive to nifedipine) and an intermittent sinus tachycardia. Further questioning revealed a history of nausea, vomiting, anxiety, palpitations, fainting episodes and episodic headaches for close to a year. As a result, further imaging was requested, with strong clinical suspicion for pheochromocytoma by the visiting endocrinologist. (Endocrinology were reviewing the patient routinely for management of gestational diabetes). An urgent ultrasound scan revealed a right sided 9x8x11cm suprarenal mass and further blood investigations showed elevated plasma metanephrines (184396 pg/mL). Mrs T was transferred to the high dependency unit and started on intravenous hydralazine and labetalol for blood pressure control and magnesium sulphate infusion for eclampsia prevention. She had slightly deranged liver function tests (ALT 69 U/L, AST 73 U/L). The patient was advised to stay in the left lateral position and plan was made to avoid unopposing B blockade.
The working diagnosis at this stage was pheochromocytoma with superimposed preeclampsia. She was transferred to the intensive care unit (ICU) overnight for alpha blockade with Doxazocin and closer monitoring.
The multidisciplinary team decided to deliver the next day via emergency lower segment caesarean section under general anaesthesia at 35+6 given suboptimal control of blood pressure in pregnancy.
The procedure was uneventful and great care was taken to reduce the pressure exerted on the catecholamine secreting tumour. The patient was transferred to ICU for ongoing transition to oral alpha blockade. The neonate required continuous positive airway pressure immediately after delivery for tachypnoea. The fetus continued to have episodes of desaturation and bradycardia. It was thought this may be due to the doxazocin from the breastfeeding mother. The episodes resolved once the neonate was switched to formula feeds.
Mrs T was transitioned back to the ward and eventually discharged on oral Doxazocin 7mg twice daily. She was advised to increase fluid and salt intake.
Two months later, she had an uncomplicated elective transperitoneal laparoscopic excision of the pheochromocytoma. The histology confirmed the presence of a right adrenal gland tumour–pheochromocytoma (stage-pT2 NX). Mrs T reports immense relief and the anxiety she experienced for close to a year has since resolved.
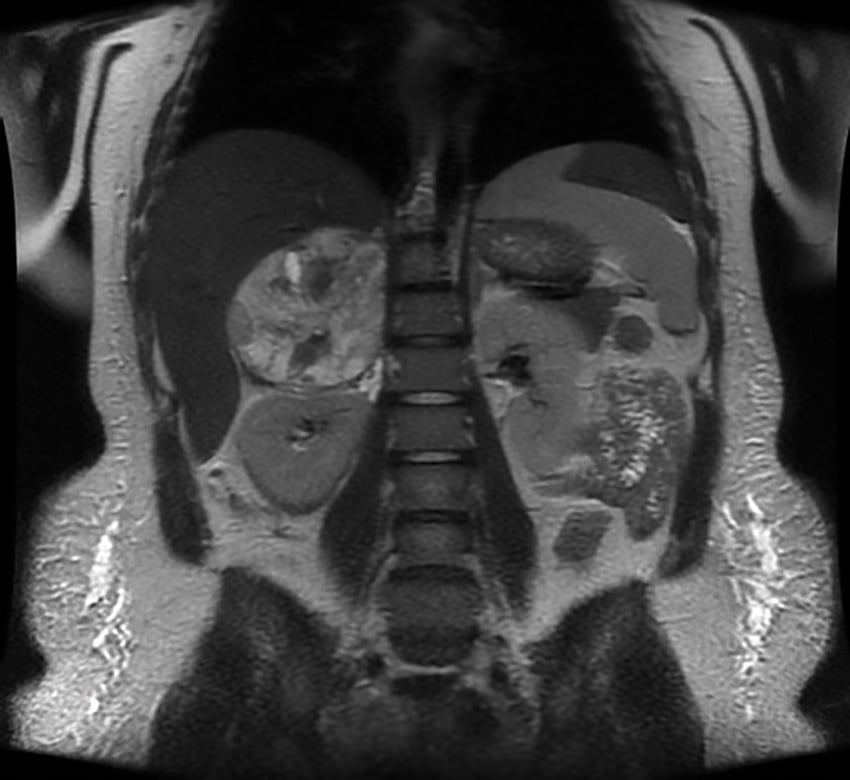
Figure 1. Postpartum MRI of neck, chest abdomen and pelvis, showing a large mass arising in the region of the right adrenal gland (consistent with a phaeochromocytoma). It abuts a number of adjacent structures but does not obviously appear to be invading any of these structures. No evidence of any metastatic disease identified within the abdomen. No obvious evidence of any other masses identified other than the patient’s physiologically enlarged postpartum uterus.
Discussion
Hypertension is a common complication in pregnancy, occurring in 5–10% of all cases.1 It is difficult to differentiate more common causes of hypertension in pregnancy such as chronic hypertension and pregnancy related hypertension (preeclampsia and gestational hypertension) from pheochromocytoma that has a much lower incidence of 0.007%.2
Advancing pregnancy intensifies symptoms of pheochromocytoma due to the increased pressure on the abdomen, fetal movements and uterine contractions. Oestrogens may also act as a growth factor for adrenal tumors.3
Associated features such as hyperglycemia and cardiomyopathy along with headaches, palpitations and sweating may direct the clinician towards pheochromocytoma over hypertension accompanied by proteinuria and oedema which is more in keeping with preeclampsia.
Our patient developed superimposed preeclampsia, which complicated her initial presentation and delayed diagnosis of the pheochromocytoma. She did not exhibit signs of preeclampsia such as, brisk reflexes, or clonus however she had a raised PCR and later, mildly elevated liver function tests. Careful history taking may have led to an earlier diagnosis of pheochromocytoma, though we appreciate the complexity in our patient’s presentation and difficultly to differentiate the two conditions.
In normal pregnancy, metabolism of catecholamines is unaltered. In those with preeclampsia, plasma catecholamine levels can be slightly elevated. If patients are using methyl dopa or labetalol, these medications can lead to false positive results.4 For this reason, imaging studies such as magnetic resonance imaging and ultrasound scans are useful to confirm diagnosis and localise the tumour in pregnancy.
| Preeclampsia | Pheochromocytoma | |
| Symptoms | Headache Blurry vision Abdominal pain Swelling of hands, feet and face |
Nausea Sweating Palpitations ‘Spells’ |
| Onset | Gradual After 20 weeks gestation |
Sudden May have symptoms prior to pregnancy or in first 20 weeks Worsens with pregnancy |
| Signs | Clonus Brisk reflexes Pitting oedema |
Tachycardia, paroxysmal hypertension, orthostatic hypotension |
| Associations | Intrauterine growth restriction | Gestational diabetes Superimposed preeclampsia Cardiomyopathy |
| Investigations | Raised liver function tests Raised creatinine Raised protein creatinine ratio Lowered platelets Lowered haemoglobin |
Raised plasma metanephrines Ultrasound scan or MRI reveals adrenal mass |
Genetic testing is considered after diagnosis and can be considered during follow up. As patients diagnosed in pregnancy are typically young, they may be more likely to carry a genetic mutation.
Alpha adrenergic receptor blockade with Phenoxybenzamine or doxazocin for 10–14 days before surgery is advised to reduce perioperative and postoperative complications.5
Doxazocin is now preferred over Phenoxybenzamine because there is less reflex tachycardia and postoperative hypotension. Neonatal hypotension and respiratory depression have not been described (though it may cross the placenta). One case report testing for doxazosin levels in human breast milk has been conducted with low levels recorded.6 We are unsure if the bradycardia and desaturations described in our case were related to doxazocin.
Our patient developed hypertensive crisis as treatment with labetalol alone led to unopposed alpha adrenoceptor stimulation. Beta adrenergic receptor blockade should be considered after alpha blockade to counteract catecholamine-induced tachyarrhythmia and alpha receptor blockade induced reflex tachycardia.7
If diagnosed in the first 24 weeks and there is sufficient alpha blockade, surgery should be undertaken laparoscopically to remove the tumor in the second trimester.8 In the third trimester, it is advised to wait until after delivery as the gravid uterus makes accessing tumor difficult.
A transperitoneal approach is advised in pregnancy. A left lateral approach is advised if right sided tumor. If left sided tumor, a right lateral approach should be undertaken with care given compression to the vena cava and a theoretical risk of uteroplacental hypoperfusion. Our patient was diagnosed in the third trimester when it was not advised to perform a resection. She was positioned in the left lateral side during cesarean delivery and care was taken to avoid manipulation of the tumor.
Mrs T had general anaesthetic with deep total intravenous anaesthetic and bispectral index monitoring. A central venous pressure line was inserted while under anaesthetic. Gentle oxytocin was given while ergometrine, carbaprost and misoprostol were avoided. Literature reports epidural, spinal and combined anesthetic techniques are safe.9 Postsurgical complications involve hypotension and hypoglycaemia, which our patient fortunately did not experience.
Most reports advocate for caesarean delivery; however, recent case studies have shown safe vaginal delivery is possible when adequate epidural analgesia is administered. It may be more favourable in multiparous women whom have had a prior successful vaginal delivery and experience a shorter second stage of labour.10 There is no clear evidence to guide the best time and mode of delivery. A multi-disciplinary team approach should be adopted in determining mode and timing of delivery.
Conclusion
Pheochromocytoma in pregnancy is a potentially fatal condition. With increasing awareness and understanding of safe management options, outcomes have improved over the last decade.
Acknowledgements
Dr Richard Foon, Dr Sylvia Lin, the Waikato Women’s Health department and the Waikato Anesthetic department.
References
- Vest A, Cho L. Hypertension in Pregnancy. Curr Atheroscler Rep. 2014 Mar;16(3):395
- Harrington J, Farley D, van Heerden J, Ramin K. Adrenal tumors and pregnancy. World Journal of Surgery. 1999;23(2):182-6.
- Isoda H. Phytoestrogens genistein and daidzin enhance the acetylcholinesterase activity of the rat pheochromocytoma cell line PC12 by binding to the estrogen receptor. Cytotechnology. 2002;40(13):117-23.
- Feingold KR, Anawalt B, Boyce A, et al. Endotext 2013. Available from: www.ncbi.nlm.nih.gov/books/NBK278970/table/pheochromocytoma.table4drug/
- Prete A, Paragliola R, Salvatori R, Corsello S. Management of catecholamine secreting tumors in pregnancy. Endocr Pract. 2016;22(3):357-70.
- Jensen B, Dalrymple J, Begg E. Transfer of Doxazosin into Breast Milk. Journal of Human Lactation. 2013;29(2):150-53.
- Prete A, Paragliola R, Salvatori R, Corsello S. Management of catecholamine secreting tumors in pregnancy. Endocr Pract. 2016;22(3):357-70.
- Prete A, Paragliola R, Salvatori R, Corsello S. Management of catecholamine secreting tumors in pregnancy. Endocr Pract. 2016;22(3):357-70.
- Prete A, Paragliola R, Salvatori R, Corsello S. Management of catecholamine secreting tumors in pregnancy. Endocr Pract. 2016;22(3):357-70.
- Prete A, Paragliola R, Salvatori R, Corsello S. Management of catecholamine secreting tumors in pregnancy. Endocr Pract. 2016;22(3):357-70.





Leave a Reply