Almost every area of medical practice displays some uniquely idiosyncratic use of language. However, it’s likely that pathology has the largest collection of curious culinary expressions, which most practitioners probably recall from their student days. Once upon a time, it was an annual ritual for medical students to concoct the best possible menu from pathology ‘ingredients’ … anchovy sauce pus or currant jelly clots, anyone?
Some of the quaint food/cookbook terms refer to macroscopic appearances such as the ‘cheesy’ (feta, not cheddar!) appearance of caseous necrosis in tuberculosis (Figure 1A). Others describe microscopic patterns such as ‘coffee bean’ nuclei in granulosa cell tumours (Figure 2A). Many of these archaic descriptions are sufficiently odd that they are at least memorable, so they serve some educational purpose. However, a number make little sense these days, especially to urban medical students. UNSW graduates might recall that the university’s Museum of Human Disease has a specimen of the polished surface of a cut nutmeg next to a specimen of chronic passive venous congestion of the liver, to help explain the origins of the term ‘nutmeg liver’ (Figure 1B). Or they might remember a specimen of millet seeds, relevant to the phrase ‘miliary tuberculosis’ which is still used to indicate the size of the individual lesions in massive haematogenous dissemination of tuberculosis (Figure 1C).
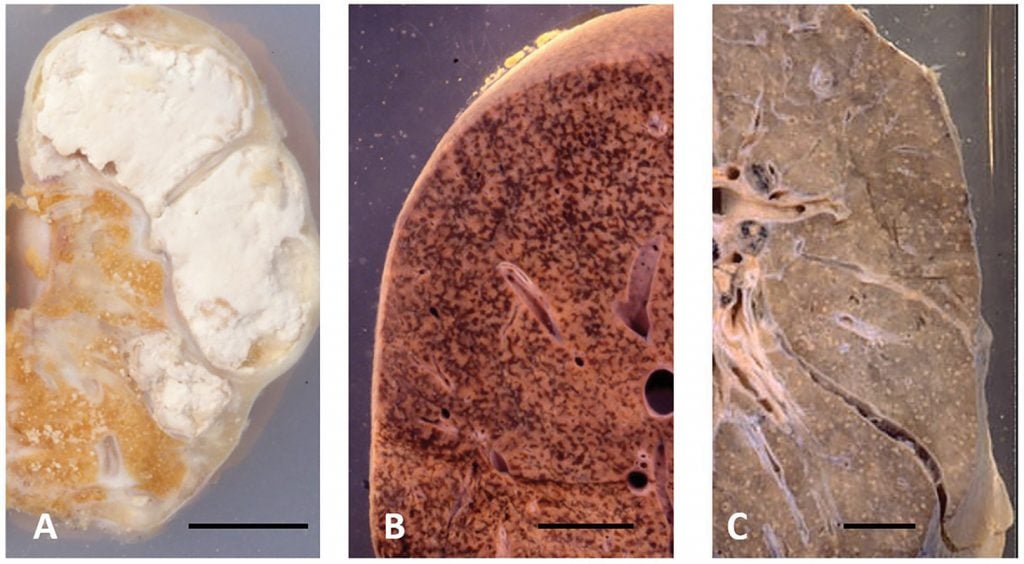
Figure 1. Macroscopic specimens illustrating changes traditionally described using food-related terminology:
(A) severe renal tuberculosis demonstrating replacement of the parenchyma of the kidney by white, crumbly necrotic material, described as ‘cheesy’ or caseous necrosis. (B) chronic passive venous congestion of the liver, for which the time-hallowed descriptor is ‘nutmeg liver’. (C) hundreds of ~1mm ‘miliary’ lesions distributed throughout the lung parenchyma in massive haematogenous dissemination of tuberculosis. Bar = 25 mm.
Food-related descriptions of pathological changes were reviewed in an article in the BMJ over 40 years ago.1 More recently, a list of food-related terms used across a variety of areas of clinical practice was reported in the American Journal of Medicine.2 This seemed to suggest that ophthalmology might be almost as enthusiastic about culinary comparisons as pathology! In another recent article, the authors compiled a glossary of over 100 food-related terms used in medical practice.3
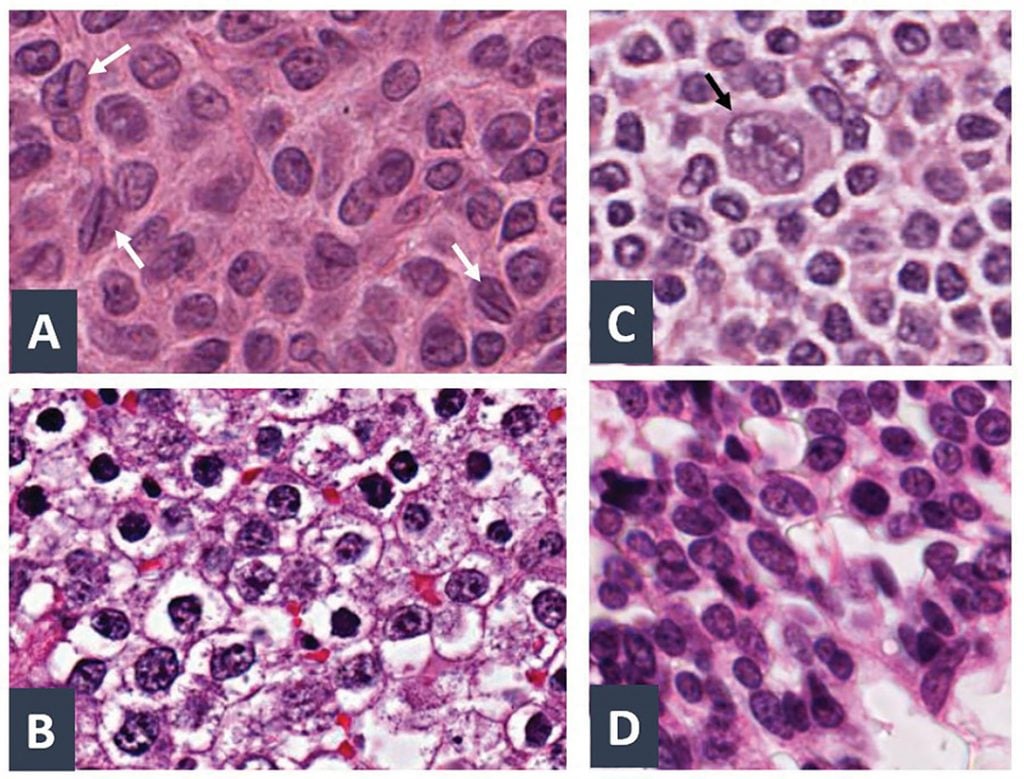
Figure 2. High-magnification photomicrographs illustrating cell nuclei traditionally described using food-related terminology: (A) ‘coffee bean’ nuclei in a granulosa cell tumour – the longitudinal groove in some of the nuclei (white arrows) yields an appearance thought to resemble a coffee bean. (B) ‘fried egg’ nuclei in a seminoma of the testis. (C) ‘popcorn’ nucleus (black arrow) of a malignant cell in lymphocytic predominance Hodgkin’s lymphoma. (D) hyperchromatic nuclei in cells with a high nucleus:cytoplasm ratio in small cell anaplastic carcinoma of the lung, thought to resemble oat grains, hence the designation ‘oat cell’ carcinoma.
Nevertheless, the inclusion of food-related terms in internationally distributed textbooks can be a source of much confusion, notably for students in parts of the world where the foods being referred to are not grown or consumed. As was pointed out in an article published some 20 years ago, ‘strawberry haemangioma’ conveys little meaning to an African medical student who has never seen a strawberry.4
Perhaps the time has come to think about the language of pathology in modern terms, rather than romanticising ‘bread-and-butter pericarditis’ or ‘sugar-icing spleen’. Pathologists are first and foremost the scientists of medical practice, who take pride in their laboratories being able to perform diagnostic assessments with precision and reproducibility – something for which we can be very grateful in these COVID-afflicted times. Ongoing discussions about COVID mean that terminology related to the modelling of epidemics has probably found its way into your everyday language. However, many medical practitioners still do not think of the sensitivity and specificity of diagnostic tests, or of their positive and negative predictive values, as fundamental to the practice of medicine and the interpretation of reports provided by pathologists. We should.
While we are on this topic, I would like to mention my pet peeve with respect to the use of language about pathology. Please don’t let me ever hear you ask about ‘the pathology in this patient’. Pathology is a science, not a disease. There is an abnormality, a pathological process, a disease, a lesion or lesions … but unless the patient has swallowed a copy of a textbook, there is no pathology in the patient!
Our feature articles represent the views of our authors and do not necessarily represent the views of the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG), who publish O&G Magazine. While we make every effort to ensure that the information we share is accurate, we welcome any comments, suggestions or correction of errors in our comments section below, or by emailing the editor at [email protected].
References
- Terry SI, Hanchard B. Gastrology: the use of culinary terms in medicine. Br Med J. 1979;2(6205):1636-9.
- Mark NM, Lessing JN, Buckley SA, Tierney LM. Diagnostic utility of food terminology: culinary clues for the astute diagnostician. Am J Med. 2015;128(9):933-5.
- Vimal M, Nishanthi A. Food eponyms in Pathology. J Clin Diagn Res. 2017;11(8):EE01–6.
- Ahmed H, Ogala WN, Ibrahim M. Culinary metaphors in Western medicine: a dilemma of medical students in Africa. Med Educ. 1992;26(5):423-4.





Leave a Reply