The veterinarian team at the Auckland Zoo approached us, and asked for our assistance with a special project, involving a primate under their care. Kera is a 17-year-old female Siamang gibbon (Symphalangus syndactylus) bred in captivity and currently living at the Auckland Zoo. Kera and her mate Intan have had two pregnancies, both sadly ending in stillbirth secondary to labour dystocia, necessitating midline laparotomy and caesarean section.

Figure 1. Kera and her mate, Intan.
Following Kera’s last pregnancy, contraception cover has been maintained by the zoo keepers, disguising the combined oral contraception pill (Marvelon: desogestrel 0.15mg, ethinyloestradiol 0.03mg) in her food, and the contraceptive implant (Jadelle: levonorgestrel-releasing implant 75mg). Given Kera’s poor obstetric history, the vet team wanted to explore permanent sterilisation via a minimally invasive surgical approach. Our team, made up of two gynaecology consultants experienced in laparoscopic surgery, and a Fellow, jumped at the chance to help.

Figure 2. Kera’s obstetric abdominal x-ray.

Figure 3. Vet team inserting IV access, shave, scrub,
and bedside ultrasound scan.
Pre-operative preparation
Kera was kept nil by mouth with no access to food in her enclosure overnight, but had access to water up to 15 minutes before administration of intramuscular sedation. This was delivered by blowpipe dart and contained a combination of ketamine and medetomidine. To facilitate safe transfer from her enclosure to the zoo’s on-site veterinary hospital, Kera was intubated with an endotracheal tube, and anaesthesia was initiated with inhaled isoflurane. On arrival to the hospital, intravascular access was established with cannulas inserted into the left and right cephalic veins.
Kera’s abdomen was prepared by shaving and a thorough scrub. Bedside ultrasound scan confirmed an empty uterus (positive endometrial stripe) and therefore excluded a current pregnancy. Socks were placed over her hands and feet for the purpose of thermoregulation. Kera was then positioned on the operating table in dorsal recumbent and draped exposing the entire abdomen, in the event that conversion to laparotomy was required.
Insertion of a urinary catheter was avoided due to the altered location of the urethra in primates, within the anterior vaginal wall, making catheterisation very challenging. We also decided against uterine instrumentation for the purposes of manipulation. Again, this was due to the small female primate reproductive tract (vagina, endocervical canal and uterus), which would be associated with high risk of injury.
Monitoring and anaesthesia
Intra-operative anaesthesia maintenance was provided by inhaled isoflurane and occasional IV ketamine boluses. Maintenance intravenous fluids were provided by Ringer’s lactate, and inotropic support by a dopamine infusion. Additional analgesia was provided through a single dose of IV paracetamol and continuous remifentanil infusion. Intra-operative monitoring was achieved by a combination of non-invasive blood pressure, temperature via rectal probe, electrocardiogram, doppler heart rate monitoring and end-tidal carbon dioxide. Kera was mechanically ventilated throughout the procedure. A dose of IV cefazolin was also given intra-operatively as infection prophylaxis.
Laparoscopy
A well-healed sub-umbilical midline laparotomy scar was noted. Hasson entry was performed by making a 5mm incision to the umbilicus, the fascia exposed, grasped, and elevated with artery clips. The fascia was then incised and entry gained to the peritoneal cavity. A 5mm port was inserted and laparoscope introduced to confirm correct placement with the presence of intra-peritoneal structure (omentum). An insufflation tube carrying carbon dioxide was then attached and pneumoperitoneum established at 7-8 mmHg (paediatric pressures). The operating table was then tilted into the reserve Trendelenburg position to allow for the displacement of the bowel out of the pelvis.
During secondary port site placement, the anterior abdominal wall was inspected, and the inferior epigastric artery and vein identified, with ports placed lateral to these vessels. The skin, muscular and fascial layers were incised with a scalpel, track open with an artery clip and 5mm ports then inserted to the left and right lower quadrants under direct vision.
Examination of the abdomen and pelvis identified normal upper abdominal structures, liver and stomach. The presence of omental adhesions was identified to the uterine fundus, bladder, left adnexa and anterior abdominal wall – most likely the result of Kera’s two previous laparotomies. Adhesiolysis was preformed using a combination of sharp dissection with laparoscopic scissors and an advance bipolar sealing device. An additional 5mm suprapubic port was required to displace the prominent urinary bladder.

Figure 5. Omental adhesion to uterine fundus, uterus, left fallopian tube and ovary.
When access to the pelvis was confirmed, and the fundus of the uterus exposed, both fallopian tubes were then identified by confirming the presence of the fimbria. Salpingectomy was preformed using an advanced bipolar sealing device, starting at the fimbria and moving proximal towards the uterus, ensuring no tubal stump was left behind, to prevent future ectopic (interstitial) pregnancy. The specimen was then sent for histology. The pedicle was inspected for haemostasis. The procedure was then repeated on the contralateral side without complication.
At the completion of the procedure, ports were removed under direct vision and pneumoperitoneum was expelled. The fascia at all four port sites was closed with interrupted 3.0 PDS to reduce hernia risk. Skin was again closed with interrupted 3.0 PDS and knots were buried to minimise Kera picking at, and pulling out, the sutures.
- Laparoscope (30-degree 5mm)
- Light cable
- Insufflation tubing
- Carbon dioxide cylinder
- Automatic insufflator
- Visual display screen
- Ports (4 x 5mm)
- Advance bipolar sealing device
- Laparoscopic instruments
- Bowel graspers, Maryland, scissors
- Operating table
- Laparotomy tray
Post operative recovery
Kera was kept in her indoor enclosure for a 14-day post-operative period. She received regular paracetamol and meloxicam (NSAID) as analgesia, and made a speedy recovery. Combined oral contraception was continued until histology returned confirming salpingectomy.

Figure 4. Post-operative with diamond shaped laparoscopy incisions.
Discussion
Given Kera’s poor obstetric history, the zoo’s vet team understandably wanted to avoid her breeding again, so the indication for permanent sterilisation was clear. The questions asked of our team were: What is the best way to achieve this in a primate? Was this possible via a minimally invasive surgical approach?
Advantages of laparoscopy over traditional open procedures (laparotomy) are well established and extensively described in medical (human) literature. Advantages include reduced rates of wound complications, decreased postoperative pain, and shorter hospital stay and recovery. It is for these reasons that laparoscopy is considered the gold-standard for most major gynaecological procedures in humans. Given similarities of size, anatomy, physiology and disease pathology with our closest relatives, primates like our friend Kera also stand to benefit from a laparoscopic procedure.
Review of the veterinary literature indicates that laparoscopic surgery in primates was first described in the 1970s. Subsequently, laparoscopic sterilisation in wild primate populations for the purposes of population control, particularly in Macaques (Macaca) species throughout Southeast Asia, has been well described.1 2 3 4 5
Surprisingly, the same cannot be said for captive primates, with only one case report of laparoscopic sterilisation available in the current literature. Ruby, a 21-year-old female chimpanzee (Pan troglodytes), underwent laparoscopic tubal ligation (modified pomeroy technique) at the North Carolina Zoo (2019).6 To date, laparoscopic procedures in primates have been extrapolated from the standard human experience. Our team encountered some limitations to this one-size-fits-all approach, and these are discussed below.
The female pelvic anatomy of primates is surprising similar to humans, but there is one obvious difference and that is the urinary bladder. In humans, this is an extraperitoneal structure, but in primates (and in Kera’s case) the bladder is intraperitoneal. This anatomical difference presented a challenge, with the prominent bladder inhibiting surgical access. This issue was exacerbated by our inability to drain the bladder.
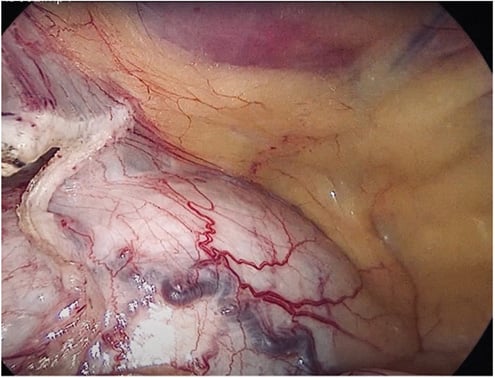
Figure 6. Distended intraperitoneal urinary bladder (post adhesiolysis).
After some troubleshooting, we solved the issue by inserting an additional 5mm suprapubic port. With the help of a laparoscopic instrument, we were able to displace the bladder enough to access pelvic structures.
Another option would be suprapubic catheterisation. In addition to issues created by the bladder, gynaecologists (and gynaecologists in training) would be very much aware of the importance of uterine manipulation when preforming pelvic surgery in humans. Despite this, as a team, we made the conscious decision to avoid uterine instrumentation to eliminate the risk of trauma to the reproductive tract, or uterine perforation.
Our team anticipated that Kera’s size would present a challenge, given that at 15kgs, she was much smaller than our usual patient demographic of adult female humans. We consulted a paediatric surgeon as part of the surgical planning process who provided invaluable advice about laparoscopic surgery in little people.
In addition to Kera’s size, the anterior abdominal wall anatomy of a primate differs from that of a human. The abdominal wall itself is much thinner, with thick skin and minimal-to-no subcutaneous fat layer, making secondary port site placement difficult, as the ports were never far from the underlying viscera. The anterior abdominal wall was inspected, and the inferior epigastric artery and vein were identified, with ports placed lateral to these vessels. The skin, muscular and fascial layers were incised with a scalpel, track open with an artery clip and 5mm ports then inserted to the left and right lower quadrants under direct vision to minimise uncontrolled trocar insertion and inadvertent visceral or vascular injury.
In the event of an intra-operative complication and conversion to an open procedure, if required, our plan was for a transverse suprapubic or Pfannenstiel laparotomy, aided by a small circumferential (Alexis O) retractor.
During the surgical planning process, multiple contraceptive methods were considered, including less invasive long-acting reversible contraception (LARC). The contraceptive implant (Jadelle: levonorgestrel-releasing implant 75mg) was previously used to provide contraceptive cover for Kera, but in the vet team’s experience, the effectiveness of implants in primate populations is unpredictable, often failing before the five years marked (Jadelle is available in New Zealand, effective for five years in humans <60kgs). The reason for this is not completely understood, but unfortunately it does necessitate removal and replacement under general anaesthetic every two years.
Intra-uterine contraceptive devices (IUCD) were also considered, but use is limited in primate populations. Again, this is secondary to primates with altered reproductive tract anatomy, making insertion of such devices very tricky.
After our team determined the use of LARCs would not meet Kera’s contraceptive needs, more permanent sterilisation options were considered, including hysterectomy, salingo-oophorectomy, salpingectomy and tubal ligation.
Hysterectomy presents issues, particularly in the absence of uterine manipulation and without expert knowledge of primate pelvic anatomy. Salingo-oophorectomy was also decided against, given the associated risk of ureteric injury at time of ligation of the infundibular pelvic ligament. Also, morbidity associated with menopause in a primate population is not so well understood (again only extrapolated from human studies).
Ultimately, salpingectomy was decided to be the superior sterilisation option, balancing risks against the benefits of lower rates of contraceptive failure and ectopic (interstitial) pregnancy.
Siamang gibbons are an endangered species and mating pairs are known to do so for life. The vet team, considering Kera’s best interest, understandably wanted to avoid any further pregnancy. But Intan may be required to breed in the future; therefore, vasectomy was not considered an option for this couple.
Summary
Despite a few speed bumps, our team successfully performed laparoscopic sterilisation for our newest friend Kera, and thoroughly enjoyed our day at the zoo.
References
- Deleuze S, Brotcorne F, Polet R, et al. Tubectomy of Pregnant and Non-pregnant Female Balinese Macaques (Macaca Fascicularis) With post-operative Monitoring. Journal of Frontiers in Veterinary Science. 2021(8);article 688656:1-10.
- Martelli P, Krishnasamy K, Kwan A, Wong A. Permanent contraception by laparoscopic tubectomy with ovarian conversation in Hong Kong macaques. Japanese Journal of Veterinary Research. 2020;68(4):209-215.
- Chai N. Endoscopy and Endosurgery in Nonhuman Primates. Veterinary Clinics: Exotic Animal Practice. 2015,15:1-15.
- Yu PH, Weng CC, Kuo HC, Chi CH. Evaluation of Endoscopic Salpingectomy for Sterilisation for Female Formosan Macaques (Macaca cyclopis). American Journal of Primatology. 2015:77:359-67.
- Kruse T, Bowman M, Ramer J, et al. Surgical Management of Uterine lesions in two captive Orangutans. Journal of Zoo and Wildlife Medicine. 2018;49(1):210-3.
- Newcomb L, Kruse M, Minter L, Sobolewski C. A Modern Approach to Minimally Invasive Surgery and Laparoscopic Sterilization in a Chimpanzee. Case Reports in Veterinary Medicine. 2019;1-5.





Leave a Reply