Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS) is a clinical and cystoscopic diagnosis, based on pain in the bladder and/or pelvis, associated with severe urinary frequency, urgency and nocturia, and following the exclusion of confusable disorders described below.1,2 Patients are often severely distressed, as GPs find that the urine culture is sterile, but often are unaware of the possible diagnosis of IC/BPS. Therefore, patients can see multiple gynaecologists or urologists prior to diagnosis, which is readily confirmed by urogynaecologists, as this condition is an important part of the urogynaecology trainee curriculum. Treatment is tailored to the severity of disease and patient response.
Diagnosis: history, bladder chart, examination and cystoscopy with refill examination
IC/BPS is defined by the European Society for the Study of Interstitial Cystitis (ESSIC) as chronic (>6 months) pelvic pain, pressure, or discomfort perceived to be related to the urinary bladder, accompanied by at least one other urinary symptom such as persistent urge to void or frequency/ nocturia. The pain is triggered by bladder filling (because patients have a small bladder capacity) and usually relieved by urination. Nocturia is virtually always present because the small bladder capacity and pain on filling wakens the patient to toilet.
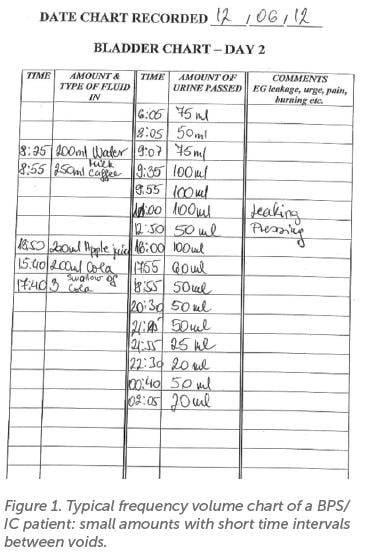
The bladder chart is an essential part of diagnosis, a typical example is shown in Figure 1, i.e. very small volumes, short voiding intervals (patient voided 11 times/day, 5 episodes of nocturia). Physical examination may reveal tenderness on palpation of the trigone (just above the cervix/vault) but should also be performed to exclude ‘confusable diseases’ such as pudendal neuralgia, endometriosis and vulval pain. Patients may also exhibit spasm of the levator muscles in the pelvic floor on palpation. The absence of urinary tract infection should be confirmed.
Cystoscopy must be performed under general anaesthesia by those experienced in diagnosis and bladder biopsy (because the maximum bladder capacity cannot be measured under local
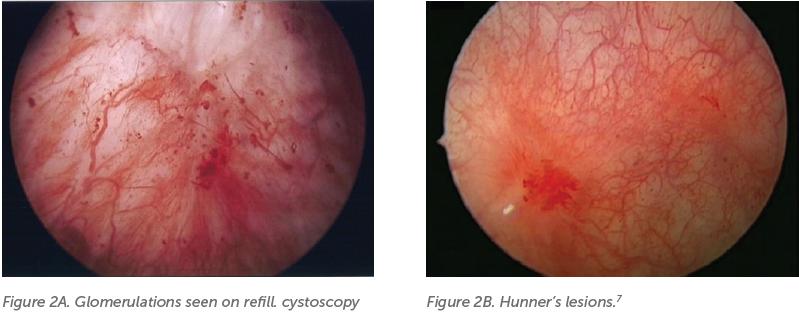
anaesthetic, patients will not tolerate the procedure). The technique has been standardised by ESSIC.2 It involves cystodistension (‘hydrodistension’) to assess for bladder capacity, followed by a refill examination to observe glomerulations, waterfall haemorrhages, and Hunner’s ulcers (now called Hunner’s lesions). Glomerulations can be found in patients without IC/ BPS and alone is not diagnostic.3 In 1915, Hunner described bladder ulcers (now referred to as lesions), appearing as a patch of red mucosa with small vessels radiating to a central pale scar.4 Bladder filling can also cause mucosal splitting in IC patients. Biopsy can assist in evaluating for inflammation, ulcer, fibrosis, and presence of mast cells – histological features associated with IC/BPS, which are more likely in the Hunner Lesion Disease (HLD) subtype.5,6 Although the name Interstitial Cystitis has widely been replaced by Bladder Pain Syndrome, these terms have been used interchangeably in medical literature. The 7th International Consultation on Incontinence recommends IC/BPS as the preferred terminology and that there should be no distinction, as has been previously suggested.1,8 There is recent emphasis on distinguishing HLD as a distinct phenotype, and that this should be determined for the purpose of clinical trials and to guide treatment.5,7,9 Cystoscopy is essential to delineate HLD vs non-HLD and exclude other disorders and thus we recommend routine cystoscopic evaluation, in contrast to the recent American Urological Association guideline.10
Due to variation in terminology and diagnostic criteria, there are discrepancies in the literature regarding the prevalence. Current estimates are that it occurs in 300 per 100,000 women, with a higher prevalence in women than men.11
Etiology
There are numerous theories as to the cause. There is evidence of an immune response, with activation of mast cells which secrete inflammatory mediators.12,13 Increased permeability of the urothelium due to damage to the GAG layer has also been demonstrated.14 This may cause pain due to reduced protection from the noxious contents of urine.15,16 Patients with IC/BPS have also been shown to have elevated anti-proliferative factor levels in urine, resulting in reduced cell production.17,18
Initial management if suspicion of disease
The role of the primary care physician is crucial. It is important to consider IC/BPS and refer patients when there is unexplained bladder pain. Patient symptoms should be believed, and a bladder chart requested when the urine culture is negative. Symptoms can cause sleep deprivation, reduce quality of life and a patient’s ability to function and work. This can have financial implications. There is an association with anxiety and depression. Dyspareunia or fear of intercourse is common, with resulting effects on relationships. Non-bladder syndromes and pain
outside the pelvis commonly co-exist. These include inflammatory bowel disease, allergies, irritable bowel syndrome, fibromyalgia, endometriosis, depression, and vulvodynia. The reason for this is unclear.19,20
Patient education is first line and involves explaining normal bladder function. Behavioural modification includes timed voiding, controlled fluid intake to avoid concentrated urine and dietary changes. An oxalate-free diet has shown some benefit. Acidic food and drink, coffee, spicy food, alcohol, and foods high in oxalates may aggravate symptoms, to varying degrees.21,22,23 It is recommended that each patient experiment in finding foods that aggravate symptoms and avoid these. See weblinks such as the IC Association at www.ichelp.org and National Institute of Diabetes and Digestive and Kidney Diseases at https://www.niddk.nih.gov/health-information/ urologic-diseases/interstitial-cystitis-painfulbladder- syndrome for patient information.
In patients who are found to have spasm or hypertonicity of the pelvic floor muscles on physical exam, pelvic floor therapy including myofascial trigger point release and Thiele massage can assist in managing pain.24 Stress and depression have been shown to occur in a higher proportion than in the general population. Treatment of this with mindfulness, counselling and medication is important in improving quality of life.
Amitriptyline is a tricyclic antidepressant which blocks H1-histaminergic receptors whilst stabilising mast cells. It may also have beta-adrenergic action, enhancing bladder storage. It is commenced at 25mg daily and titrated up to 100mg, though has sedative effects.25 Impramine 25–50mg can also be used. Studies have demonstrated small benefit from antihistamines such as hydroxyzine and cimetidine.26,27 Neuropathic analgesics such as gabapentin and pregabalin have been shown to reduce bladder hypersensitivity in animal models.28,29 Non-opioid analgesics should be used.
Urogynaecology management
Following diagnosis, treatment options include conservative therapies, oral medications, intravesical instillations and surgical management. We recommend that patients be referred to a urogynaecologist to ensure appropriate diagnosis and management.
Hydrodistension is always performed as part of the diagnostic cystoscopy, and can give short term improvement in a minority. Cystoscopic fulguration or diathermy of Hunner lesions has been clearly shown to result in symptomatic improvement.30 Injection of the corticosteroid triamcinolone to Hunner lesions has been shown to have comparable results to fulguration in small experimental studies.31,32
Dimethyl sulfoxide (DMSO) is the only intravesical agent approved for treatment of IC by the FDA. Side effects include a garlic-like odour for up to 24 hours and approximately 10% of patients report a flare which resolves, thought to be due to mast cell degranulation. 50% DMSO is instilled and retained for 20 minutes, sometimes along with a heparin, lidocaine, or steroid mix.34 This is repeated weekly for 6–8 weeks. Repeat courses can be undertaken for those who have a good response. Heparin can be instilled on its own and is thought to have similar properties to the GAG layer. Other instillations include hyaluronic acid, chondroitin sulfate, a combination (Ialuril) or chlorpactin.
Oral cyclosporine has been shown to be effective, particularly in those with HLD.33 Use needs to be closely monitored due to its adverse effects. There is no evidence to support efficacy from other types of immunosuppressant medications.
Sodium pentosan polysulfate (PPS/Elmiron) is an expensive (approximately $140/month) oral treatment, 100mg TDS, used for at least six months. It is a synthetic sulphated polysaccharide excreted into the urine, thought to replenish the GAG layer. It is the only oral drug currently approved by the FDA. It also has antihistaminic and possible anti-inflammatory roles. Recent reports have demonstrated a risk of pigmentary maculopathy from long-term exposure and regular ophthalmology review prior to and during treatment is recommended.35 There are conflicting findings from trials regarding its efficacy.36
There is some evidence of benefit from intravesical botulinum toxin; however, studies so far have included small numbers of participants.37 Sacral nerve stimulation is still considered an investigational procedure for IC/BPS, there may be benefit in select patients.38 It is recommended that long-term outcomes should be collected and reported. There is limited data to suggest efficacy of percutaneous or transcutaneous tibial nerve stimulation.39,40
Major reconstructive surgery should only be considered in cases where all other treatment options have failed. Bladder augmentation cystoplasty using bowel can improve storage and reduce pain. Risks include recurrent urinary tract infections, metabolic changes, and malignancy. Urinary diversion with or without cystectomy through creation of an ileal conduit or a continent diversion are options where cystoplasty is unsuccessful.41
Future research
Unfortunately, IC/BPS is a condition where much remains unknown. Further research is needed on its pathology, so that we can better understand why and how it occurs. Improved understanding of subtypes of the condition, as well as research into new treatment options, is greatly needed.
References
- Hanno P, et al. International Consultation on Incontinence, 7th Edition 2023. Chapter 18: Interstitial cystitis/bladder pain syndrome.
- van de Merwe JP, Nordling J, Bouchelouche P, et al. Diagnostic criteria, classification, and nomenclature for painful bladder syndrome/interstitial cystitis: An ESSIC proposal. Eur Urol. 2008;53(1):60-7. DOI: 10.1016/j.eururo.2007.09.019
- Wennevik GE, Meijlink JM, Hanno P, Nordling J. The role of glomerulations in bladder pain syndrome – a review. J Urol. 2016;195(1):19-25.
- Hunner GL. A rare type of bladder ulcer in women; report of cases. Boston Med Surg Journal. 1915;172:660-4.
- Fall M, Nordling J, Cervigni M, et al. Hunner lesion disease differs in diagnosis, treatment and outcome from bladder pain syndrome: An ESSIC working group report. Scand J Urol. 2020;28:1-8.
- Akiyama Y, Homma Y, Maeda D. Pathology and terminology of interstitial cystitis/bladder pain syndrome: A review. Histol Histopathol. 2019;34(1):25-32.
- Homma Y, Akiyama Y, Tomoe H, et al. Clinical guidelines for interstitial cystitis/bladder pain syndrome. Int J Urol. 2020;27(7):578-89.
- Abrams PH, Cardozo L, Fall M, et al. The standardisation of terminology of lower urinary tract function: Report from the standardisation sub-committee of the international continence society. Neurourol Urodyn. 2002;21:167-78.
- Hanno P, Fall M, Meijlink J, Nordling J. Towards a new paradigm in bladder pain syndrome and interstitial cystitis. BJU Int. 2020;126(5):549-50.
- Clemens JQ, Erickson DR, Varela NP, Lai HH. Diagnosis and Treatment of Interstitial Cystitis/Bladder Pain Syndrome. J Urol. 2022 Jul;208(1):34-42. doi: 10.1097/JU.0000000000002756. Epub 2022 May 10. PMID: 35536143.
- Leppilahti M, Sairanen J, Tammela TL, et al; Finnish Interstitial Cystitis-Pelvic Pain Syndrome Study Group. Prevalence of clinically confirmed interstitial cystitis in women: a population based study in Finland. J Urol. 2005;174(2):581-3. doi: 10.1097/01. ju.0000165452.39125.98
- Peeker R, Enerback L, Fall M, Aldenborg F. Recruitment, distribution and phenotypes of mast cells in interstitial cystitis. J Urol. 2000;163(3):1009-15.
- Hofmeister MA, He F, Ratliff TL, et al. Mast cells and nerve fibers in interstitial cystitis (IC): An algorithm for histologic diagnosis via quantitative image analysis and morphometry (QIAM). Urology. 1997;49(5A Suppl):41-7.
- Monastyrskaya K, Sánchez-Freire V, Hashemi Gheinani A, et al. MiR-199a-5p regulates urothelial permeability and may play a role in bladder pain syndrome. Am J Pathol. 2013;182(2):431-48.
- Hauser PJ, Dozmorov MG, Bane BL, et al. Abnormal expression of differentiation related proteins and proteoglycan core proteins in the urothelium of patients with interstitial cystitis. J Urol. 2008;179(2):764-9.
- Johansson SL, Fall M. Clinical features and spectrum of light microscopic changes in interstitial cystitis. J Urol. 1990;143(6):1118-24.
- Keay S, Seillier-Moiseiwitsch F, Zhang CO, et al. Changes in human bladder epithelial cell gene expression associated with interstitial cystitis or antiproliferative factor treatment. Physiol Genomics. 2003;14(2):107-15.
- Keay S, Kaczmarek P, Zhang CO, et al. Normalization of proliferation and tight junction formation in bladder epithelial cells from patients with interstitial cystitis/painful bladder syndrome by d-proline and d-pipecolic acid derivatives of antiproliferative factor. Chem Biol Drug Des. 2011;77(6):421-30.
- Alagiri M, Chottiner S, Ratner V, et al. Interstitial cystitis: Unexplained associations with other chronic disease and pain syndromes. Urology.1997;49(5A Suppl):52-7.
- Tirlapur SA, Kuhrt K, Chaliha C, et al. The ‘evil twin syndrome’ in chronic pelvic pain: A systematic review of prevalence studies of bladder pain syndrome and endometriosis. Int J Surg. 2013;11(3):233-7.
- Shorter B, Lesser M, Moldwin RM, Kushner L. Effect of comestibles on symptoms of interstitial cystitis. J Urol. 2007;178(1):145- 52.
- Li GZ, Zhang N, Du P, et al. Risk factors for interstitial cystitis/ painful bladder syndrome in patients with lower urinary tract symptoms: A chinese multi-center study. Chin Med J (Engl). 2010;123(20):2842-6.
- Friedlander JI, Shorter B, Moldwin RM. Diet and its role in interstitial cystitis/bladder pain syndrome (IC/BPS) and comorbid conditions. BJU Int. 2012;109(11):1584-91. doi: 10.1111/j.1464- 410X.2011.10860.x.
- FitzGerald MP, Payne CK, Lukacz ES, et al; Interstitial Cystitis Collaborative Research Network. Randomized multicenter clinical trial of myofascial physical therapy in women with interstitial cystitis/painful bladder syndrome and pelvic floor tenderness. J Urol. 2012;187(6):2113-8. doi: 10.1016/j.juro.2012.01.123.
- van Ophoven A, Hertle L. Long-term results of amitriptyline treatment for interstitial cystitis. J Urol. 2005;174(5):1837-40. doi: 10.1097/01.ju.0000176741.10094.e0
- Thilagarajah R, Witherow RO, Walker MM. Oral cimetidine gives effective symptom relief in painful bladder disease: A prospective, randomized, double-blind placebo-controlled trial. BJU Int. 2001;87:207.
- Theoharides TC. Hydroxyzine in the treatment of interstitial cystitis. Urol Clin North Am. 1994;21: 113.
- Yoshizumi M, Watanabe C, Mizoguchi H. Gabapentin reduces painful bladder hypersensitivity in rats with lipopolysaccharide- induced chronic cystitis. Pharmacol Res Perspect. 2021;9(1):e00697.
- Boudieu L, Mountadem S, Lashermes A, et al. Blocking α2δ-1 subunit reduces bladder hypersensitivity and inflammation in a cystitis mouse model by decreasing nf-kb pathway activation. Front Pharmacol. 2019;10:133.
- Ko KJ, Chung H, Suh YS, et al. Therapeutic effects of endoscopic ablation in patients with Hunner type interstitial cystitis. BJU Int. 2018 Apr;121(4):659-666. doi: 10.1111/bju.14097.
- Crescenze IM, Gupta P, Adams G, et al. Advanced management of patients with ulcerative interstitial cystitis/bladder pain syndrome. Urology. 2019;133:78-83.
- Jiang T, Zhou X, Chen Z, et al. Clinical efficacy of submucosal injection of triamcinolone acetonide in the treatment of type II/III interstitial cystitis/bladder pain syndrome. BMC Urol. 2020;20(1):36.
- Wang Z, Zhang L. Treatment effect of cyclosporine A in patients with painful bladder syndrome/interstitial cystitis: A systematic review. Exp Ther Med. 2016;12(1):445-450. doi: 10.3892/ etm.2016.3301.
- Lim YN, Dwyer P, Murray C, et al. Long-term outcomes of intravesical dimethyl sulfoxide/heparin/hydrocortisone therapy for interstitial cystitis/bladder pain syndrome. Int Urogynecol J. 2017;28(7):1085-1089. doi: 10.1007/s00192-016-3232-0.
- Pearce WA, Chen R, Jain N. Pigmentary Maculopathy Associated with Chronic Exposure to Pentosan Polysulfate Sodium. Ophthalmology. 2018;125(11):1793-1802. doi: 10.1016/j.ophtha. 2018.04.026.





Leave a Reply