The beating hearts of Australia
Rural, regional and remote Australia is a beautiful and vast area. For many First Nations Peoples it is their home, land and connection to culture, family and the past. It is also the backbone of the nation, with many of its residents working in major industries that drive the country’s economy.
At the heart of many of these towns is a local hospital, and in particular a birthing unit. When a town has a maternity service, it is a place where new families are literally started. This requires anaesthetics, general practitioners, paediatrics and theatre teams; and is integrated with other support services such as an emergency department, elective surgery, and allied health. Therefore, birthing units are the beating hearts of rural, regional and remote Australia.
The loss of a town’s maternity service can have a devastating effect. It can lead to reduced health services, young families leaving, and a lack of local services for First Nation Peoples on their own Country. Maintaining high quality and safe obstetric and gynaecological services is therefore essential for many towns’ survival. This however is not without significant challenges.
The Mapping Project
The Australian Government Department of Health and Aged Care funded Mapping Maternal Health and Gynaecological Services in Rural, Regional and Remote Australia: Uptake, Barriers and Recommendations – Research Project (mapping project) aimed to tackle these challenges through several means. The project brought together health service, workforce and population databases, and an ethics approved extensive survey of front-line maternity managers and leaders. This enabled the creation of a RANZCOG interactive online platform of existing maternity and gynaecological services, population demographics and workforce data that will support future service planning.
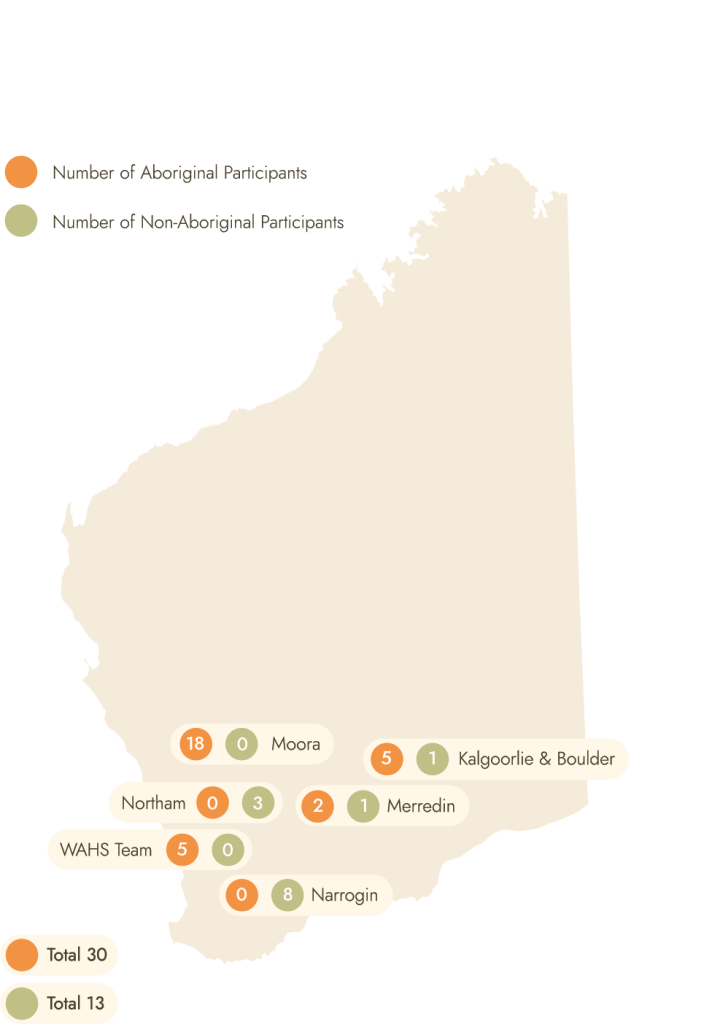
The project also engaged with rural and remote women to find out more about their experiences accessing obstetric and gynaecological services. This was achieved through the College’s collaboration with researchers from Flinders University and Murdoch University’s Ngangk Yira Institute of Change on yarning circles in South Australia (SA) and Western Australia (WA) with Aboriginal and non-Aboriginal women. This provided insightful information on what is needed to strengthen service delivery from a consumer perspective.
Learning from the yarning circles
Yarning circles are an established Indigenous method of research information gathering (Bessarab and N’aidu 2010) that aims to create a safe space for participants to tell their stories and offer opinions. Fifty-nine (59) Aboriginal women and twenty-eight (28) non-Aboriginal women took part in yarning circles across rural and remote SA and WA. The yarning circles helped determine the facilitators and barriers that affect service provision, and how services might be made more effective and consumer focused as outlined in the recommendations.

Recommendation 1: Appointment scheduling
Scheduling appointments for rural and remote patients requires consideration of the long distances women travel from, their expected travel time, the mode of transport the women use and the window of opportunity for appointment timings. In addition to this, consideration should be given to prioritising other appointments the women need when they have travelled to larger centres such as ultrasounds, education or visits to specialists.
Recommendation 2: Potentially mobile Women’s Health services
Women value privacy and some level of anonymity. There has to be a balance between known care providers who are not part of the local community but visit regularly to provide care. As a result, consistent timetabling of women’s health visiting services is required. This could potentially include a full range of services including cervical screening, mammograms, pregnancy checks and ultrasounds. As part of this recommendation, female providers were preferred if available. Where this need cannot be met, cultural training for all clinicians was highly recommended. In addition to this, Aboriginal women requested more stories of other Aboriginal women’s experiences. They also highlighted the need for more Aboriginal staff within the health system.
Recommendation 3: Health practitioner (and service) attributes
Women consistently identified the importance of knowing and being comfortable with health providers. It was noted that long term clinicians who women can develop a relationship with are highly valued. Trusted practitioners not only provide women with continuity of care but promote the opportunity for an equal partnership in health.
Recommendation 4: Support during Telehealth consultations
While Aboriginal women discussed a preference for face-toface appointments, they understood the value of telehealth over travelling long distances for appointments. Aboriginal women specifically highlighted the need to be supported in their room by an Aboriginal Health Worker or another health professional they are comfortable with.
Learning from the health service research
The ethics approved research was led by RANZCOG with the data analysis undertaken by the University of Notre Dame’s Institute of Health Research. The research involved voluntary participation from rural, regional and remote health services that provide services. Participants completed an online survey that covered the following themes: available services, proximity to supporting services, models of care, and workforce data.
The research commenced in May 2022, and as research governance approval was also required from each state and territory by January 2023, the timely approval from each jurisdiction was a key requirement for health services taking part in the research. 204 health services confirmed their eligibility to take part in the research. Of the 204 health services, 144 were granted research governance approval by January 2023. 80 (55.6%) of those health services took part in the research. This percentage was lower than anticipated, even with support provided to sites to assist with the survey. Many sites however quoted being too busy to be involved in the research, or a lack of permanent staff that would be able to provide the required information. This alone highlighted the severe staff shortages and heavy reliance on locums in many rural areas.
The findings outlined below were deemed to be statistically significant from the research data;
Maternal health services offered by health services
- As expected, the availability of maternal health service options for women decreased the higher the remoteness category.
- Contrary to this pattern, several Monash Modified Model (MM) 6 and MM 7 located health services managed to provide higher risk or more advanced obstetric services such as Vaginal Birth after Caesarean (VBAC). This finding has provided the Department with an opportunity to review such outcomes in remote sites and consider if these processes and services can be safely replicated across other remote areas.
Gynaecological services offered by health services
- Responding health services offered fewer gynaecological services than they offer maternity services.
- Surgical abortions later than 12 weeks require women to travel longer distances than for other gynaecological services.
- Medical abortion access was limited in the lower half of WA compared to other rural and remote areas.
Factors associated with increased demand of services
- There appeared to be some univariable association of increased demand for gynaecological services with the model of maternity care currently available at responding health services. Health services that identified as having a shared care model of care (OR 3.2 95%CI 1.2-8.7 p=0.023) or a public hospital maternity care model of care (A) (OR 3.4 95%CI 1.3-9.0 p=0.016.) were both around three times more likely to report increased demand for gynaecological services compared to other models of care.
- Health services that use more fly-in fly-out Consultants were more likely to report increased demand for gynaecological services. For every 10% increase in the percentage of fly-in fly-out consultants in the last month, the odds of reporting increased demand for gynaecological services increased by 15% (95%CI 1-30%, p=0.042).
- Health services that offered hysterectomies were 4.0 (95%CI 1.5-11.0) times more likely to report increased demand for gynaecological services.
- Health services that offered colposcopy (OR 5.5 95%CI 1.9-16.2) or cystoscopy (OR 4.0 95%CI 1.5-10.8) were also more likely to report increased demand for gynaecological services.
Reasons for obstetric transfers
- Staffing issues as a reason for obstetric transfer started at MM3 and in general increased with remoteness level.
- Medical staffing issues were reported less often as a reason for obstetric transfer than midwifery staffing issues.
Support services currently available
- Most Consultant funded positions were in MM3 based health services, and around half were 50% or less filled by permanent staff.
- It appeared that health services in remote and very remote communities have less funded positions filled with permanent GP Obstetricians than medium and small towns.
- Only a relatively smaller number of health services reported all funded midwife positions were filled by permanent staff and these health services tended towards the lower MM.
- The more remote MM areas had quite low numbers of funded midwife positions filled by permanent staff.
Fly-in Fly-out (FIFO) and Locum workers
- The degree to which a health service relied on FIFO and/ or locum workers within the last month varied from 10% to 100% of total FTE.
- The proportion of staff employed as FIFO or locum increased with increasing MM category.
The O&G Map
As part of the mapping project, RANZCOG has designed and developed an interactive web map accessible via the RANZCOG website. The interactive map (referred to as the O&G map) will be publicly available and provide access to the location of publicly funded obstetric and gynaecological specific health services, key population data and O&G workforce data. The launch of the O&G map on the College website is currently underway.
A heartfelt thank you
The College would like to thank the many frontline staff and consumers who took part in the mapping project. The College hopes that this work will be the start of a ‘living project’ to help guide the future planning of rural, regional and remote obstetric and gynaecological services – the ‘Beating Hearts of Australia.’
To find out more about the Mapping Project please email [email protected]






Leave a Reply