Since the introduction of surgical robots to Australian operating theatres in the early 2000s, the popularity of robotic surgery has well and truly skyrocketed. Amongst almost all surgical specialties, robotic surgical systems have been used to replicate traditionally open or laparoscopic procedures with precision, dexterity and minimal invasiveness, whilst also offering potential protection against work-related musculoskeletal injuries1.
While the question of cost-benefit remains under scrutiny2, the unique technical advantages of robotic surgery have resulted in early scepticisms fading and the demand for robot-assisted procedures surging. Studies have demonstrated comparable safety and clinical outcomes for a wide range of gynaecological procedures including hysterectomy, myomectomy, sacrocolpopexy, excision of severe endometriosis and isthmocoele repair3. There is no doubt that robotic surgery has cemented itself in the world of operative gynaecology.
The surgical robots in use reflect years of careful engineering with well-designed user interface and intuitive controls. Even the novice operator trying their hand at a display robot will find that they are capable of stacking a few blocks in no time at all. Although the first hands-on experience with a surgical robot may feel as exciting as getting your hands on the latest iPhone, one must remain mindful that surgical robots are no toy. As with all new techniques and technology, there is a learning curve to mastering their control and optimising their functionality in real-life surgery.
According to data supplied by Device Technologies for this article, as of April 2023 Australia is home to 88 Da Vinci Xi surgical systems, of which 14 reside in public hospital operating theatres. With the mounting realisation among gynaecological consultants and trainees of their utility, there is growing demand for more equitable access to surgical robot systems in the public sector for surgical training on these platforms4.
With a relatively small proportion of surgical robots in Australia residing in public hospital settings, most gynaecology trainees may find that they have limited or no exposure to robotic surgery during their training years. Even experienced surgeons may find limited opportunity to learn robotic skills through observation before taking a seat in the console. With benefits such as 3D vision, instruments with seven degrees of motion, enhanced ergonomics particularly when navigating high patient BMI, and facilitation of multidisciplinary collaboration in increasingly complex surgeries, the need for orientation to robotic training under simulation and avenues for formal credentialing is emerging rapidly. In this article, we assess the simulation platforms currently available for training in robotic surgery and discuss the potential impacts and implications of simulation-based platforms on training, certification and credentialing in gynaecological surgery
Simulation training specific to robotic surgery is available in a number of different formats, and takes inspiration from those options available to the trainee laparoscopist. In dry-lab simulation, surgeons practice their robotic skills using the console to control instruments docked inside a so-called ‘box trainer’ or synthetic body cavity model. Surgeons can begin to learn basic skills such as camera control, dual and third-arm coordination, cutting, dissection, suturing and knot-tying using real instruments on a plastic or siliconebased model. Dry-lab simulation does offer a good basis for gaining familiarity with robot functionality and control5.
The main limitation of dry-lab simulation is that such practice does not give the operator the experience of working with real-life tissue. With the lack of haptic feedback offered by robotic arms, navigating tissue tension is an added complexity that must be conquered by the robotic surgeon.
Wet-lab simulation provides a logical solution to this problem. This platform replaces box-trainers with animal or cadaveric models. Practicing with real tissues allows the novice robotic surgeon to gain an appreciation for tissue responsiveness to robotic instruments and to master safe and gentle tissue handling, overcoming the absence of haptics. As is the case with any wet-laboratory arrangement, access is impeded by significant costs, scarce supply and rigorous ethical approval pathways which can be prohibitive5.
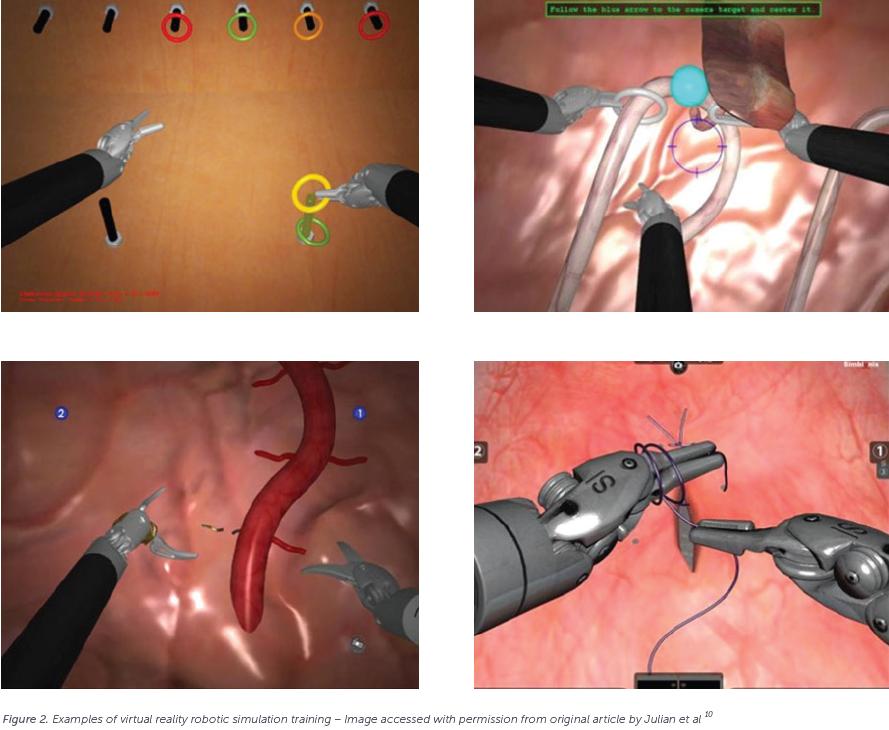
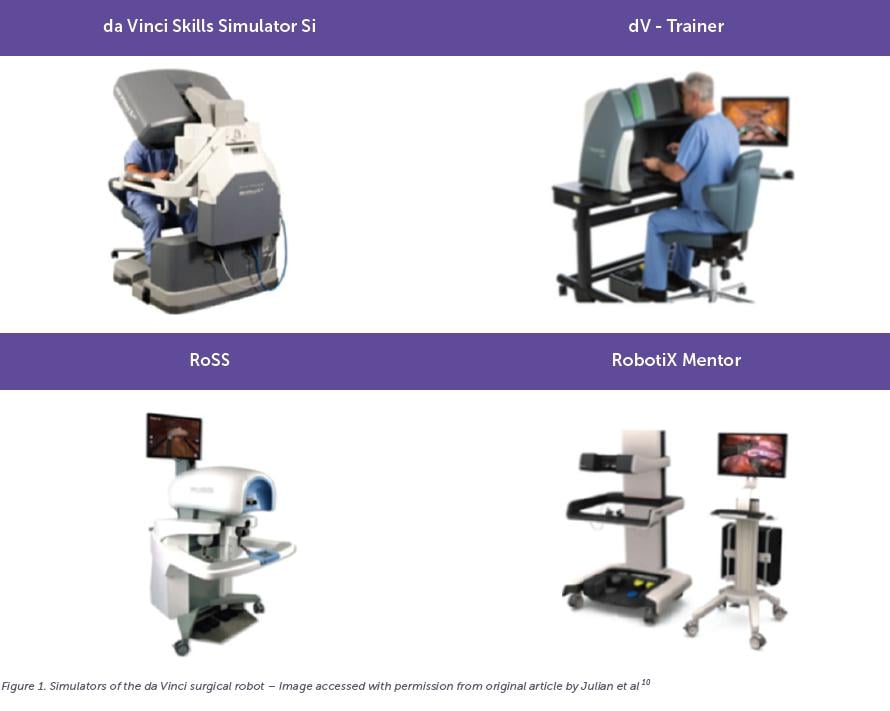
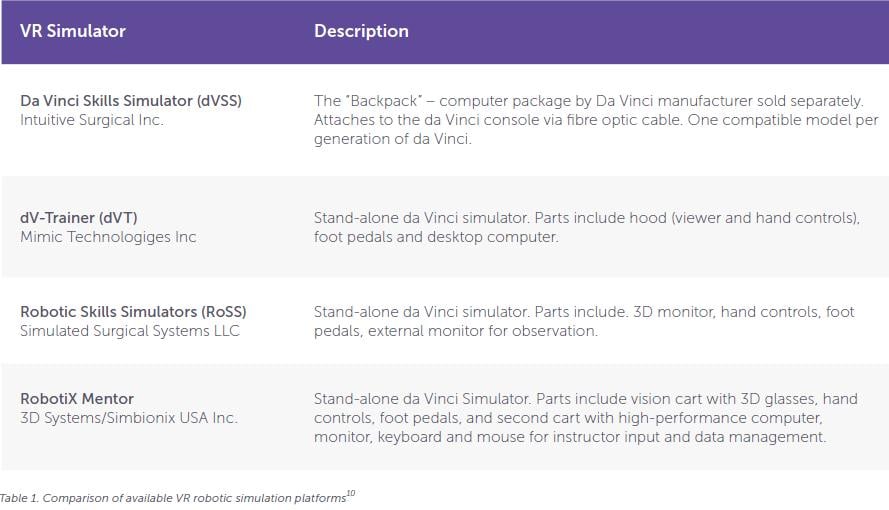
Virtual reality (VR) robotic simulation can forgo the need for access to a surgical robot in order to enter the robot training domain. Use of stand-alone vision carts, 3D monitors, handpieces and foot pedals reproduce the command of robotic controls. Computer packages that attach to the actual surgical console also exist, which do require robot availability but mimic the surgical experience with a high degree of realism. With capacity to design infinite training scenarios, VR allows the user to enter robotic training at any level of experience and practice simple to complex surgical skills. Simulated tasks range from sorting rings onto pegs to performing start-to-end surgical procedures. Inbuilt feedback mechanisms allow for real-time user assessment and measurement of progress5,6.
Both wet and dry-lab simulators require the availability of a not-in-use robot system and training media. Dry-lab simulation therefore has the advantage of being the more cost-effective and accessible option. High capital costs for VR simulators may somewhat restrict their widespread adoption. However, where access to surgical robots is limited, standalone VR simulators remain an attractive and upcoming alternative7.
Since the first surgical robot was approved for use in humans by the United States FDA in 2000, numerous studies comparing robotic simulators and their utility for building surgical proficiency have been published. Through extensive validation, surgical skills development through simulation training in robotic surgery has been demonstrated5.
Validation studies comparing simulation models should examine the face, content and construct validity of the various platforms. Face validity refers to the degree to which the simulation resembles the real task (i.e. how well does the task recreate the experience of suturing, dissection or handling of tissues?). Content validity assesses the value a simulated task in building relevant skills (i.e. does this task train skills that a surgeon actually needs?). Construct validity measures the ability of the simulation to differentiate between users of different skill levels (i.e. can the difference in performance of a resident versus a fellow be accurately detected?)5.
Other types of study may examine predictive validity which measures the degree of correlation between simulation performance and real-life surgical performance, and concurrent validity which examines how performance of a new simulator compares to performance of an existing validated simulator5.
A 2013 study by Ramos et al aimed to compare dry-lab versus VR exercises in terms of their face, content, construct and concurrent validities8. Participants were grouped by experience level (novice or expert) and asked to complete three VR exercises using the da Vinci Skills Simulator (Intuitive Surgical) and corresponding dry-lab versions of the same task on the da Vinci Surgical System. Post-study questionnaires evaluated the surgeons’ experiences. Expert surgeons found the exercises on each platform both useful (content validity) and realistic (face validity), and reliably outperformed the novice surgeons at all tasks (construct validity). There was a moderate correlation between performance on the dry-lab simulator compared to the VR simulator (concurrent validity).
Further examining the utility of VR simulation to the dry-lab experience, a 2020 comparative study by Raison et al examined the performance of 43 novice operators (predominantly medical students) following allocation to dry-lab or VR-based simulation training at two centres in the UK and Italy6. Participants were asked to complete equivalent training exercises during a 3-hour course with expert mentoring. Upon completion of the training they were assessed by two trained raters using the validated Global Evaluative Assessment of Robotic Skills (GEARS) scoring tool. GEARS scores increased significantly in both groups over the course, with higher technical skills observed in the VR group earlier in the course, but a statistically significant difference between the groups in favour of dry-lab training at course completion.
A growing number of VR platforms currently exist on the market. A study by Hertz et al in 2018 compared the face and content validity of all dedicated da Vinci robot simulators – which includes the da Vinci Skills Simulator (dVSS), dVTrainer (dVT), Robotic Skills Simulators (RoSS) and RobotiX Mentor9. Participants were surgical residents with limited robotic exposure. Each was asked to complete tasks on three simulators then complete a feedback questionnaire. The authors concluded that all simulators offered face and content validity, with statistically significant results.
In summary, robotic simulation offers an exciting alternative platform for surgical training and accreditation in gynaecology which allows surgeons to build confidence and competence prior to operating robotically on real patients. The validation of simulation training models as useful for the trainee robotic surgeon is especially important in view of limited surgical exposure to major gynaecological procedures in O&G training11. It offers surgical colleges, including ours, the opportunity to consider the potential applications of simulation platforms in assisting formal surgical training. Minimum standards for simulation-based exposure and performance may substitute some of the training requirements needed prior to obtaining accreditation via mentoring and proctoring. It is also conceivable that, with increasing validation of virtual reality robotic simulation training, these platforms may enhance the rigour of formal accreditation and re-certification pathways for surgeons and trainees. Importantly, this may also offer the potential to improve patient safety.






Leave a Reply