Discovering how to safely reduce the rate of preterm and early term birth should be one of the highest priorities in contemporary healthcare. Being born too early can lead to serious consequences, including death and lifelong disability, for the child.
Preterm birth is defined as birth before 37 completed weeks of gestation. This definition was never based on any measure of fetal maturation, but rather was chosen as the age at which the newborn is likely to weigh more than 2500 g. Birthweight had traditionally been the measure of interest before the introduction of ultrasound imaging enabled accurate estimation of gestational age.
We now know the fetus is not fully mature until 39 weeks gestation. The 14-day period between 37 weeks and 38 weeks and 6 days is known as ‘early term’. The rate of birth in the early term period has risen dramatically in recent years with one in every three Australian children now born in this 14-day window. Early term birth substantially increases the risk of behavioural and learning problems at school age. It is likely the increase in early term births in our maternity services is one of the causes contributing to difficulties being experienced by Australian children in our education system.
In 2014, a statewide program was introduced to safely lower the rate of preterm birth across the whole population in Western Australia (WA). In the first full calendar year, the rate of preterm birth across the state fell by 7.6% and the reductions extended to the earlier gestational ages. With funding provided by a NHMRC Partnership grant, the program was then rolled-out nationally in June 2018 through the establishment of the Australian Preterm Birth Prevention Alliance (the Alliance). The Alliance and its activities are the world’s first national preterm birth prevention program.
The seven strategies included in the program were chosen for the high evidential basis of their effectiveness and suitability for the Australian healthcare environment. In summary, they include: avoidance of birth before 39 weeks completed weeks of gestation unless there is medical or obstetric justification; measurement of the length of the cervix at all mid-pregnancy morphology ultrasound scans; prescription of vaginal progesterone pessaries for any case of shortened cervix or for past history of spontaneous preterm birth; ongoing monitoring of the length of the cervix if shown to be shortened; smoking cessation programs; and promotion of continuity of care by a known healthcare provider (Figure 1).
The success seen in WA was soon replicated in the ACT and Tasmania, but not in the larger population states of NSW, Victoria and Queensland.
It was clear the strategies together can be successful, but a more effective method of implementation was required to achieve and sustain reductions in preterm birth. The method chosen was the Institute for Healthcare Improvement (IHI) Breakthrough Series Collaborative model. Appropriate financial support was provided by the Commonwealth Government in the May 2021 Budget.
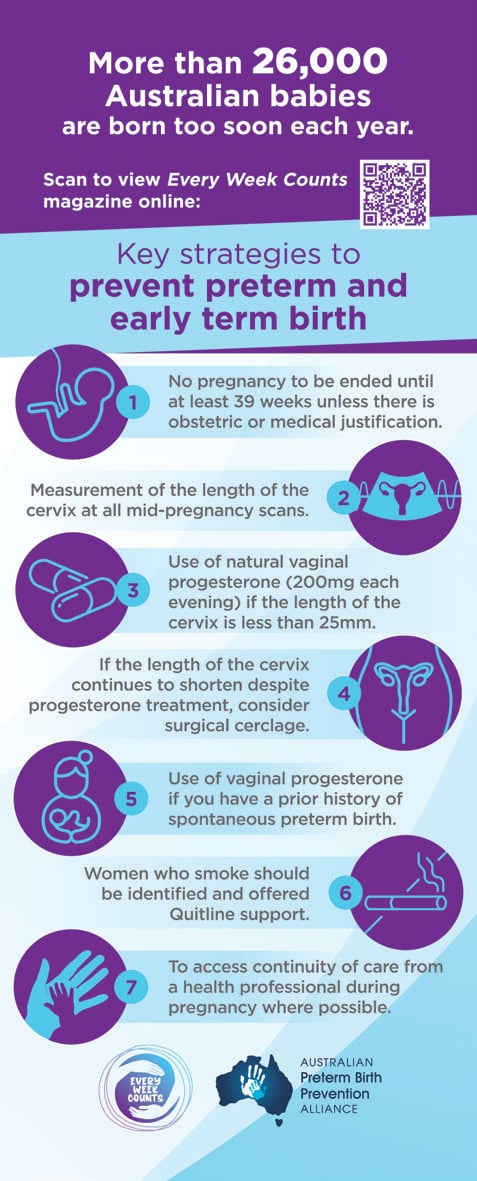
Figure 1. The seven clinical strategies included in the Every Week Counts National Collaborative.
The IHI Breakthrough Series Collaborative model was originally developed in Boston, USA, and aims to produce rapid and enduring improvements in clinical practice across healthcare facilities. In essence, there is a structured program in which the overall aim is defined and the package of evidence-based strategies is provided to each participating maternity service. Each team utilises improvement science to test and implement these strategies to maximise the chance of achieving impactful results in their own environment. Consumer representatives are embedded in the design, delivery and decision-making processes across all stages of the Collaborative.
Sixty-three hospitals from 49 health care services are included in the Collaborative (Figure 2). These sites were chosen with a view to providing diversity in geographical location and level of service. The invitation to participate was issued in consultation with the eight jurisdictional health departments and was based on the principle of ‘going with the willing’.
The Collaborative commenced in October 2021 and is known as the Every Week Counts National Preterm Birth Prevention Collaborative. Our aim is to safely lower the rate of preterm and early term birth across the 63 participating maternity services by 20% by March 2024.
Teams in each hospital undertake local tests of their implementation ideas for each of the seven strategies.
The process of iteratively conducting these tests, known as Plan-Do-Study-Act (PDSA) cycles, allow teams to rapidly learn how to reliably implement strategies and achieve improvements in their local context. The learning and data from each PDSA cycle are shared on a software platform called LifeQI, together with outcome data from their own hospital, the other 62 hospitals and the aggregate data from all 63 hospitals. At the time of publication, there have been more than 680 PDSA cycles registered in LifeQI across the 63 sites participating in the National Collaborative.
Each of the participating hospitals also receive ongoing support provided by professional Improvement Advisors in regular virtual coaching calls. Clinical teams and their Executive Leaders also attend three face-to-face Learning Sessions across 18 months at which the learnings from all participating hospital teams are shared.
The Collaborative model is proving to be highly effective. At its heart is the principle of empowerment of healthcare workers to make improvements in their own hospital environment. Every member of the working team becomes vitally important to the overall task – including not only executive leaders, obstetricians, and midwives, but also delivery ward and operating theatre booking clerks, pharmacists, sonographers and any other person involved in the provision of such care.
To enable this large national project, the Alliance partnered with Women’s Healthcare Australasia (WHA). WHA is a not-for-profit organisation based in Canberra that includes 160 maternity services from across Australia. Each service provides clinical data that are then returned to the participating centres in a format that allows teams to see the effect of their improvement efforts over time on outcomes for women and their babies, as well as benchmarking of their service when compared with others. The availability of such effective and timely data systems made WHA the perfect partner, providing a rich source of information to monitor the program and continuously feed each hospital with their own outcomes along with those of their peers.
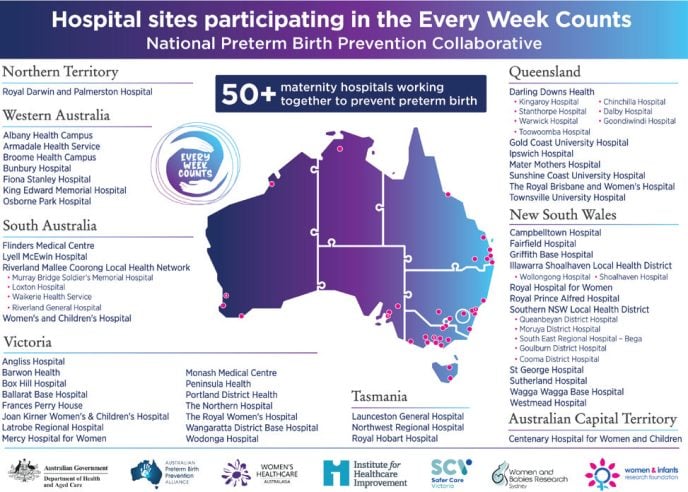
Figure 2. The names and locations of the 63 maternity hospitals participating in the Every Week Counts National Collaborative.
Together, the Alliance, WHA and IHI have partnered with each of the nation’s eight jurisdictional Health Departments, many of which have provided additional resources enabling the number of participating hospitals to be increased to 63. Important partners also include Safer Care Victoria and the Stillbirth CRE for shared policies and educational materials, and consumer and First Nations groups. The Women and Infants Research Foundation in WA is the Administering Institution.
The Collaborative is scheduled to conclude in March 2024. However, this program is expected to be ongoing and aims to provide appropriate support to as many of our nation’s maternity services as is possible.
This national story is one of Australian research being shown to be effective when applied to one state and then rolled out with support from the Commonwealth to include all of our six states and two territories. The early signs of success are very reassuring and give hope that Australia is on track to become the world’s first country to strategically and safely lower its rate of untimely early birth.









Leave a Reply