I was a pre-clinical medical student in 1978 when Louise Brown’s birth after IVF hit the headlines. The early days of IVF were highly newsworthy and every week had a story either over-dramatising the latest great breakthrough or threatening the end of civilisation as we know it, owing to the nefarious activities of these dangerous doctors. Maybe this was why I became interested in this area of obstetrics and gynaecology, although it was only much later, in Edinburgh in 1987, that I committed to subspecialisation in the new field of ‘reproductive medicine’. My clinical training in management of infertility and the plethora of other endocrine and anatomic disorders that affect the human reproductive system could not have been at a more exciting time as IVF came of age and the opportunities that access to human embryonic tissue could offer became obvious.
I moved to take the Chair in Obstetrics and Gynaecology in Sheffield in 1999. I continued to have an active interest in obstetrics and was regularly ‘on call’ for the labour ward at the Jessop Hospital, but was mainly occupied in managing the move to the academic department that was part of the new ‘Jessop Wing’ that opened in 2001 (a note to developers of new hospitals: it’s not wise to use the same, or a similar, name as the old building – people show up in the wrong place even years later).
A small group of us were asked to consider setting up an National Health Service (NHS)-based fertility/IVF centre within the new building. At this time many IVF units were entirely private, limiting access to the less well off, and NHS funding was extremely patchy. We felt strongly that Sheffield needed an NHS centre and were fortunate to have access to space and funding to set this up. From the outset we had a strong academic presence within the clinical unit, with a senior lecturer, clinical lecturer and non-clinical senior lecturer (now professor) and myself working in the Assisted Conception Unit (ACU). We were approached at an early stage by Profs Harry Moore and Peter Andrews, both University of Sheffield biomedical researchers, who were keen to develop studies using human embryonic stem cells (hESC). This was timely as Tony Blair was piloting the necessary legislation through the UK Parliament to legalise hESC research and possible clinical use. Our new unit gave us the opportunity to develop ‘near GMP’ IVF. This meant that hESC products could potentially be used in clinical trials and therapeutics later.
Good manufacturing practice (GMP) is used in the pharmaceutical industry for drug development and clinical trial development. It requires clean room technology with intensive monitoring of air quality, bacteriological contamination and facility monitoring, for example of incubator temperature, humidity, O2 and CO2 tension and so forth. We were able to build these features into the IVF unit with a grant from the Medical Research Council. This also allowed us to meet the requirements of the European Union Cells and Tissues Directive, which was being applied to UK IVF at that time. We were one of the first centres to meet these criteria.
We had to call this ‘near GMP’ because it is impossible to carry out some of the IVF procedures to a GMP standard. The mechanics of sperm sample production were particularly difficult to organise in a completely sterile controlled environment as it put many of the men off their stroke. However, there was optimism that we could derive stem cell lines in the new ACU that could be used later in clinical trials.
Once the House of Lords approved the Act of Parliament we were able to apply for ethics committee permission to try to derive hESC. We were always careful to make sure that every step of the process was fully approved and were transparent in our plans in setting up the stem cell lab within the IVF lab. Harry and Peter were able to collaborate with the clinical team and derived stable stem cell lines that were later donated to the national Stem Cell Bank run by National Institute for Biological Standards and Control (NIBSC) in North London, which opened in 2004. This allowed any legitimate researchers to have access to the cell lines. At that time, Prof Colin Blakemore, chief executive of the MRC, said: ‘Stem cell research offers real promise for the treatment of currently incurable diseases. The bank will ensure that researchers can explore the enormous potential of this exciting science for the future benefit of patients.’ This describes the feeling that many of us had about the potential benefits that could derive from hESC research.
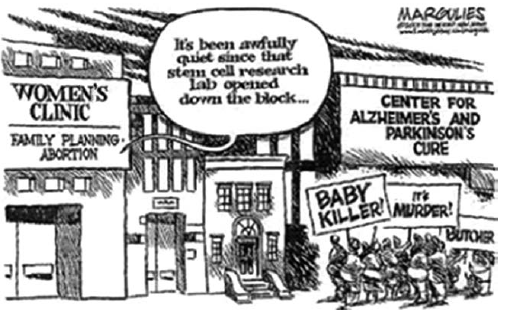
Newspaper cartoonists in the USA found much to inspire them in the stem cell debate. © Jimmy Margulies. First appeared in The Record, Hackensack, New Jersey. Used with permission of the artist.
There were many early achievements and discoveries. I remember the excitement when the lab identified a stem cell derivative that secreted insulin and modified its level of secretion in response to changing glucose concentration in the culture medium. There was a finding that some lines de-differentiated even after many passages, becoming teratomas, with obvious implications for human therapeutic use, and the persistent problem that the cell lines expressed HLA and hence could not be used for transplantation to other individuals. There was also constant engagement with the HFEA as regulator of this research, with MRC and NIBSC and with the public concerning the ethics and governance of hESC research. I think we expected more criticism and debate than actually happened, and we were never picketed or heckled. Of course, this was before the days of social media, so those who wished to complain and criticise were identifiable and could not anonymously troll.

Meanwhile, in Australia and the UK, the possibilities of this scientific breakthrough were the focus of positive news reports
Stem cell research and therapeutics has come a long way in the last decade. Many of us have moved on to other areas of work and maybe the promise of the early days has yet to be realised. However, there are already tangible clinical benefits from this research and it has begun to translate into clinical practice. We have also learned a great deal about cell biology, regulation of cell division and differentiation and about early embryology. The ACU in Sheffield has become highly successful and continues to be active in research. The world of IVF also continues to innovate and adopt new ideas at a rapid rate. The use of IVF to access the embryonic genome will be a key tool in the science of individualised medicine in the coming decades. There are many more discoveries to make!
Further reading
UK Code of Practice for the Use of Human Stem Cell Lines 2010. Available from: www.mrc.ac.uk/documents/pdf/code-of-practice-for-the-use-of-human-stem-cell-lines/ .
Steering Committee for the UK Stem Cell Bank and for the use of Stem Cell Lines. See: www.mrc.ac.uk/research/research-policy-ethics/uk-stem-cell-bank-steering-committee/ .
UK Stem Cell Bank. See: www.nibsc.org/science_and_research/advanced_therapies/uk_stem_cell_bank.aspx
Regulation of stem cell research in Europe. See: www.eurostemcell.org/stem-cell-regulations .
Human Fertilisation and Embryology Act (1990). Available at: www.legislation.gov.uk/ukpga/1990/37/contents
Human Fertilisation and Embryology (Research Purposes) Regulations 2001. Available at: www.legislation.gov.uk/uksi/2001/188/contents/made .





Leave a Reply