Timor-Leste, as a nation, was born out of desire for independence – the independence vote in 1999 was unanimous, but the carnage that followed was overwhelming – infrastructure was destroyed and the health system fared no better. Many doctors left the country and the infrastructure, particularly in the regional areas, was close to non-existent. In the 16 years since, external aid, a concerted government investment in healthcare and a characteristic Timorese courage have helped to re-energise the health sector. Today, the beautifully designed Hospital Nacional Guido Valadares (HNGV), funded by international aid donations, is the largest medical facility in the country and treats thousands of patients each year.
The maternity unit at HNGV delivers approximately 4500 babies a year. The hospital also has a busy outpatient department (OPD) and gynaecological unit. The daily work is divided between the OPD – with referrals from clinical health centres (CHCs) – and operating theatres, on-call labour ward cover and daily rounds of O&G inpatients. There are six maternity cubicles, each with two beds, and an acute gynaecology room for presentations – typically ruptured ectopic pregnancies, heavy menstrual bleeding, miscarriage and acute pelvic inflammatory disease (PID). There are a large number of spontaneous vaginal deliveries, as it is the main maternity unit in a country of 1.2 million people. The caesarean section rate at HNGV in 2015 was 21.3 per cent, which reflects the complicated referred cases as well as the differing indications and thresholds for a caesarean section, depending on the background of the consultants in the unit. Instrumental delivery rates were 6.8 per cent in 2015, while there are large numbers of both breech vaginal and twin deliveries.
The O&G unit is staffed by six consultants, eight junior doctors (resident equivalent), five family medicine program (FMP) trainees (intern equivalent) and approximately 20 midwives and nurses. In addition, there is a consultant midwife from St John of God Hospital, Perth, who has become an invaluable member of the maternity unit. A problem faced in Timor-Leste is the number of languages used: there are specialist doctors from the Cuban brigade, the Chinese brigade, a United Nations Population Fund (UNFPA) employee who is Nepalese, two local Timorese consultants (trained in Indonesia) and me (trained in Australia). Spanish, Portuguese (a colonial remnant), Indonesian, Tetun and English are used in conversation daily as well as in the clinical notes, making understanding and conversing between health personnel and patients challenging, to say the least.

On the labour ward at HNGV.
The Royal Australasian College of Surgeons (RACS) has had a presence in Timor-Leste since 2002. The project has been conducted under the Australia Timor-Leste Program of Assistance for Secondary Services (ATLASS), funded by the Australian Government and managed by RACS, in collaboration with the Timor Leste Ministry of Health. The project has made a significant contribution to the provision of clinical services and training of doctors in the hospital. Currently, the project involves the provision of five specialists – in the areas of surgery, paediatrics, emergency medicine, anaesthesia and O&G – to help with the training of the next generation of Timorese doctors, with a particular focus on postgraduate training. As there is currently no postgraduate training available in Timor-Leste for O&G, this has become one of the main aims of the RACS initiative here.
The current role of the O&G specialist is to train the FMP doctors, who spend eight to ten weeks rotating around the various specialities. This short but intensive period with the specialist within the O&G department aims to place them in good stead to manage and refer cases once they are sent to the CHCs, many of which are in isolated areas. The teaching is a combination of didactic lectures along with on-the-job training on the wards, OPD and in theatre.
Teaching is not restricted to the FMP doctors. Both formally and informally, teaching is undertaken daily with the current junior medical officers and midwives on a range of topics, including interpretation of cardiotocography, instrumental deliveries, common obstetric emergencies and postoperative care. Daily teaching on ward rounds is also undertaken, according to the caseload available. This teaching is often juxtaposed with more formal multidisciplinary teaching sessions (involving midwives and doctors) on common procedural skills, such as breech extraction, shoulder dystocia management and performance of instrumental deliveries.

Teaching caesarean section to junior medical officers.
Besides the busy labour ward, most of the clinical time is spent in the OPD and operating theatres. The OPD clinic is made up of antenatal referrals and gynaecological presentations. Standard antenatal care is undertaken in the community; however, women with risk factors – large or small for gestational age, pre-eclampsia, twins, unsure dates – are sent to the OPD for a second opinion. Additionally, there is a large gynaecological component in the clinics, with referrals spanning from utero-vaginal prolapse, chronic pelvic pain from PID and endometriosis to heavy and irregular menstrual bleeding.
Ultrasound encompasses a significant amount of the work, as it provides not only the ability to date pregnancies to a reasonable degree, but also diagnose malformations and assess the status of the fetus in utero. Diagnosis of gynaecological conditions, such as large ovarian cysts and uterine myomas, by ultrasound also makes diagnosis and pre-operative planning easier. Discussion and advice on difficult ultrasound interpretation as well as management of specific maternal-fetal medicine cases is often undertaken with colleagues from Australia.

Teaching caesarean section to junior medical officers.

Members of the obstetrics and gynaecology unit at HNGV.
There are three theatres and the O&G unit has three half-day elective lists per week. After-hours access to theatre is good; as theatre staff are present 24 hours a day and anaesthetists are available within 30 minutes. The range of pathology presenting to the OPD allows a relatively large number of vaginal and abdominal operations to be undertaken on the elective lists. As histopathology services are not available in Timor-Leste (and are very expensive for patients to send to Indonesia), anticipatory surgery is often undertaken based on a suspected pre-operative diagnosis.

An 18.5kg right ovarian tumour removed at laparotomy in a 45-year-old; proceeded to total abdominal hysterectomy, left salpingo-oophorectomy and infracolic omentectomy.
Though the main aim of the employment by RACS of an O&G specialist was to assist in postgraduate teaching, there is a large service component to the role of consultant, along with providing improvements in the systems within the maternity unit. In seven months, 264 procedures were performed by me, with the major procedures listed in Table 1. The rest of the procedures consisted of vaginal breech and twin deliveries, manual vacuum aspiration/dilatation and curettage, minor vaginal surgery and tubal ligations. This does not include the supervision or assistance of midwives or doctors undertaking complex deliveries or the more than 400 ultrasounds undertaken to date.
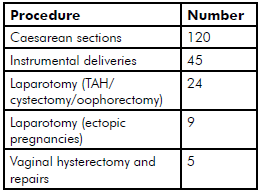
Table 1. A summary of major procedures
undertaken over a seven-month period at HNGV.
There are a number of limited investigations available. Access to x-ray is relatively easy, but attaining computed tomography (CT) imaging is difficult due to the persistent breakdown of the machine. Access to basic laboratory results (full blood count; urea, electrolytes, creatinine; liver function test; and blood sugar level) is relatively easy and quick, though the hospital at times lacks the reagents for serology testing for HIV, hepatitis B and syphilis.
The other main component of assistance is the initiation (or re-initiation) of audits undertaken in the unit and the continued involvement of the unit in hospital multidisciplinary meetings. The main audits include maternal mortality and ‘near miss’ audits, perinatal mortality audits and caesarean section audits.
In addition to these duties, there is also interaction with various non-governmental organisations within the health sector in Timor-Leste – for example, Bairo Pite clinic and Marie Stopes International – in order to provide assistance in improving the provision of obstetrics and gynaecology care in the community.
Beyond the busy work schedule, there is the possibility to enjoy world-class diving, dining at various restaurants (a remnant of the UN presence here) and hiking/walking the many tracks along the beach and hills surrounding Dili. Visits to the regional towns – such as Baucau and Balibo – and Atauro Island also make for a nice weekend getaway from the busy schedule of the hospital.

Members of the RACS team at HNGV.
Timor-Leste is a safe and friendly place a stone’s throw from Australia’s northern border and a great first step for anyone considering gaining experience in developing world O&G. Overall, the RACS O&G position at HNGV is an enjoyable, but demanding, job that goes far beyond the postgraduate teaching role that was initially envisaged. There is significant need for care that allows exposure not often seen in many developed countries and the opportunity to be able to not only provide a valuable service to the community, but also the ability to continually learn and develop one’s capacity in this exciting and practical field.
As I complete my assignment in June, the 12-month position is now being advertised for July 2016. I am happy to provide further information on the role and can be contacted via RANZCOG.

The walk up to the ‘Cristo Rei’ statue is rewarding for the views it provides from the top.






Leave a Reply